1. Background
Breast cancer is the most prevalent malignancy among women (1, 2). Timely and proper diagnosis of breast malignancies is of critical importance. In general, masses with cystic and solid components, irregular contour, micro-calcification, or other non-reassuring findings on B-mode ultrasound examination are considered potentially malignant and planned to be biopsied. Doppler ultrasound (including color and spectral methods) can help to differentiate benign masses from malignant tumors. This technique may obviate the need for biopsy in some suspicious lesions (3-9).
Color Doppler can recognize neovascularization, which may be used as a clue for detecting malignant lesions (5-10). The findings of color Doppler studies, however, may be overlapped in highly vascular benign masses and malignant neoplasms (11). This overlap makes it difficult to differentiate malignant tumors from benign masses just based on color Doppler features. However, it seems that the combination of B-mode ultrasound and Doppler study may increase the sensitivity and specificity of ultrasound examination for detecting breast masses with high probability of malignancy. In addition, awareness of the vascularization status of the lesion is valuable for making decision upon performing neoadjuvant chemotherapy, and monitoring response to the treatment (12).
Currently, spectral Doppler parameters are not considered in many imaging centers as a part of routine breast ultrasound examination in the daily practice. The investigations on the applications of spectral Doppler for breast mass evaluation are limited, and entail inconsistent results. The aim of this study was to assess whether the features of breast masses on spectral Doppler examination may help identify the nature of the lesion as well as to determine the optimal cut-off points for each spectral index.
2. Methods
2.1. Approvals
The research proposal was approved by “Institutional Review Board” and “Research Ethics Committee” of Shahid Beheshti University of Medical Sciences, Tehran, Iran. In addition, informed consent was obtained from all participants.
2.2. Study Design
This analytic cross sectional (diagnostic) study was conducted on 100 consecutive women with breast masses that were nominated to undergo core-needle biopsy. The patients were included in the study prospectively with convenience sampling during 12 months (from February 2014 to February 2015). The exclusion criteria were the patient unwillingness and loss of follow-up. The mean age of patients was 45.02 ± 11.88 years (range: 20 - 81 years).
2.3. Data Recording
The findings of B-mode ultrasound (size, margin, content, and echopattern of masses) were recorded according to the breast imaging-reporting and data system (BI-RADS) for mammography and ultrasound (2013 updated version, 5th edition). Color and spectral Doppler features (the presence or absence of blood flow, central or peripheral distribution of flow, resistive index [RI], pulsatility index [PI], and peak systolic velocity [PSV]) were also recorded for each patient. The color Doppler study was optimized by modifying ultrasound machine settings for each individual patient, and spectral Doppler parameters were obtained via manual tracing of 1 to 3 contiguous recorded waveforms.
All examinations and measurements were performed by a radiologist with 15 years of experience in breast imaging in a tertiary care referral center (Mahdieh Women’s Hospital, Tehran, Iran) just before core-needle biopsy of the mass. All of the patients were examined, utilizing a 5- to 9-MHz linear array transducer (Accuvix V10, Samsung-Medison, Seoul, Korea).
Histopathologic results were considered as the gold-standard for classifying masses into benign and malignant groups.
2.4. Statistical Analysis
For statistical analysis, the software SPSS version 20.0 for windows (SPSS Inc., Chicago, IL) was used. The results were presented as mean ± standard deviation (SD) for quantitative variables, and summarized by absolute frequencies as percentages for categorical variables. Continuous variables were compared using t test or non-parametric Mann-Whitney U test. Categorical variables were compared, using Chi-square test or Fisher's exact test. P-values of 0.05 or less were considered statistically significant.
