1. Background
According to the World Health Organization (WHO) report, more than 25 million people in the world are currently living with cance. More than 18.1 million people get afflicted with this disease, and about 9.6 million die of it. Cancer is the third leading cause of death in Iran. According to the National Comprehensive Cancer Control Program (NCCCP) report, it is estimated that more than 80000 new cases of cancer occur annually in the country, and more than 30000 die out of the disease in Iran (1-3).
Cancer is referred to as the unbridled process of cell division. Blood cancers affect the production and function of blood cells. Most of these cancers begin in the bone marrow where blood is manufactured. Stem cells mature in the bone marrow and develop into three groups of red blood cells (RBCs), white blood cells (WBCs) and platelets (PLTs).
In most blood cancers, the normal stages of development of blood cells are impaired by the uncontrolled growth of abnormal blood cells. Cancer cells inhibit many of the blood functions such as fighting infections and preventing severe bleeding. All in all, the blood cancers are caused by the impairment in the production and maturation of white blood cells (4-7).
Survival analysis is a collection of statistical methods for analyzing the study data at a specific time until the occurrence of the event (8). This branch of statistics is widely used nowadays in various disciplines, including medicine. The unique survival analysis feature is the use of censored data in analysis processes. “Censored” means that some participants of the study may not experience the event-under speculation for one reason or another (9). In survival analysis, nonparametric, semi-parametric, and parametric methods are used for the purpose of the study. In a parametric approach, it is assumed that the survival time follows a particular distribution and based on that distribution, analyses are performed. Among the parametric distributions, the Weibull model is more commonly used because of its uniform risk function. However, this model is not suitable for analyzing data that have a non-niche risk function. Inverse Entezar Weibull model is among the presented distributions (10).
2. Objectives
In the present study, the factors affecting the survival of patients with various types of cancers were investigated using this model.
3. Methods
The data used in this historical cohort study were extracted from the patients’ records of the Taleghani Hospital, Tehran, Iran in the bone marrow transplantation section. The patient record is formed with the patient’s basic information such as sex, age, height, weight and the like. After referring the patient to the hospital due to a variety of blood complaints types, the patient’s medical information are stored in their documents. After evaluating the patients, they receive bone marrow transplantation if necessary. The current study includes information about patients who referred to the hospital during the years 2007 to 2016. The final follow up was conducted by telephone in order to collect the patients’ survival time from March 2015 to August 2016. In the follow up process, if the patients had died, the cause and date of death were recorded, and if the patients were alive, we informed them that they would be invited to a counseling meeting for a more precise re-examination when needed. Regarding patients, the inclusion and exclusion criteria were not defined and all patients were included in the study.
A total of 492 records were registered. The Patients' information data in their records included sex, age, height, weight, blood type, type of disease, WBC, PLT, hemoglobin (HB), body surface (this value is used to determine many measurements in medicine, including the dosage setting and the amount of fluid required), the CD34 antigen, mononuclear cells (Total MNC) cells, the type of transplantation (from oneself and the others), the number of relapses before transplantation, the number of recurrence after transplantation, survival status and survival time by month. In this study, event variable is defined as survival time. The survival time is calculated by the difference between the initial event and the final event. The date of bone marrow transplantation was considered as the initial event and the date of the patients' death was defined as the end event. Since the follow-up of the patients’ survival was carried out by contacting the entered telephone numbers in their relevant form but many telephone numbers were not available, the survival status of this group of patients was monitored by referring to the registration office.
Patients whose deaths were not recorded in registration office were considered as censored data.
