1. Background
Breast cancer (BC) is one of the most public health issues in Iran and worldwide (1-3). In low and middle income countries, its growth rate was up to 5% per year (4).
In Iran, BC is known as the most common cancer in women after skin cancer (5, 6). The Iran Ministry of Health estimated that the incidence of breast cancer in women was 22 per 100 000 and the prevalence in this same population was 120 per 100 000 (7). In recent review, 65.5% to 70.5% of breast cancer cases were in the early stages (1 and 2) and less than 30% were in the advanced stages in Iran (3).
In recent decades, death rate from breast cancer has been decreasing (8), which is resulted from earlier detection by screening and progressing awareness of people about its signs and symptoms. So, one of the most important strategies in alleviating breast cancer mortality is screening in order to earlier detection (9).
Using guidelines for the early detection of breast cancer can raise the chances of breast cancer diagnosis at an early stage and its successful treatment (10, 11). In addition, the evidence shows that women have limited knowledge about BC warning signs, risk factors, and screening programs (12).
In health care system of Iran, general physicians, who are responsible for a defined population with close contact with people, have an important role in implementing the breast cancer screening as one of the health ministry high priority programs.
2. Objectives
The objectives of this study were to find the amount of knowledge, and awareness in general physicians with regard to BC and its screening tests, in order to implement effective interventional programs in future.
3. Methods
This cross sectional study was performed among 200 general physicians (GP) from urban and rural areas from Jun to September 2017 in Hamadan, Iran.
Sampling method was census and contained all GPs, who contracted as family physicians in Hamadan health center province. All of them were included in our study if they intended to participate and excluded if they spent special educational course period about cancer screening and risk factors.
A self-administered semi-structured questionnaire to take information about sociodemographic characteristics of participants and their knowledge about breast cancer was designed and its content validity was confirmed by an expert group, including an oncologist, 2 community and preventive medicine specialists, and the head of experts in cancer registration unit in Hamadan province health center. After agreement on the questionnaire, the piloting was done on a random sample of 20 physicians. So, the potential problems in the applicability of the tool were assessed.
The first section in questionnaire was included in questions about respondent’s age, sex, location of work (rural or urban area), and the time interval after graduation. And the second part of questions contained participant’s knowledge about breast cancer signs, symptoms, risk factors, and screening programs based on updated guidelines (10, 13, 14).
All the correct responses to each question were given a score of 1 and the wrong answer or ‘don’t know’ response were scored zero, respectively.
In order to determine the relationship between symptoms, risk factors, and screening programs awareness and some variables such as physician’s sex, age, and work experience years, we compute related questions in every domain. So, high score showed high awareness.
The study begun after approval from institute’s ethical committee (ID: IR.UMSHA.REC.1396.393). Consent to participate was obtained from all participant before collecting data.
Chi square test, Mann Whitney U test, and Spearman correlation were performed in data analysis, using SPSS version. 21. Significance level was set at P < 0.05.
4. Results
Among all 200 physicians, who had contract with Hamadan province health center, 150 persons completed questionnaires. All respondent’s characteristics were shown in Table 1.
| Characteristic | Mean ± SD | Range (Max - Min) | No. (%) |
|---|---|---|---|
| Age | 35.47 ± 8.1 | 55 - 25 | |
| Spent years after graduation | 9.4 ± 7.8 | 26 - 1 | |
| Years of work experience | 8.6 ± 7.4 | 26 - 1 | |
| Sex | |||
| Male | 70 (46.7) | ||
| Female | 80 (53.3) | ||
| Practice setting | |||
| Center of province | 36 (24) | ||
| Other districts | 114 (76) |
The mean score of total knowledge on breast cancer screening, risk factors, signs and symptoms for 23 questions was 15.07 ± 2.4 (max: 20 ; min: 9), which meant that correct answers were given to more than half of the questions.
In symptom awareness area, 45.3% of the physicians had correct answer to 4 questions, whereas about risk factor, 61.4% recorded correct answer to 8 questions. The highest knowledge score was related to breast cancer risk factors and the lowest was related to screening programs of breast cancer.
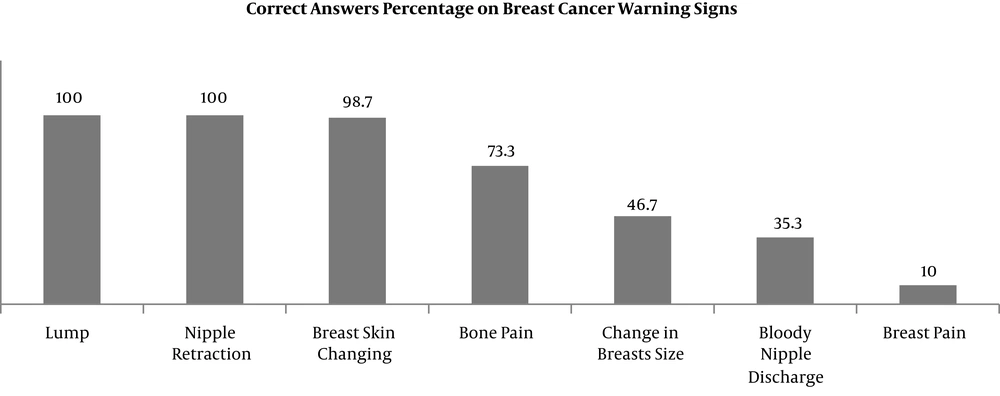
Figure 1 shows that all physicians knew lump and nipple retraction as symptoms of breast cancer also less than half, accounted “change in breast size, bloody nipple discharge, and breast pain” as symptoms (Figure 1).