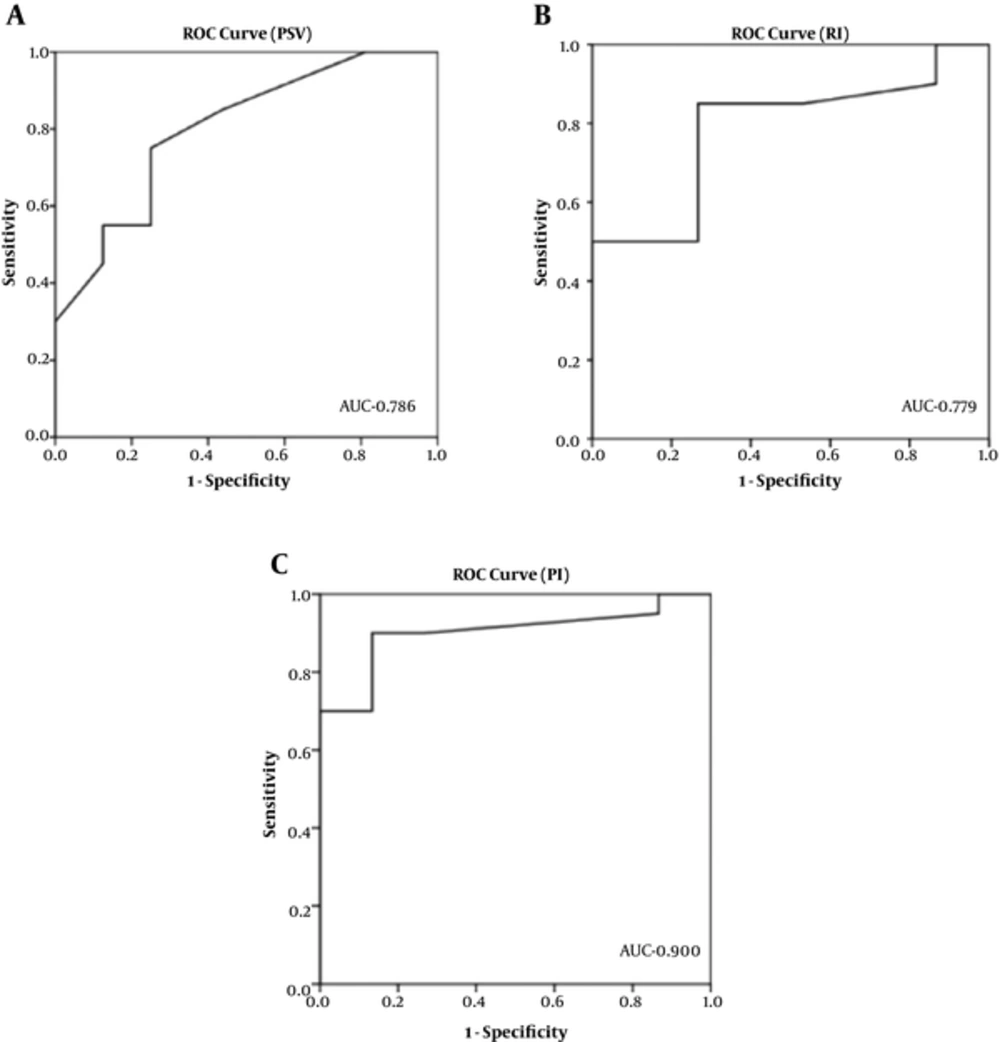
Receiver operating characteristic (ROC) curve was used to identify the optimal cut-off points for PSV, RI, and PI to discriminate malignant from benign masses with the highest sensitivity and specificity.