The registered types of blood cancers were as follows: multiple myeloma, non-Hodgkin lymphoma, Hodgkin lymphoma, acute myeloid leukemia, anaplastic astrocytom, myelodysplastic syndrome, primitive neuroectodermal tumour, acute lymphoblastic leukemia, and thalassemia. The types of transplantations were from the patient cells and from others. Due to the fact that the information required in this study was collected from patients’ files and these files were prepared for the purpose of this research, there was no ethical issues in this study. This study was conducted after obtaining permission from the Ethics Committee of Shahid Beheshti University of Medical Sciences and presented to the Vice Chancellor of Student and Cultural Affairs of Shahid Beheshti University of Medical Sciences and Bone Marrow Transplantation Department of Taleghani Hospital (code: ir.sbmu.retech.rec.1396.966). In the present study, the Inverse Entezar Weibull is fitted with the blood cancer data; to fit the model and estimate the relevant parameters, SAS9.1.3 and version 2.13.0 of R software were utilized. In order to describe the data, charts were created using SPSS version 22.
4. Results
Among the subjects, 99 (20.1%) died of blood cancer and 393 (79.9%) survived, out of which 45% (18%) were female and 55% (22%) male. The incidence of mortality is stated in parentheses for both sexes. The mean age of the patients at the time of diagnosis was 38.17 years with a standard deviation of 14.027 and a range of 2 to 67 years for age. Most patients were less than 40 years old at the time of diagnosis. Of all the patients, 55% (81%) were under 40 years and 45% (79%) were more than 40 years old. The percentage of patients who survived after transplantation is presented in parentheses. Out of all the patients, 34% (14%) were affected by Hodgkin lymphoma, 33% (15%) by multiple myeloma, 13% (24%) by acute myeloid leukemia, 12% (26%) by non-Hodgkin lymphoma, and 8% (32%) by acute lymphoblastic leukemia; values in the parentheses show the degree of fatality of each diagnosis. Transplantation was performed through two methods of “from oneself” and “from someone else”. Eighty percent of all patients had “from someone else” method of transplantation, out of which 81% survived, and the remaining (20%) had “from oneself” method of transplantation, out of which 74% survived.
Sixty three percent (22%) of the patients experienced no relapse before receiving transplantation, 31% (15%) had one, and 4% (32%) experienced two relapses. The fatality rate in each number of the relapses is shown in brackets. Eighty three percent (15%) of the patients had no relapses, 16% (42%) had one, and 1% (60%) had 2 relapses after transplantation. The fatality rate in each number of the relapses occurring after transplantation is shown in brackets. The aforementioned information is presented in Table 1.
| Variable | Values |
|---|---|
| Survival status | |
| Died | 99 (20.1) |
| Survived | 393 (79.9) |
| Sex | |
| Male | 271 (55) |
| Female | 221 (45) |
| Age at transplantation | |
| < 40 | 271 (55) |
| > 40 | 221 (45) |
| Type of disease | |
| Hodgkin lymphoma | 167 (34) |
| Multiple myeloma | 162 (33) |
| Acute myeloid leukemia | 65 (13) |
| Non-Hodgkin lymphoma | 59 (12) |
| Acute lymphoblastic leukemia | 39 (8) |
| Type of transplantation | |
| Autologous | 98 (20) |
| Allogeneic | 394 (80) |
| Number of relapses before transplantation | |
| Zero | 319 (65) |
| Once | 153 (31) |
| Twice | 20 (4) |
| Number of recurrences after transplantation | |
| Zero | 408 (83) |
| Once | 79 (16) |
| Twice | 5 (1) |
aValues are expressed as No. (%).
