1. Background
Although uterine cancer is not ranked among the ten most common cancer types in Iran, it is the 12th most prevalent in women and the third most common cancer of the female genital tract after breast and ovarian cancer. The mortality rate of endometrial cancer in Iran is 0.6 in 100,000 persons. According to the annual report of the Iranian national cancer registry, 1304 new cases were registered in 2014; with a crude incidence rate of 3.43 in 100000 and an age-adjusted incidence rate (ASR) of 3.67 in 100000 (1). Endometrial cancer was the most common malignancy of the female genital tract, with an estimated 63230 new cases in 2018 in the United States (2). In 2017, 67% of endometrial adenocarcinomas were confined to the uterus (stage I) and 21% of patients had locally advanced disease such as cervical/parametrial involvement (3). Following research by Nillof et al. about elevated levels of CA125 in advanced endometrial cancer (4), the interest in evaluating the correlation of this tumor marker with other surgicopathologic and prognostic variables of this cancer increased. Several studies evaluated the correlation of preoperative CA125 in endometrial cancer with depth of myometrial invasion (5), cervical involvement (5-7), stage (6, 8, 9), grade (10), lymphovascular invasion (8), extrauterine and adnexal involvement (6, 7, 9, 11) as well as lymph node metastasis (8-10, 12-14). Some studies evaluated the utility of serum CA125 for follow-up of patients with endometrial cancer in order to detect disease recurrence (5). Some experts have recommended preoperative assessment of CA125 for determining the need for lymphadenectomy in endometrial cancer, which has been a matter of controversy long before (7, 8, 10, 12-14).
The initial preoperative assessments in endometrial cancer are history and physical examination, endometrial biopsy, imaging, considering for genetic evaluation, as well as serum CA125 assay for patients with extrauterine disease (3). Recently, there have been data supporting neoadjuvant radiotherapy and adjuvant extrafascial hysterectomy for locally advanced endometrial cancers (cervical/ parametrial invasion) as an alternative procedure for the former approach which was radical hysterectomy (15). Regarding the National Comprehensive Cancer Network (NCCN) guidelines, two distinct management strategies exist for patients with cervical/parametrial involvement in endometrial cancer: (1) radical hysterectomy and staging followed by adjuvant therapy or (2) adjuvant extrafascial hysterectomy after neoadjuvant radiotherapy (3). However, comparison of radical and extrafascial hysterectomy shows a higher risk of complications such as urinary tract disruption and stricture, infectious morbidity, and gastrointestinal disturbances with the more extensive radical surgery (16, 17). Recommending preoperative CA125 assessment in patients with endometrial cancer, as mentioned in NCCN, is for following the patients, not as an initial staging predictor (3). Therefore, not only the role of serum CA125 in preoperative assessment, treatment plan and the extent of surgery are a matter of controversy; but also its cut-off levels for predicting the extent of the disease, are still in dispute.
2. Objectives
In this study, we investigated the relationship of serum CA125 with the clinicopathologic variables of endometrioid endometrial cancer and evaluated the appropriate cut-off values for predicting the extension of disease to cervical stroma and parametrium in the patients under study.
3. Methods
Pathological and surgical data of 128 patients with endometrial carcinoma who were surgically staged at Imam Hossein Hospital in Tehran from 2011 to 2018 were recorded in a previously-printed questionnaire. The data were obtained from the electronic database of the hospital. Surgical staging included exploratory laparotomy, total abdominal hysterectomy and bilateral salpingo-oophorectomy with or without pelvic and para-aortic lymph node dissection. Some patients were treated by sampling the lymph nodes per surgeon’s direction, especially when specific high risk comorbidities or morbid obesity were present. All the operative procedures were performed by a gynecologic oncologist. Pathologic assessments were performed in the department of pathology in the same hospital with a team of gynecologic oncology experts. Pathological staging was based on the 2017 criteria of the International Federation of Gynecology and Obstetrics (FIGO) system and the histological classification was performed using the criteria of the World Health Organization (WHO), mentioned in NCCN 3.2019 (3).
