1. Introduction
Gagner et al. performed the first laparoscopic adrenalectomy in 1992 (1). Todays, it is usually performed in two minimally invasive approaches: the posterior retroperitoneal and the lateral transabdominal approach. The choice of approach is dependent upon the patient, tumor criteria, and the surgeon’s experience. The lateral transabdominal approach has preference for large tumors, morbidly obese patients, and when malignancy is suspected.
Morbid obesity is an independent risk factor for complications of adrenalectomy such as wound infection and sepsis in postoperative period, and can increase the operation time and risk of conversion of laparoscopy to open procedure. Also, diabetes mellitus can increase wound complications (2).
Recent data show that laparoscopic adrenalectomy can reduce the risk of intraoperative bleeding, recovery time, wound complications, analgesic need, and hospital stay in morbidly obese and diabetic patients (3).
Some investigators explained one stage bariatric surgery and laparoscopic adrenalectomy in morbidly obese patients (4, 5).
In addition to morbid obesity, large liver, big tumors and surgeon’s insufficient experience are factors that can increase the risk of conversion to open surgery (6, 7).
The new advances in imaging tools such as ultrasonography, computed tomography (CT) scan, and magnetic resonance imaging (MRI) have resulted in more accurate diagnosis of adrenal tumors (8).
2. Case Presentation
A 37-year-old morbidly obese diabetic female with body mass index (BMI) = 47 that was candidate for bariatric surgery and had a complaint of right flank pain was the case of this study. In preoperative phase, we found a large complex adrenal mass in her ultrasonography result that was suspected for pheochromocytoma or malignancy.
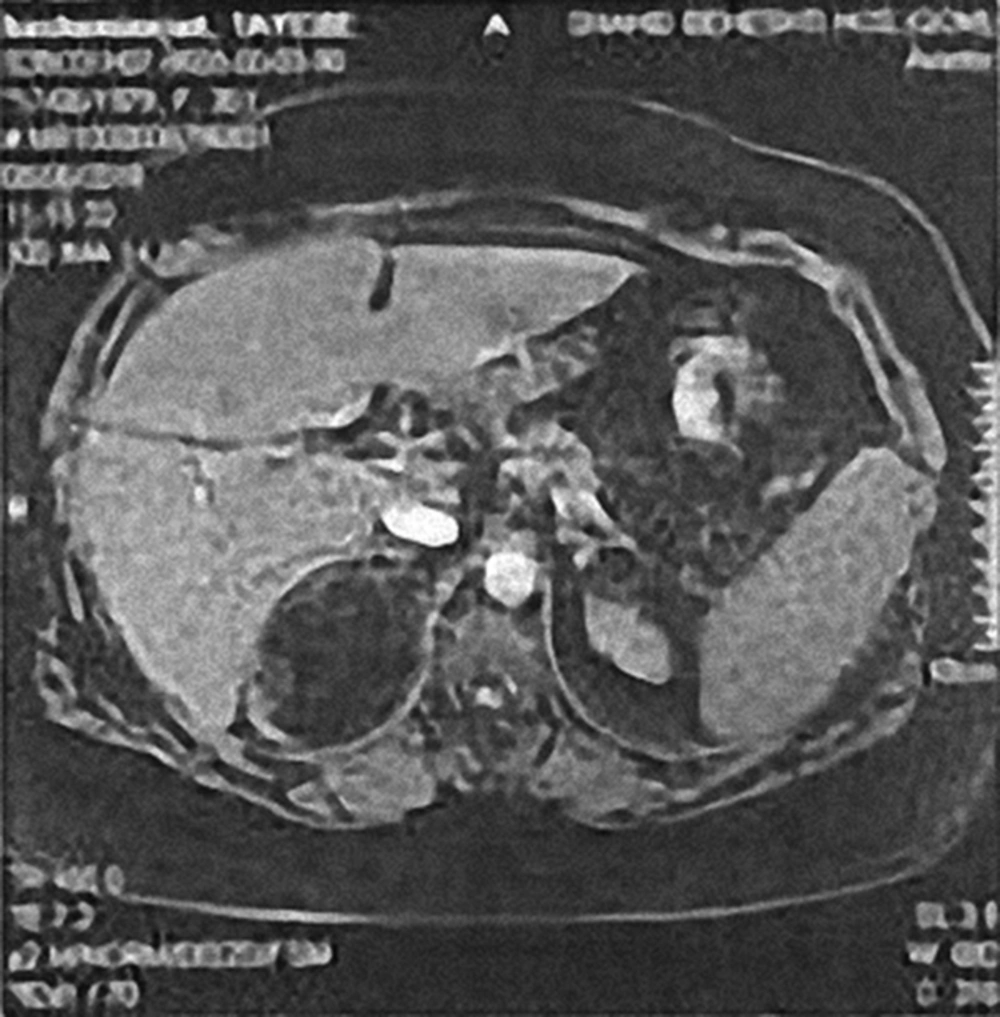
In adrenal T2W MRI, the patient had an 82 × 78 × 55 mm heterogeneous mass in right adrenal gland that was suspected to myelolipoma, pheochromocytoma or malignancy (Figure 1).