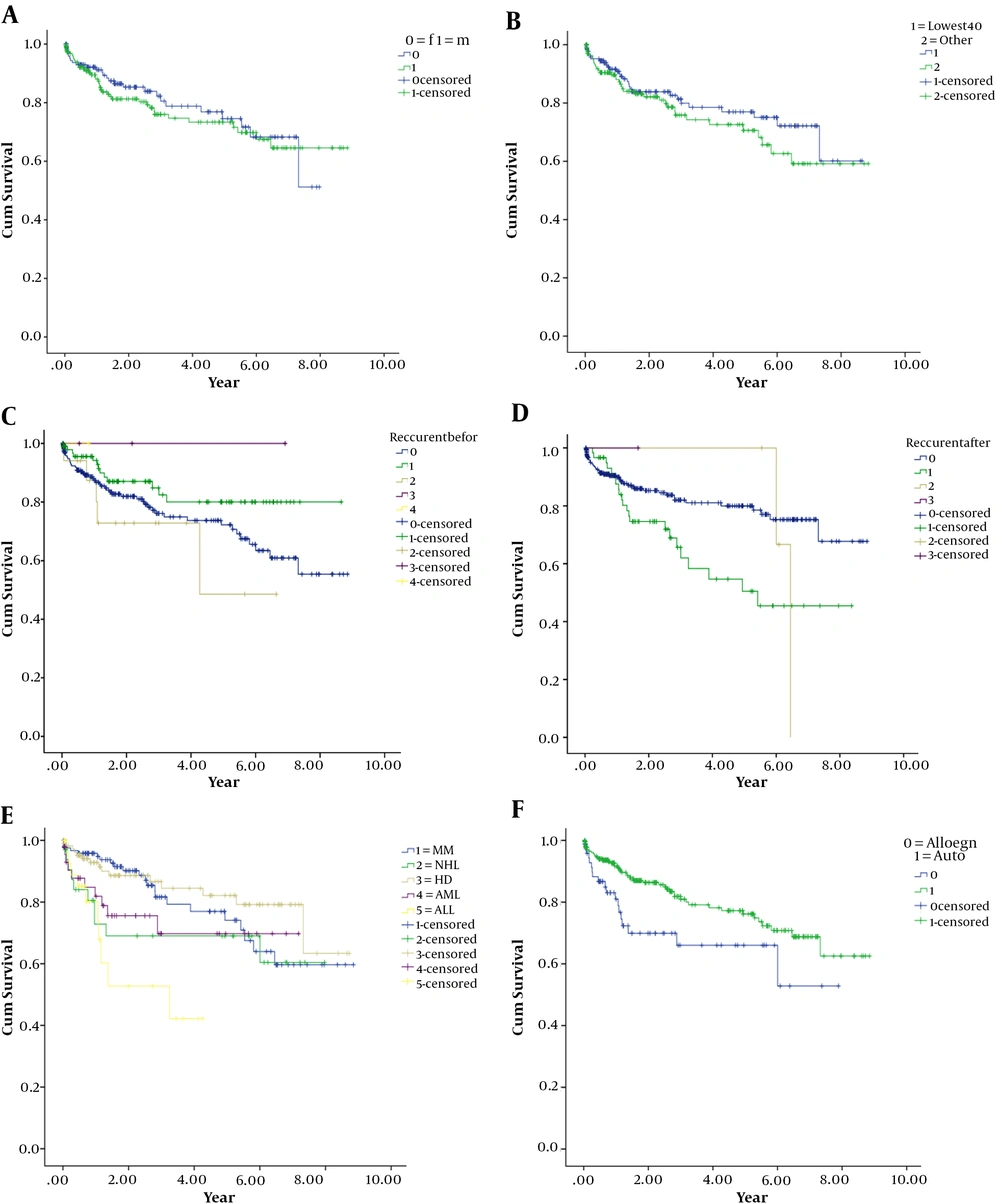
Table 2 shows the distribution frequency of patients based on some variables in the study. Figure 1 illustrates Kaplan Mayer’s charts by distinguishing the levels of used variables in the research. After fitting the Inverse Entezar Weibull parametric model with gender variables, age at the time of transplantation, the number of relapses before transplantation, type of transplantation, and the type of diagnosis and parameters estimation, the results are summarized in Table 3. Based on the results, age variables at the time of transplantation, the type of diagnosis, and the number of relapses before transplantation have a meaningful relationship with the survival of patients with all types of blood cancers (P < 0.05).