3. Results
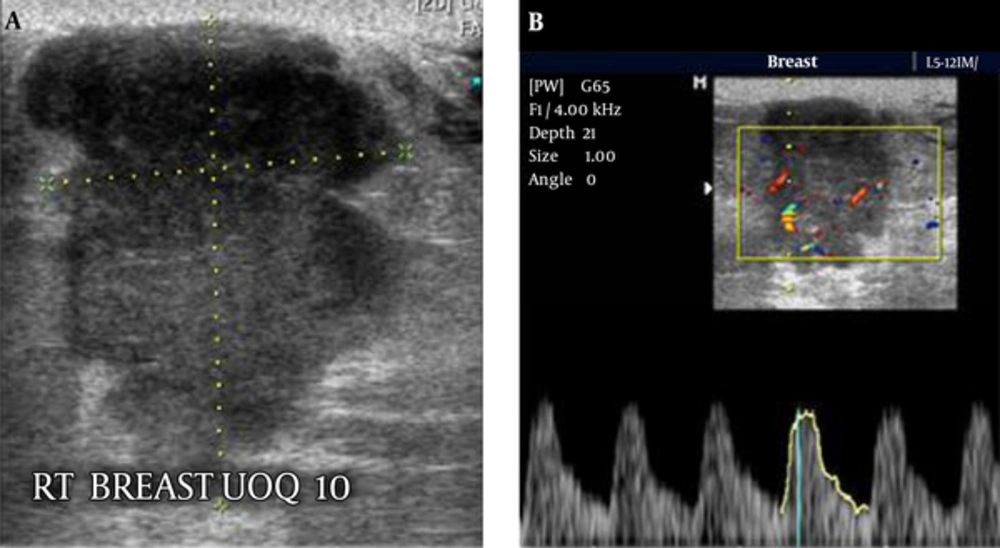
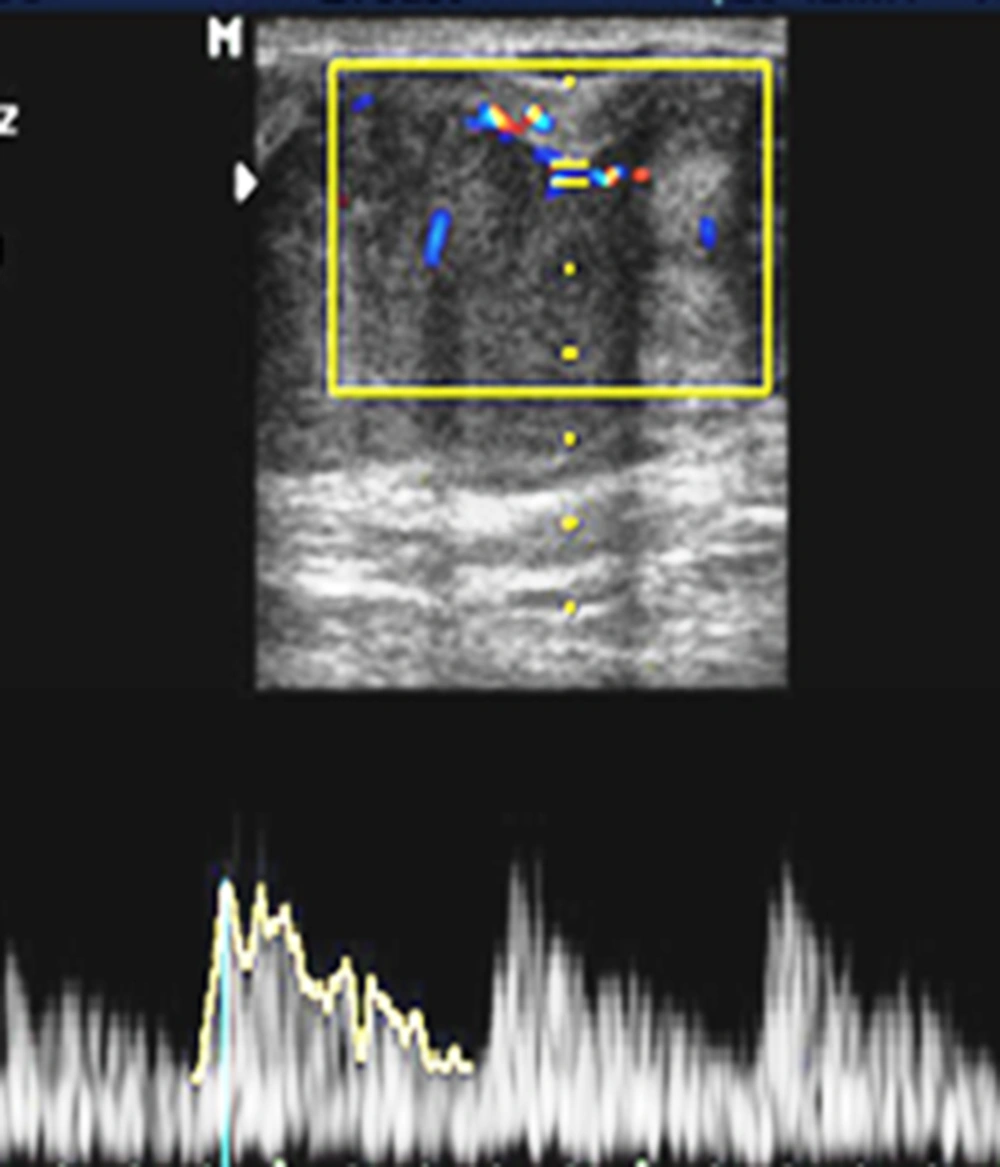
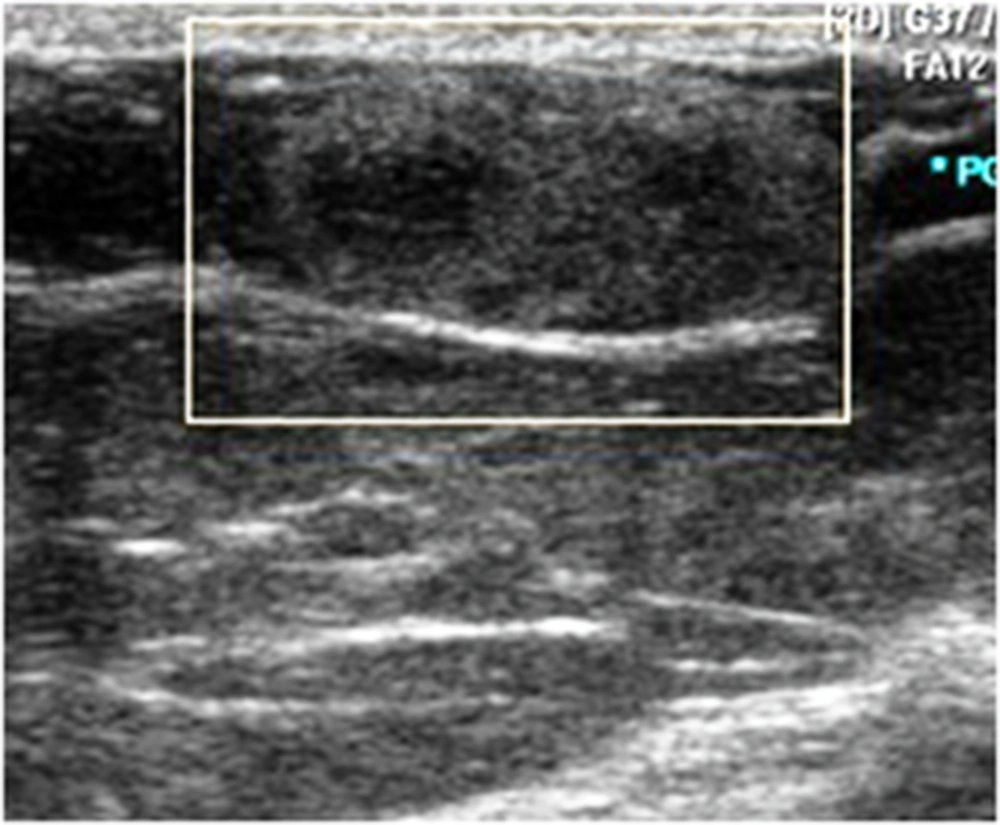
The comparison of B-mode and Doppler ultrasound findings of benign and malignant masses is summarized in Table 1 and some sample ultrasound images are shown in Figures 1 to 3 .