In abdominal CT scan, the mass was reported suspicious for malignancy or myelolipoma (Figure 2).
In laboratory findings, we found normal hormonal assay that is listed in Table 1.
| Test | Result | Unit | Normal Ranges |
|---|---|---|---|
| FBS | 341 | mg/dL | 70 - 115 |
| Sodium | 134 | mmol/L | 135 - 145 |
| Potassium | 4.1 | mmol/L | 3.5 - 5.5 |
| Urine 24h/metanephrine | 94.2 | µgr/24h | 0 - 350 |
| Urine 24h/Cr | 504 | mg/24h | 600 - 1800 |
| Cortisol 8 AM | 24.5 | µgr/dL | 5 - 25 |
| Aldosterone (upright) | 61.8 | pg/mL | 25 - 315 |
| ACTH | 15.57 | pg/mL | 4.7 - 48.8 |
Abbreviations: ACTH, Adrenocorticotropic Hormone; Cr, Creatinine; dL, Deciliter; FBS, Fasting Blood Sugar; L, Liter; mg, Milligram; mL, Milliliter; mmol, Milimol; pg, Pictograms; µgr, Micrograms.
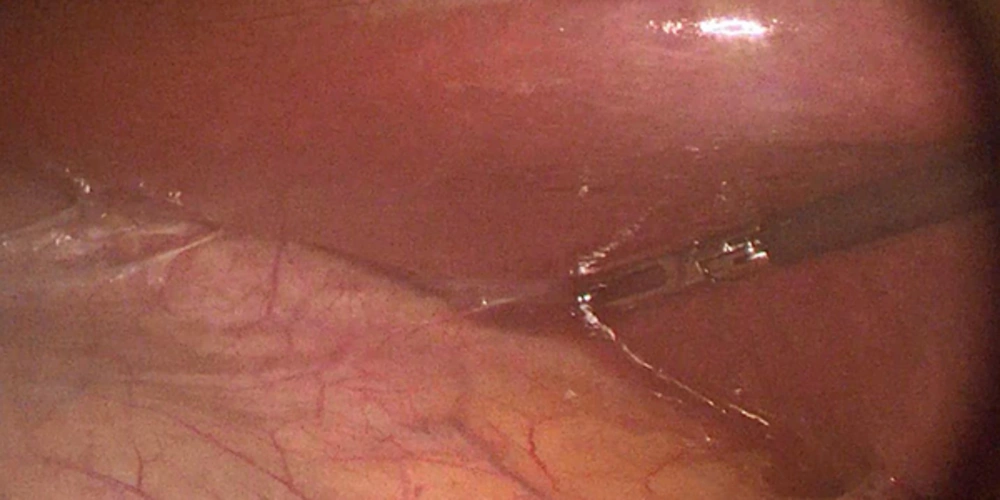
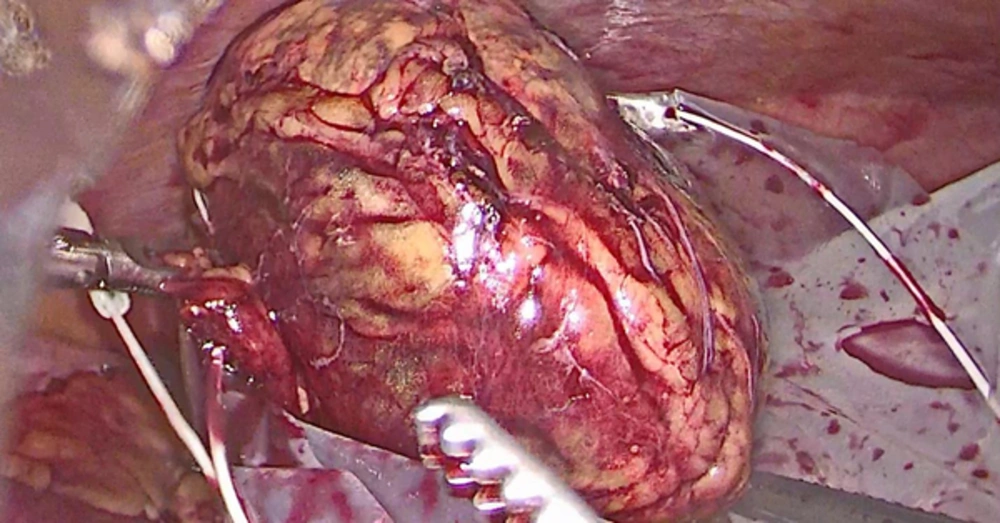
The patient was scheduled for laparoscopic lateral transabdominal adrenalectomy. After intubation, under general anesthesia, in lateral decubitus position, we inserted the first 12 mm trocar in open technique in midclavicular line. 2 cm under costal margin, and after insufflation of CO2, we inserted next three 5 mm trocars. The patient had a very large liver and after division of triangular ligament from inferior border of liver, we used a grasper from the most medial trocar near epigastrium to elevate the liver for good exposure. Then, we explored the lateral border of inferior vena cava (IVC), right renal vein, and right adrenal vein. Then, the adrenal vein and subsequently the adrenal arteries were clipped and divided. Finally, adrenalectomy was done and we substituted the 10 mm lens with the 5 mm one and extracted the specimen in endobag from the 12 mm trocar (Figures 3, 4). The patient was discharged two days