Forty-six patients with non-endometrioid pathology, un-recorded preoperative CA125 and ovarian involvement were excluded from the study. Patients with ovarian involvement were excluded because of the probable bias in the differentiation of synchronous from metastatic disease. Finally, 82 patients with recorded preoperative CA125 and endometrioid endometrial cancer without adnexal involvement were eligible to participate in this study. Samples for measuring CA125 (u/mL) were taken preoperatively, submitted to the laboratory of the same hospital, and processed using electrochemiluminescent enzyme immunoassay.
Quantitative data were expressed as mean and standard deviation. Descriptive statistics (frequency observations and percentages) were used for qualitative data processing. t-test (similar to non-parametric Mann-Whitney) and univariate ANOVA test were used for correlation assessments. We examined the correlation of preoperative serum CA125 levels with FIGO stage, depth of myometrial invasion, parametrial involvement, cervical stromal involvement, pelvic lymph node metastasis, tumor grade, and lymphovascular invasion. A receiver operating characteristic (ROC) curve was used to determine the optimal preoperative CA125 cut-off value, which could predict with maximum sensitivity and specificity, the cervical stromal and parametrial invasion in endometrioid endometrial cancer. Sensitivity, specificity, predictive values, and likelihood ratios were calculated. Statistical Package for Social Sciences (SPSS; SPSS Inc. Chicago II, USA), version 21 software was used for analysis. A P value < 0.05 was considered as statistically significant.
4. Results
128 patients with endometrial cancer were identified during a seven-year period from 2011 to 2018. Eight cases with adnexal involvement were excluded from the study to eliminate the bias of imprecise diagnosis of synchronous or metastatic ovarian tumor, and 38 cases were excluded due to unrecorded preoperative CA125 or non-endometrioid pathology. Finally, 82 cases with endometrioid endometrial carcinoma were included in this study.
Descriptive statistics: The mean age of participants was 56.5 ± 10.14 years. The number and frequency (percentages) of patients with each surgicopathologic characteristic are shown in Table 1. For 11 (13.4%) and 29 (35.4%) patients, pelvic lymph node dissection and para-aortic node sampling was not performed, respectively, because of comorbidities or morbid obesity. Regarding imaging reports, pelvic/ para-aortic lymph nodes seemed to have been involved in only 1 (1.2%) patient; however, information was missing for 7 (8.5%) cases. The mean tumor size was 3.6 ± 2.7 cm (range: 0.5 - 13 cm).
| Characteristics | No. (%) |
|---|---|
| 2017 FIGO stage | |
| I | 71 (86.6) |
| II | 3 (3.7) |
| III | 6 (7.4) |
| IV | 2 (2.4) |
| WHO grade | |
| 1 | 48 (58.5) |
| 2 | 26 (37.1) |
| 3 | 8 (9.8) |
| Depth of myometrial invasion, % | |
| < 50 | 55 (67.1) |
| ≥ 50 | 27 (32.94) |
| Cervical stromal invasion | |
| Negative | 74 (90.2) |
| Positive | 8 (9.8) |
| Parametrial invasion | |
| Negative | 78 (95.1) |
| Positive | 4 (4.9) |
| Peritoneal cytology | |
| Negative | 78 (95.1) |
| Positive | - |
| Not reported | 4 (4.9) |
| Lymphovascular space invasion | |
| Negative | 77 (93.9) |
| Positive | 5 (6.1) |
| Pelvic lymph node metastasis | |
| Negative | 69 (84.1) |
| Positive | 2 (2.4) |
| Not reported | 11 (13.4) |
| Para-aortic lymph node sampling | |
| Negative | 52 (63.4) |
| Positive | 1 (1.2) |
| Not reported | 29 (35.4) |
Analytical statistics: On univariate analysis (ANOVA), significant correlations between the mean level of preoperative CA125 (u/mL) and tumor grade/FIGO stage were detected. t-test analysis showed significant differences in preoperative CA125 level (u/mL) between involved versus uninvolved groups regarding cervical stromal and pelvic node involvements (P < 0.05). For parametrial involvement, it showed a marginally significant difference (P = 0.058) which could be the result of sample size limitation. However, no statistically significant correlation was detected between lymphovascular and depth of myometrial invasion with preoperative CA125; although the means differed considerably (P > 0.05) (Table 2).