| Ultrasonographic Feature | Benign | Malignant | P Value |
|---|---|---|---|
| Size, mm | 17.05 ± 4.80 | 24.67 ± 9.03 | < 0.001 |
| Component | 0.017 | ||
| Solid | 63 | 85.7 | |
| Solid-cystic | 37 | 14.3 | |
| Margin | < 0.001 | ||
| Circumscribed | 71 | 8.6 | |
| Not-circumscribed | 29 | 91.4 | |
| Echogenicity | < 0.001 | ||
| Hypo-echo | 80 | 42.8 | |
| Mixed-echo | 20 | 57.2 | |
| Flow | < 0.0001 | ||
| Present | 21.5 | 74.3 | |
| Absent | 78.5 | 25.6 | |
| Flow pattern (If present) | < 0.001 | ||
| Peripheral (Rim) | 78.5 | 46.2 | |
| Central (Internal) | 21.5 | 53.8 | |
| PSV, cm/s | 11.69 ± 3.30 | 18.90 ± 10.40 | 0.012 |
| RI | 0.63 ± 0.07 | 0.73 ± 0.09 | 0.001 |
| PI | 0.90 ± 0.40 | 1.09 ± 0.20 | 0.001 |
Abbreviations: PI, pulsatility index; RI, resistive index; PSV, peak systolic velocity.
aValues are expressed as mean ± SD or %.
Invasive ductal carcinoma. A, B-mode ultrasound reveals a large lobulated mixed-echo mass in the right breast of a 60-year-old woman; B, On color Doppler study, the mass shows mainly peripheral flow. Spectral indices were PSV = 24 cm/s, RI = 0.8, and PI = 1.2. PSV, peak systolic velocity; RI, resistive index; PI, pulsatility index.
3.1. Histopathologic Results
According to the histopathologic examinations, 65 patients had benign and 35 patients had malignant breast masses. Malignant lesions were invasive ductal carcinoma (n = 25), ductal carcinoma in situ (n = 8), and invasive lobular carcinoma (n = 2) histologically. Benign masses included fibrocystic changes (n = 22), sclerosing adenosis (n = 14), fibroadenoma (n = 10), nonspecific adipose tissue (n = 10), mastitis (n = 4), lactation-related changes (n = 4), and intramammary lymph node (n = 1).
3.2. B-Mode Ultrasound
The comparison of B-mode ultrasound findings revealed that solid-cystic component, not-circumscribed margin, and mixed echogenicity were significantly more common in malignant tumors compared to the benign lesions (Table 1).
3.3. Color Doppler Study
On color Doppler study, 74.3% of malignant tumors showed detectable flow, while blood flow was seen in 21.5% of benign lesions (P < 0.0001). The flow pattern was mainly central (i.e., internal vascularity) in malignant tumors, and peripheral (i.e., vessels in rim) in benign masses (P< 0.001).
3.4. Spectral Doppler study
On spectral analysis, the mean PSV was significantly higher in malignant masses compared to the benign lesions (18.90 ± 10.40 cm/s versus 11.69 ± 3.30 cm/s; P = 0.012). Similarly, the mean RI (0.73 ± 0.09 versus 0.63 ± 0.07; P = 0.001), and the mean PI (1.09 ± 0.20 versus 0.9 ± 0.04; P = 0.001) were significantly higher in malignant tumors.
To determine the diagnostic accuracy of spectral Doppler indices for differentiating malignant tumors from benign lesions, we found that all 3 indices, i.e. PSV (AUC = 0.786), RI (AUC = 0.779), and PI (AUC = 0.900), were highly capable to distinguish malignant from benign lesions (Figure 4). The optimal cut-off points for PSV, RI, and PI were 12.5 cm/s (sensitivity = 75%, and specificity = 71.4%), 0.68 (sensitivity = 85%, and specificity = 71.4%), and 0.93 (sensitivity = 90%, and specificity = 85.7%), respectively.