| Variable | Minimum | Maximum | Values |
|---|---|---|---|
| WBC | 200 | 129000 | 6602.6 ± 8215.9 |
| HB | 1.7 | 15.8 | 9.52 ± 1.38 |
| PIT | 3000 | 381000 | 61700 ± 56004.6 |
| BSAb | 0.225 | 6.033 | 3.34 ± 0.83 |
| CD34 antigen | 0.1 | 87.03 | 2.57 ± 7.66 |
| Total MNC | 0.2 | 36.39 | 6.28 ± 2.58 |
Abbriviations: BSA, body surface; HB, hemoglobin; MNC, mononuclear cells; PIT, platelet; WBC, white blood cell.
aValues are expressed as mean ± SD.
bBody surface (m2) = √([height (cm) × weight (kg)]) / 3600)
| Variable | Estimate | SE | P Value |
|---|---|---|---|
| Sex | |||
| Male | -0.005 | 0.127 | 0.97 |
| Femalea | - | - | - |
| Age at transplantation, y | -0.013 | 0.006 | 0.034 |
| Type of transplantation | |||
| Autologous | -0.007 | 0.25 | 0.98 |
| Allogeneica | - | - | - |
| Number of relapses before transplantation | -0.24 | 0.11 | 0.031 |
| Type of disease | |||
| Hodgkin lymphoma | 0.448 | 0.262 | 0.087 |
| Multiple myeloma | 0.687 | 0.294 | 0.01 |
| Acute myeloid leukemia | 0.18 | 0.04 | <0.001 |
| Non-Hodgkin lymphoma | 0.163 | 0.291 | 0.576 |
| Acute lymphoblastic leukemiaa | - | - | - |
aRepresents the reference category.
5. Discussion
Due to the importance of cancer as the principal health problem in Iran and the increasing rate of blood cancer mortality among Iranians, the present study was performed to assess the survival rate of patients with blood cancer who received bone marrow transplantation (1, 8, 9, 11-15). A total of 492 patients with a variety of blood cancers who received bone marrow transplantation between 2007 and 2016 were examined, using Inverse Entezar Weibull parametric model. Based on the results of this study, the effect of sex on the survival of patients was not significant. The findings of the present study were not in line with the studies carried out by Arcese et al., Mousavi et al., and Tahmasebi et al. (1, 16-25).
According to Figure 1A, the survival rate of female patients in this study is somewhat higher than that of male patients in some instances; however, this difference was not considered as statistically significant. According to the findings of this study, age was considered as a significant variable. Othus et al., Huebsch et al., and Youbi et al. also considered the age variable relevant to the patient survival in their study, which proved to be in line with the findings of the present study (26-28). Similarly, in a study conducted by Kent et al. (29) in 2009, adolescent and adult patients with blood cancer had lower survival rates compared with children. In general, despite the differences in the survival rate of different age groups, in the age group of adolescents and youngsters aged 15 - 29, improved survival rate was observed (30-41). According to this model, the number of relapses before receiving transplantation and the type of diagnosis were also significantly associated with survival of the patients. In the other study by Arcese et al. (17), “the number of relapses of patients after transplantation” was introduced as a significant factor. The “type of diagnosis” was introduced as a significant variable in the other study which was performed in California School of Bone Marrow Transplantation, and was in accordance with the findings of the present study (28).
In this study, for the first time, the survival of patients with blood cancers has been studied, using a parametric model (Inverse Entezar Weibull) in the presence of independent variables and censored data, which is the strength of the study. The incomplete information in some files was one of the limitations of this study. In addition, uncertainty about the survival of some patients resulted in their elimination.
In conclusion, based on the findings of this study, the parametric models are suggested to be used in the analysis of survival time due to the importance of cancer patients’ survival rate.
5.1. Conclusions
This study showed that factors of age at the time of diagnosis, number of relapses before the bone marrow transplant, and the type of diagnosis are the effective elements in the survival of patients with blood cancer.