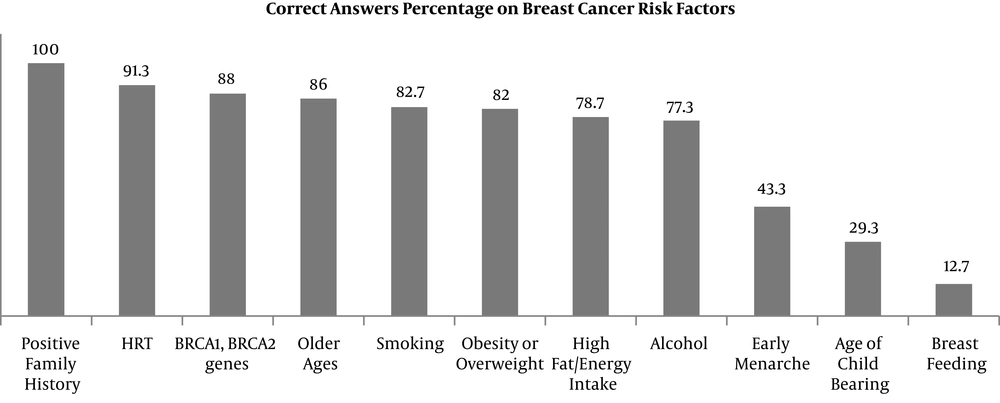
More than 90% of general physicians knew that positive familial history and hormone replacement therapy (HRT) are considered as risk factors of breast cancer, while only 12.7% knew that there is an association between breastfeeding and breast cancer (Figure 2).
Regarding the screening methods, 45.3% of respondents selected correct answers on proper test for screening, 63.3% on appropriate action in positive signs and symptoms, 28% on suitable age for screening, 44.7% on appropriate action in finding breast mass, and 60.7% on screening frequency and interval rules.
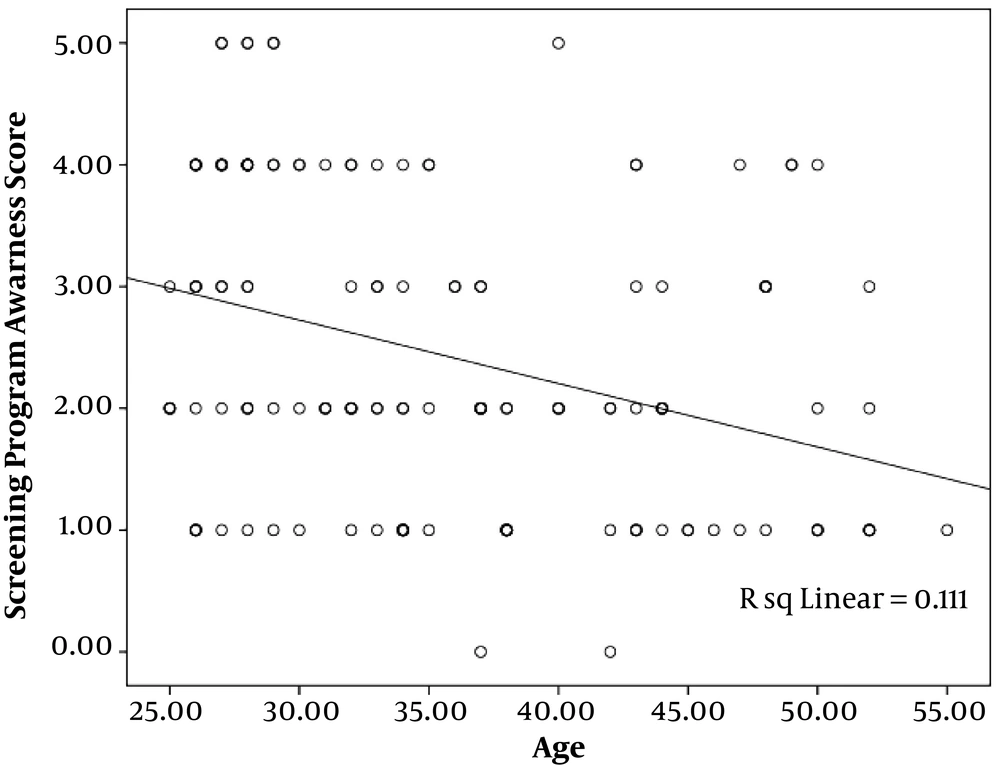
There was a significant reverse correlation between knowledge about screening programs and age of participants (r = -0.3; P < 0.001; Figure 3), and their years of work experience (r = -0.26; P < 0.001). Years of work experience had significant direct correlation with symptom knowledge of physicians as well (r = -0.1; P = 0.02). However, there were no significant difference in relationship between risk factor knowledge and sex, age and years of work experience (Table 2).