| Surgicopathologic Characteristic | Preoperative CA125, u/mL | P Value |
|---|---|---|
| 2017 FIGO stage | 0.000 | |
| I | 14.94 ± 16.55 | |
| II | 62.26 ± 17.04 | |
| III | 74.94 ± 44.27 | |
| IV | 248.6 ± 98.42 | |
| WHO grade | 0.017 | |
| 1 | 18.61 ± 46.07 | |
| 2 | 41.33 ± 44.57 | |
| 3 | 28.35 ± 31.87 | |
| Depth of myometrial invasion, % | 0.112 | |
| < 50 | 21.23 ± 45.25 | |
| ≥ 50 | 38.02 ± 43.68 | |
| Cervical stromal invasion | 0.000 | |
| Negative | 19.94 ± 30.24 | |
| Positive | 89.83 ± 95.07 | |
| Parametrial invasion | 0.058 | |
| Negative | 22.17 ± 39.38 | |
| Positive | 116/37 ± 63.41 | |
| Lymphovascular involvement | 0.168 | |
| Negative | 25.42 ± 45.85 | |
| Positive | 47.36 ± 28.53 | |
| Pelvic lymph node metastasis | 0.017 | |
| Negative | 21.97 ± 31.77 | |
| Positive | 62.27 ± 7.46 |
aValues are expressed as mean ± SD.
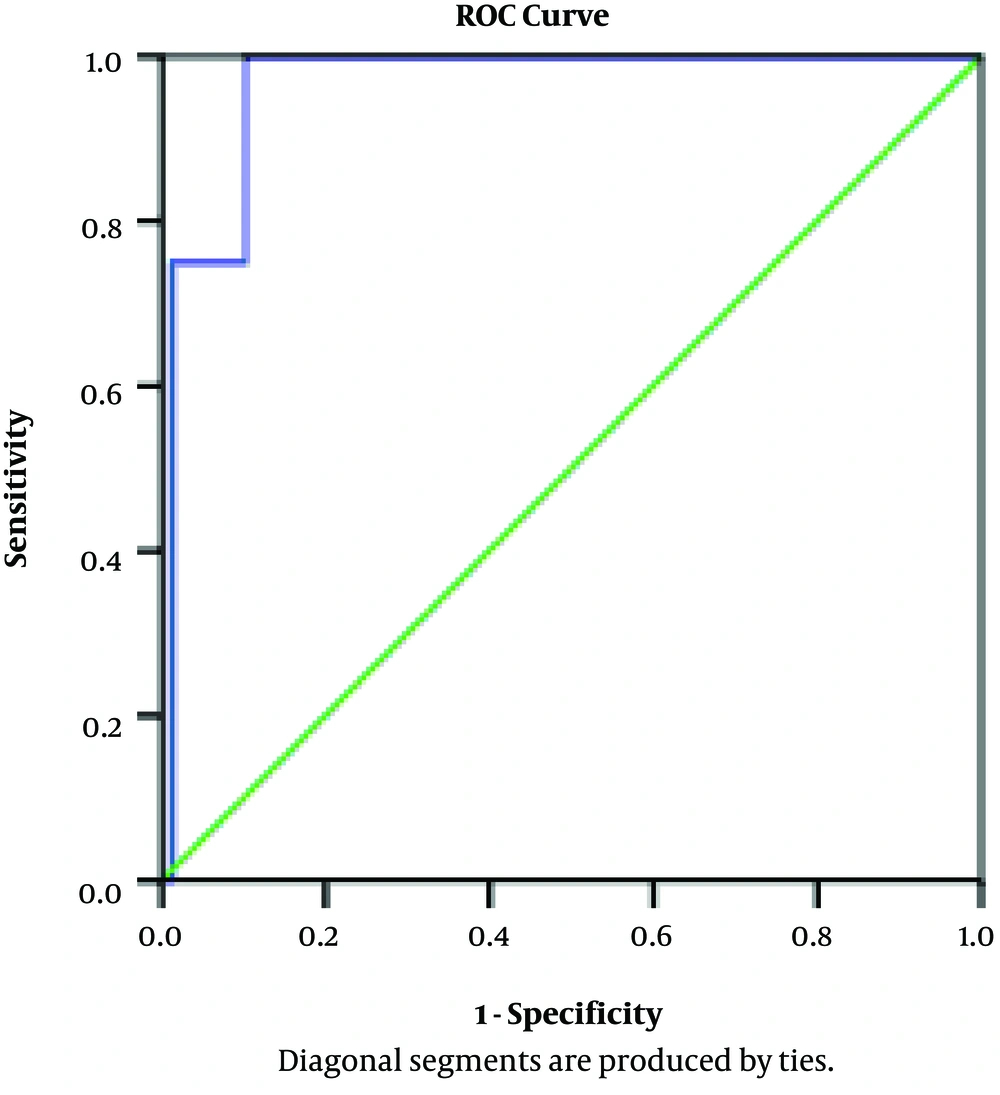
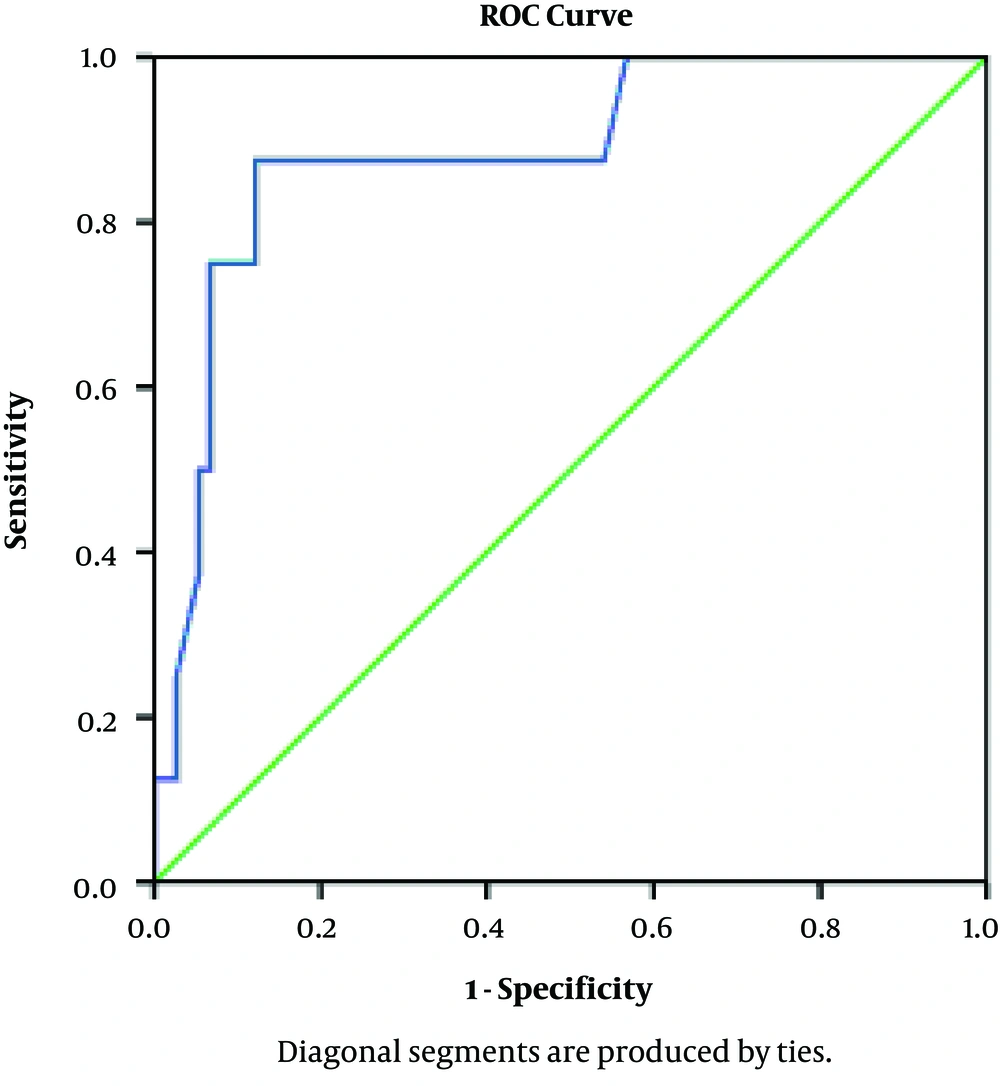
Using the ROC curve, the optimal preoperative CA125 cut-off values for predicting parametrial and cervical stromal invasions in endometrioid endometrial cancer were detected as 45.5 and 41.9 u/mL, respectively (Table 3 and Figures 1 and 2).
