1. Introduction
Prostate cancer, an adenocarcinoma, is the second most common cause of cancer deaths among men. Anxiety, stress, pain and sleep disorders are the side effects of cancer, which can affect the patients’ quality of life. Androgen deprivation therapy is the main treatment in the hormonal-sensitive metastatic prostate (1). The psychological consequences of cancer can be exacerbated in patients undergoing new hormonal therapies, especially androgen deprivation therapy (ADT).
In addition, fatigue is a common side effect among patients with cancer (2). Increased fatigue has been observed in patients with prostate cancer who are undergoing new hormonal treatments, especially androgen deprivation therapy (3). Significant decrease in the serum level of testosterone resulted from ADT causes many side effects such as cognitive impairment, sexual dysfunction, fatigue, and poor sleep quality, which can reduce quality of life (4). Further Patients with prostate cancer who undergo ADT are at risk for sleep disorder (5).
There is growing evidence of mindfulness-based cognitive therapy (MBCT) that is considered as a successful and cost-effective intervention for reducing the negative psychological impact of cancer and treatment including the quality of life and depression improving (6). In addition the results of meta-analysis show this effectiveness (7). Cognitive-behavioral therapy (CBT) is considered as a good treatment for chronic fatigue syndrome, however, a small percentage of patients recovered from this therapy therefore, planning new approaches is needed (8).
Furthermore, acceptance and commitment therapy (ACT) is a CBT that one of the main goals of them is increasing the psychosocial flexibility, which can be appropriate for promoting health (9). Research studies have shown that ACT can be effective in improving quality of life (10), pain relief (11), stress and depression (12). According to the findings in Gonzalez-Fernandez and Fernandez-Rodriguez systematic review study (13), ACT is useful in oncologic patients and has improved the emotional state, quality of life and psychosocial flexibility in these patients.
Although several studies have shown the effectiveness of MBCT and ACT independently on psychological indices in cancer patients, no study compares the therapeutic effect of MBCT and ACT in these patients. According to the contradictory findings in this field and also based on the research suggestion of Kim et al. (14) the present study was carried out regarding the importance of fatigue index in predicting the quality of life in male recipients of ADT and the necessity of designing effective interventions in this context.
2. Case Presentation
The present study was an A1B1C1A2B2C2 reversed design with a multiple baseline and a 6-month follow-up (during February to September 2015). A 61-year-old man who had treated with methadone maintenance treatment (MMT), and had received radical prostatectomy for localized prostate cancer two years ago and also was receiving ADT was selected among respondent-driven sampling. The patient received 40 mg Degarelix daily and methadone syrup with a daily dose of 50 mg. He entered to the treatment process while had complaints of fatigue, impulsivity, and sleepless.
At baselines A1 and A2 only evaluation was carried out. In phase B1 and B2 MBCT and ACT were presented. The interval between the two phases of intervention was a six-month follow-up (C1, 2).
MBCT was provided to the subject for three weeks (per sessions 45 minutes). ACT mainly helped to reducing stress and increasing well-being through increased psychosocial flexibility in three weeks (per sessions 45 minutes).
In this study, demographical checklist, the structured clinical interview for DSM-5 (SCID-5), Pittsburgh sleep quality index (PSQI), fatigue severity scale (FSS) and the Connor-Davidson resilience scale (CD-RISC) were used. The evaluation of three indices such as sleep quality, fatigue intensity and resiliency was considered as primary outcomes and the relationship between them was considered as secondary outcomes. The data were analyzed by means of a generalized estimation equation and repeated measures correlation (RMCORR). All stages of this study were carried out after obtaining informed consent from the patient and based on the Declaration of Helsinki (DoH).
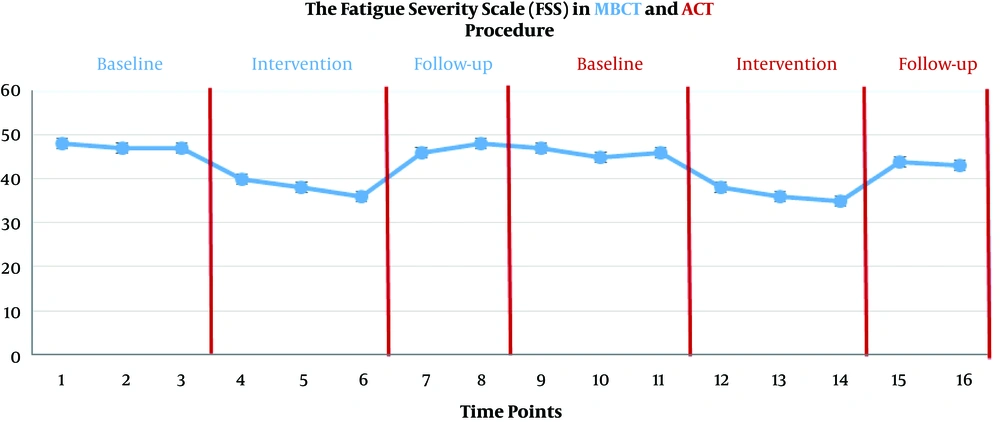
The scores of FSS are presented in Figure 1.