4. Discussion
In the present study, the comparison of B-mode ultrasound findings between malignant and benign lesions revealed that malignant tumors were much larger. In addition, the main characteristics of malignant tumors included not-circumscribed margin, solid-cystic component, and mixed echogenicity. These findings are consistent with previous studies (1-3, 11).
Color Doppler helps to detect neovascularization in malignant tumors and may help to distinguish them from benign breast masses (5-10). In the present study, hypervascularity and detectable flow were more common in the malignant lesions. Similarly, in a study conducted by Grischke et al. central blood flow was detectable in 71% and 6.6% of malignant and benign breast masses, respectively (8). The positive predictive value (PPV) for malignancy detection based on the combination of breast B-mode ultrasound findings and color Doppler patterns was reported 92% (9). A lesion vascularization status can be an indicator of malignant potential, metastasis potential, and invasiveness. Moreover, it may provide information about response to treatment and prognosis. Lee et al. studied 52 malignant tumors and 32 benign breast lesions, and found that the presence of high-flow in the early stages of breast tumor is associated with the higher probability of metastasis to the axillary lymph-nodes (5). It was classically thought that malignant breast tumors have stronger color Doppler signals compared to benign lesions (13, 14). However, subsequent studies showed that this is not always true. In general, vascularization is increased in high-grade high-cellular malignant tumors, which have special feeding vessels helping them grow and invade, while low-grade malignant tumors may have no detectable vascularity on color Doppler examination (11, 12). On the other hand, some studies have reported that there is an overlap in color Doppler findings of hypervascular benign masses and malignant tumors (11). This is not unusual, and makes it difficult to differentiate malignant tumors from benign lesions just based on color Doppler pattern. However, it seems that the combination of B-mode ultrasound and color Doppler findings can increase the sensitivity and specificity of ultrasound examination for determining the nature of breast tumors (12).
In this study, the mean values of PSV, RI, and PI were significantly higher in malignant tumors compared to benign lesions. In addition, all of these indices, particularly PI, had high sensitivity and specificity for differentiating malignancies from benign lesions. The findings of this study are similar to some previous studies. For example, Chao et al. reported that PSV, RI, and PI are higher in carcinomas; however, unlike our investigation, they did not find any cut-off point to distinct benign and malignant tumors according to these characteristics (3). Studying on 70 breast masses, Stanzani et al. demonstrated that RI ≥ 0.73 is significantly predictive of malignancy (15). Grischke et al. demonstrated that the presence of blood flow in tumors is a highly specific finding (specificity: 93%) for differentiating malignant from benign breast masses. Other Doppler parameters (such as RI ≥ 0.80) minimally increased the specificity. In their study, sensitivity, specificity, and positive predictive value of Doppler examination to detect malignant breast tumors were 80%, 90%, and 93%, respectively (8).
4.1. Conclusions
In this study, we aimed at investigating the diagnostic accuracy of spectral Doppler ultrasound to determine the malignant potential of breast masses.
In conclusion, although we cannot reliably categorize a breast mass as malignant or benign only based on Doppler ultrasound, this study emphasizes that color and spectral Doppler entail additive information to B-mode ultrasound examination in order to suspect breast malignancies.
4.2. Clinical Practice Points
It was stated earlier that the blood flow pattern in breast malignant lesions is usually central (within the mass) rather than peripheral (around the mass). However, spectral Doppler indices like PSV, RI, and PI may add accuracy to suspect breast malignancies. In the present study, we investigated these indices and determined the reliable cut-off point for each one. The application of spectral Doppler besides the B-mode and color Doppler ultrasound examination may be beneficial in detecting potentially malignant tumors with higher confidence. It may prevent some unnecessary biopsies, and also can guide the treatment strategies in the future.