| Tumor Characteristic Index | Parametrial Invasion | Cervical Stromal Invasion |
|---|---|---|
| Area under the ROC curve | 0.965 | 0.883 |
| Optimal cut-off value, u/mL | 45.5 | 41.9 |
| Sensitivity, % | 100 | 87.5 |
| Specificity, % | 89 | 87.8 |
| Confidence interval 95% | 0.915 - 1.00 | 0.758 - 1.00 |
| P-value | 0.002 | 0.000 |
| Predictive value (+), % | 33.3 | 43.75 |
| Predictive value (-), % | 100 | 98.48 |
| Likelihood ratio (+) | 9.7 | 7.17 |
| Likelihood ratio (-) | 0 | 0.142 |
5. Discussion
General principles of surgery for endometrioid endometrial cancer are: total abdominal hysterectomy and bilateral salpingo-oophorectomy, with or without pelvic and para-aortic lymph node dissection, peritoneal cytology, and omental biopsy. Nevertheless, the surgical extent could vary with the disease extent; for example, when parametrial or cervical stromal involvement presents, some experts suggest extrafascial hysterectomy after neoadjuvant radiotherapy with or without chemotherapy (15).
Several factors could help predict parametrial or cervical invasion such as preoperative CA125. Cancer antigen (CA) 125 is a glycoprotein secreted from coelomic epithelial structures (such as fallopian tubes, endometrium, and endocervical epithelium). It could be elevated in both benign (endometriosis, pregnancy, and inflammation) and malignant (such as gynecologic, pancreas, and colon cancer) conditions. It is accepted for use in the follow-up of patients with advanced endometrial cancer (4). The cut-off value of CA125 which could predict the extent of the disease is a matter of controversy. Several studies have been performed on this subject, some of which are discussed below.
Considering the study of Hsieh et al. a study from Taiwan on 124 endometrial cancers in 2002, preoperative CA125 > 40u/mL (sensitivity: 77.8%, specificity: 81%) could be predictive of pelvic node involvement (12).
Regarding a study from Japan on 214 endometrial cancers in 2003, the cut-off value of preoperative CA125 which predicted pelvic and para-aortic lymph node metastases was 25 and 40 u/mL, respectively. This study included all endometrial cancer pathologies, not only the endometrioid type (13).
Due to a study by Povolotskaya et al. from England on 95 endometrial cancers in 2014, the proposed CA125 cut-off value to predict lymph node metastases was 28 u/mL (10).
In this study, which was only in patients with endometrioid endometrial cancer, the mean preoperative CA125 in pelvic node-positive cases was 62.27 ± 7.46 u/mL, which showed a weak but significant difference between the positive versus negative group (P = 0.017). However, only two cases had pelvic lymph node involvement, 64 cases had no involvement, and in 11 cases pelvic lymphadenectomy was not performed.