after the operation without any complications. The pathologic study report was myelolipoma. The patient had no complication after a 3-month follow up. Informed consent was obtained from the patient and her spouse for publication of this manuscript and related images.
3. Discussion
Laparoscopic adrenalectomy is a safe approach and was introduced in 1992 for the first time (1). Also, Morbid obesity is an independent risk factor for complications of adrenalectomy in the postoperative period. It is a risk factor for conversion to open procedure, especially in presence of large liver (hepatomegaly), large tumors, and the surgeon’s insufficient experience (2, 6).
But successful laparoscopic procedure for adrenal tumors can reduce the post-operative complications in morbidly obese patients (3).
Amador G. Ruiz de Gordejuela et al. reported successful one stage laparoscopic left adrenalectomy in addition to sleeve gastrectomy in a morbidly obese patient by supragastric approach (4).
Sergio Jose Bardaro et al. performed laparoscopic left adrenalectomy for a cortical adenoma during Roux-en-Y gastric bypass in a morbidly obese patient without any later complications (5).
Rodriguez-Hermosa et al. reported a safe laparoscopic adrenalectomy in a morbidly obese patient with a large pheochromocytoma without any complications in a 6- month follow up (6).
3.1. Conclusion
Laparoscopic adrenalectomy may be a safe procedure with good results in morbidly obese patients even in presence of large liver and can reduce the postoperative complications as well as the recovery period in comparison with the open approach especially in diabetic patients.
In fact, morbid obesity, large liver, and big tumors only can harden the laparoscopic procedure but are not contraindications for it.