| Score | Sex | Age | Work Experience Years | |||
|---|---|---|---|---|---|---|
| Mean ± SD | P Valuea | r | P Value | r | P Value | |
| Symptom knowledge | 0.1 | 0.06 | 0.1 | 0.02 | ||
| Male | 4.6 ± 1.05 | |||||
| Female | 4.67 ± 0.9 | 0.3 | ||||
| Risk factor knowledge | 0.05 | 0.5 | 0.02 | 0.9 | ||
| Male | 8.04 ± 1.3 | |||||
| Female | 7.67 ± 1.6 | 0.2 | ||||
| Screening program knowledge | -0.3 | < 0.001 | -0.26 | < 0.001 | ||
| Male | 2.3 ± 1.3 | |||||
| Female | 2.5 ± 1.2 | 0.4 | ||||
a Mann-Whitney test.
5. Discussion
All health staff and chiefly family physician’s whom women may approach first, must be able to distinguish the risk factors, signs and symptoms, and screening programs of early cancer and must be able to refer patients for further diagnosis and treatment. So, their knowledge, attitude, and practices can predict the early diagnosis in communities (15).
The current study was performed on all family physicians in Hamadan province of Iran. It was observed that correct knowledge and its mean score about all the screening programs of breast cancer was very low and it was lower than median. In addition, there was a significant inverse correlation between screening programs knowledge and their ages and years of work experience. However, physicians’ knowledge about breast cancer risk factors was adequate and the most frequent true answers were about “family history” and HRT and the least were about the “effects of breastfeeding” and “age of pregnancy “and “touching a mass” in signs and symptoms questions. These findings about mentioned risk factors and breastfeeding as protective factor were similar to other related studies in Iran (16).
Sabatino et al. in a study on 50 to 75 years old women who had not get screening recently, showed that 70% of these women had not got advised from their physicians to do mammography (17).
Meissne et al. in their study on 10 212 women in 2007 showed that 3 188 women had not received screening programs. They found out that 80% of the women, who had not done screening, had not been advised to do mammography and the problem has been advised for doing the screening; so, women probably did not request mammography by themselves. Among those who did not do screening programs, women of 40 to 49 years, those with lower education or women with lower income were more prevalent. Only a few percent of participants did not have screening due to access problems to health system (18).
In a study conducted by Smith et al. in Canada, 46% of the physicians reported that they routinely prescribe mammography for 40 to 49 years women and 40% believed that there is no necessity to do this. Also, 62% of physicians prescribed mammography if it was demanded from their patient and only 18% of physicians acted exactly like the protocol (19).
Vakili et al. carried out a study in Shiraz in 2010 about acceptance rate of screening programs in over 18 years population. They concluded that screening methods are used very lower than expected in population (20). This lower rate could possibly be justified by lack of information and advised for screening from physicians.
In Montazeri et al.’s study in Iranian women, it was concluded that Iranian women do not have sufficient information and knowledge about breast cancer risk factors and its screening methods and programs (21). In our study, even family physicians did not have sufficient information and knowledge about breast cancer risk factors and its screening methods and programs; although, the question types and contents for physicians and general population is definitely different. It was similar to Babapoor’s findings, in which the physician’s knowledge about breast cancer screening program was in a moderate level.
Findings of the present study emphasize the need to train Iranian physician’s breast cancer screening programs to promote early identification of breast cancer. In a survey in Iran, significant increases in women knowledge about breast cancer were observed (22). Also, these kinds of studies on physicians are not sufficient in our country. Despite screening can lead to overtreatment, it can motivate women to participate in a preventive health strategy.
We recommend that there should be a well-designed health education program to compensate physicians’ knowledge deficits, especially in older ages in order to raise knowledge toward cancer with emphasis on the role of prevention and screening. Probably, implementing breast cancer screening programs in physicians’ training course can be helpful. In addition, it is useful to deliver educational booklets to physicians. Of course, the best method for training them can be issue in future researches.
However, in breast cancer screening, health manager’s decisions and health policy as well as the cultural factors should be considered. Importance of early diagnosis in breast cancer and its high rate in our country are adequate reasons for considering this issue in top of our priorities.
In the current study, family physicians knowledge on breast cancer screening was insufficient. It is strongly recommended that there should be a well-designed health education program to compensate physicians’ knowledge deficits, especially in older ages in order to raise knowledge toward cancer with emphasis on the role of prevention and screening. Importance of early diagnosis in breast cancer and its high rate in our country are adequate reasons for considering this issue in top of our priorities.