Considering another study from North Carolina on 141 endometrial cancers in 2014, the proposed preoperative CA125 cut-off value to predict higher disease stages (stages III and IV) was 35 u/mL. Various pathologies of endometrial cancer were included in this study (6).
Regarding Espino-Strebel and P. Luna’s study from the Philippines on 90 endometrioid endometrial cancers in 2012, a preoperative CA125 of more than 55 u/mL was a predictor of extrauterine involvement (9).
In our study, the best preoperative CA125 cut-off value for predicting parametrial involvement (stage III) was detected as 45.5 u/mL (sensitivity 100%, specificity 81%, positive predictive value (PPV) 33.3%, negative predictive value (NPV) 100%, area under curve (AUC): 0.965, confidence interval (CI): 0.915 - 1.00, and P value: 0.002).
With regard to Pinar Cilesiz Goksedef’s study from Turkey on 97 endometrioid endometrial cancers in 2010; there were significant correlations between CA125 ≥ 35 u/mL and depth of myometrial invasion/ cervical stromal involvement (5).
In regard to our study, the mean preoperative CA125 in cases with cervical stromal involvement was 89.83 ± 33.61 u/mL. t-test showed a significant difference between cervical stroma involved and uninvolved cases. The cut-off value for predicting cervical stromal invasion with 87.5% sensitivity and 87.8% specificity was 41.9 u/mL (AUC: 0.883, CI: 0.758 - 1.00, P value: 0.000, PPV: 43.75%, and NPV: 98.48%).
Considering Chen et al.’s study from Taiwan on 120 endometrial cancers in 2011, a preoperative CA125 value of 40 u/mL showed significant correlation with a higher grade of the tumor and lymphovascular involvement (8).
Similarly, in our study, univariate analysis (ANOVA) showed a significant association between tumor grade and mean preoperative CA125 (P = 0.017). Nevertheless, comparing preoperative CA125 between lymphovascular involved versus uninvolved groups demonstrated no significant correlation, although the means differed considerably (47.36 versus 25.42 u/mL, respectively) (P value = 0.168).
Based on the study of Modarres-Gilani et al from Iran on 91 cases with endometrial cancer in 2017, in line with our results, high preoperative CA125 was significantly correlated with advanced stage (cut-off value: 20 u/mL) (18). Also, they found a significant correlation between depth of myometrial invasion and CA125 level, but our study did not demonstrate this association.
In Espino-Strebel and P. Luna’s study, there was a weak but significant correlation between CA125 and depth of myometrial invasion (P = 0.02) (9).
The mean preoperative CA125 in the two groups of myometrial involvement (< 50% and ≥ 50%) were 21.33 and 38.02 u/mL, respectively. We found no significant correlation between the two groups, although the means differed considerably (P = 0.112).
5.1. Conclusions
The results of this study, in accordance with other studies, showed that preoperative CA125 in endometrioid endometrial cancer is significantly correlated with the disease stage, grade, pelvic lymph-node metastasis, and cervical stromal involvement. For parametrial involvement, the test was marginally significant, which may be due to the limitation of sample size. Our study showed that the optimal preoperative cut-off values to predict cervical stromal and parametrial involvement are 41.9 and 45.5 u/mL, respectively. We can conclude that in values above this range, the disease would probably be extensive. Other standpoints with parametrial or cervical stromal involvement are the recently proposed methods of treatment which differ from the previous ones. Some experts recommend neoadjuvant radiation with or without chemotherapy followed by extrafascial hysterectomy that has less complications compared to primary surgery. Therefore, by predicting parametrial/ cervical stromal involvement, the primary approach and maybe the final outcome might differ. Regarding this study and also other studies, we recommend routine preoperative CA125 measurement in endometrioid endometrial cancer patients. It would be useful along with physical examination and imaging for considering the disease extent and planning the appropriate therapy.
For future investigations, we recommend comparing the survival of patients in the two groups (primary radical surgery versus adjuvant extrafascial hysterectomy).