The scores of FSS decreased significantly during the MBCT and ACT (P < 0.01), although this reduction was not maintained at the follow-up stage (P > 0.05).
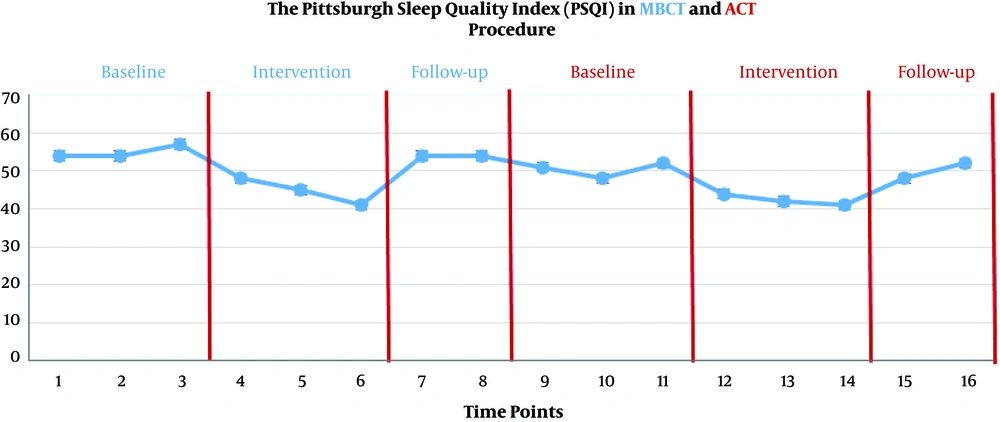
The scores of PSQI during the baselines (A1, 2), MBCT (B1) and ACT (B2), and follow-up assessments (C1, 2) are presented in Figure 2.
The scores of PSQI decreased significantly during the MBCT (B1) and ACT (B2) (P < 0.01), although this reduction was not maintained at the follow-up stage (P > 0.05). In addition, the scores of resiliency scale decreased significantly during the MBCT (B1) and ACT (B2) (P < 0.01), although this reduction was not maintained at the follow-up stage (P > 0.05).
Repeated measures correlation test (RMCORR) was used to determine the relationship between the FSS, PSQI and CD-RISC. The results showed a significant negative relationship.
rrm (1, FSS - PSQI) = -0.67, 95% CI [-0.79, -0.55], P < 0.001
rrm (1, FSS - CD-RISC) = -0.72, 95% CI [-0.83, -0.61], P < 0.001
3. Discussion
The present study is the first study in comparing the effectiveness of MBCT and ACT on the FSS, improvement in PSQI and CD-RISC in a patient with prostate cancer. The primary outcomes showed that both MBCT and ACT were effective on FSS, PSQI, and CD-RISC; however, these changes did not persist until the follow-up stage. Secondary outcomes also showed that there is an inverse relationship between the FSS and PSQI and the CD-RISC. Although a similar study has not been done so far, Haller et al. (7) checked out the effectiveness of these two treatments on the psychological indices in cancer patients. Along with the results of this study, they (7) showed that the use of MBCT in breast cancer patients was associated with a short-term effect on fatigue, sleep and stress indices, although only changes in stress remained persistent in a six-month follow-up. In this regard, in another study Park et al. (6) showed that eight sessions of MBCT had a significant effect on psychological status of patients with breast cancer. In addition, according to the results of a study by Lao et al. (15) MBCT increased cognitive flexibility and supra-consciousness. Further, Britton et al. (16) showed that the use of MBCT has been associated with improved PSQI in patients undergoing drug therapy. Along with the results of the present research, Rimes and Wingrove’s study (8) indicated the effectiveness of MBCT on chronic fatigue syndrome. In contrast to the results of this study, based on the effectiveness of MBCT, Chambers et al. (17) pinpointed that this treatment had no significant effect on reduction of distress in men with advanced prostate cancer.
A part of the results of this study showed that ACT was associated with a decrease in the FSS, improvement in PSQI and CD-RISC. In this regard, the results of the Daly-Eichenhardt et al. (18) showed that acceptance and commitment therapy has significantly improved the quality of life and the psychological flexibility. In addition, Jacobsen et al. (19) in their study indicated that ACT reduced fatigue severity in fatigue syndrome patients.
Based on the secondary outcomes of this study there is an inverse relationship between FSS, PSQI and psychosocial flexibility. In this regard, the results of Honn et al. (20) determined that sleep disorders can reduce psychological flexibility by weakening cognitive functions, and there is a significant reverse relationship between the two variables. In contrast with results of this study, there was no significant relationship between psychosocial flexibility and fatigue in the other study by Jacobsen et al. (19).
The results of this study showed the effectiveness of third wave interventions on the psychological indices in the metastatic cancer patient. The use of MBCT and ACT as an affordable and accessible intervention can be accompanied by clinical applications in the field of cancer. However, the results of this study, due to a single-case study, have limited generalizability. A randomized clinical trial in comparing the effectiveness of MBCT and ACT with non-treatment, placebo therapy and other effective treatments in oncology can be a good route for future studies.