1. Background
Acute myeloid leukemia (AML) is a group of genetically heterogeneous hematological disorder characterized by clonal and uncontrolled expansion of undifferentiated myeloid precursors in the hematopoietic system and is accompanied by impaired normal blood cell production (1-4). As the most common type of acute leukemia in adults, AML accounts for 75% of the newly diagnosed acute leukemia cases. Despite the development of several treatment protocols, it has been associated with poor clinical outcomes and approximately half of the patients younger than 60 years old and about 80% of the elderly patients died because of AML complications. In AML cases, the mean age of patients at diagnosis is about 70 years old (1, 3, 5, 6). More than half of the AML cases have some chromosomal abnormalities, whereas the others have a normal karyotype (NK). The recent advancements in sequencing technologies have led to the identification of several novel recurrent gene mutations in AML, including NPM1, FLT3, RUNX1, NRAS, DNMT3A, and TET2 and also in cases with normal cytogenetics (7, 8).
Tumor cells use several strategies to evade the immune system attack. For example, they induce the overexpression of immune cell-intrinsic checkpoints, including cytotoxic T-lymphocyte-associated antigen 4 (CTLA-4), programmed cell death protein 1 (PD-1), T cell immunoglobulin and mucin domain-containing protein 3 (TIM-3), T cell immune receptor with Ig and ITIM domains (TIGIT), and others on the surface of activated T cells to act as their negative regulators (9). Such strategy is associated with T cell exhaustion, which leads to the decreased anti-tumor activity in these cells (10). Several studies have shown that the elevated PD-1, TIM-3, and TIGIT expression on T cells is associated with immune suppression in AML. The combined blockade of PD-1 and TIM-3 in mouse models of AML has resulted in the decreased tumor burden and leukemia-related death (11-13). It has been also reported that the expression level of B lymphocyte-induced maturation protein 1 (Blimp-1) on T cells of initially diagnosed AML patients increases, which is linked to the up-regulation of inhibitory immune checkpoints, such as PD-1 and TIGIT on T cells and the decreased cytokine production and cytotoxicity (10). Blimp-1 transcription factor encoded by Prdm1 acts as a master regulator of B cells to plasma cell terminal differentiation (14, 15). Remarkably, Blimp-1 is involved in T cell exhaustion in mouse models of chronic viral infections (16, 17). It has also suggested that Blimp-1 exerts its suppressive effect through binding to PD-1 and TIGIT promoters and eventually leads to up-regulation of the genes. In addition, it has been shown that Prdm1 knockdown in AML patients-derived T cells can restore the normal function of these cells (10).
B cell lymphoma 6 (Bcl6) and Bach2 (BTB and CNC homologue 2) are two transcription factors, which negatively regulate the expression of Prdm1. Bach2 forms heterodimers with Maf proteins and binds to Maf recognition elements (MARE) located on the Prdm1 gene (18). It is expressed in B cells (but not plasma cells), whereas Blimp-1 expression pattern is in contrast to Bach2. In addition, loss of Bach2 is associated with elevated levels of Blimp-1 in activated B cells. Bach2 has considered as an authentic Prdm1 repressor in B cells (19-21). An epigenetic investigation suggested that H3/H4 acetylation and H3K9 methylation at the intron 5 MARE region of BAL17 mature B cells are lower and higher compared to X63/0 plasma cells, respectively. It has also widely indicated that there is an association between lower levels of acetylation in B cells and direct binding of Bach2 to regulatory regions of Prdm1. Immunoprecipitation assay in BAL17 cells showed that Bach2 forms a protein complex including some proteins, such as HDAC3, NCoR1, NCoR2, Tbl1x, and Rif1. Furthermore, down-regulation of HDAC3 or NCoR1 in B cells leads to overexpression of Prdm1 mRNA (14).
2. Objectives
The purpose of the current study was to compare the relative expression level of the Bach2 and HDAC3 genes in peripheral blood mononuclear cell (PBMC) samples of Iranian patients with AML and healthy subjects.
3. Methods
This study was performed in accordance with the Helsinki Declaration and carried out in the Imam Reza Hospital of Tehran, Iran. The informed consent was obtained from participants and the research protocol was approved by the Ethics Committee of AJA Cancer Epidemiology Research and Treatment Center (AJA-CERTC), AJA University of Medical Sciences, Tehran, Iran (approval number: #IR.CERTC.I.S.000/97/2-8780).
Twenty-four patients with de novo AML without a history of retroviral infections confirmed by hematology and oncology specialists via laboratory tests, including bone marrow aspiration and biopsy were enrolled in this study. Fifteen healthy participants (8 males and 7 females with the mean age of 52 years (age range: 26 - 71 years old)) who were matched for gender, age, and demographic characteristics were selected as the control group and blood samples were collected from all participants. Control participants as well as patients younger than 35 years old with a history of hematologic or cancer-related disorders were excluded from the study. Of the 24 patients, 6 had no history of chemotherapy.
Blood samples were collected and PBMCs were isolated. According to the protocol of manufacturer (CinnaGene, Iran), PBMCs were used for RNA extraction using RNX plus reagent. Quality and concentration of RNA samples were determined by spectrometry. Complementary DNA (cDNA) synthesis was carried out by HyperscriptTM first-strand synthesis kit (GeneAll, South Korea). Measurement of the relative gene expression of BACH2 and HDAC3 was performed by quantitative real-time PCR (qRT-PCR) (Corbett research RG-6000 real-time PCR machine, Australia) and SYBR Green PCR Master Mix (Amplicon, Denmark) using Pfaffl method. Beta-2 microglobulin (B2M) gene was selected as the internal control to normalize the relative expression levels of the target genes. All reactions were performed in duplicate. The amplification reactions consisted of an initial denaturation step at 95ºC for 15 min, followed by 40 cycles of denaturation at 95ºC for 15 s, annealing at 60ºC for 30 s, and extension at 72ºC for 30 s. The primer sequences used in this study are listed in Table 1. The obtained results as well as qRT-PCR data were analyzed by student’s t-test, chi square, and Shapiro-Wilk using GraphPad Prism version 7.0 for Windows (GraphPad Software, La Jolla, CA., USA).
| Target Gene | Primer Sequence (5’-3’) | Length, bp | GC, % | Product Length, bp | TM, ºC |
|---|---|---|---|---|---|
| Bach2 | F: 5’-ATGATTTGGTGGTCAGCTTGC-3’ | 22 | 50.00 | 244 | 59.05 |
| R: 5’-TCGCGGATGTTTTCTCTGCT-3’ | 22 | 45.45 | 59.83 | ||
| HDAC3 | F: 5’-TGGCACAGGTGACATGTATGA-3' | 21 | 47.62 | 126 | 59.37 |
| R: 5'-ACCTGGTTGATAACCGGCTG-3’ | 20 | 55.00 | 60.04 | ||
| B2M | F: 5’-CCTGAATTGCTATGTGTCTGGG-3’ | 21 | 47.62 | 109 | 59.45 |
| R: 5’-TGATGCTGCTTACATGTCTCGA-3’ | 20 | 50.00 | 60.04 |
Sequence of Primers Used for qRT-PCR
4. Results
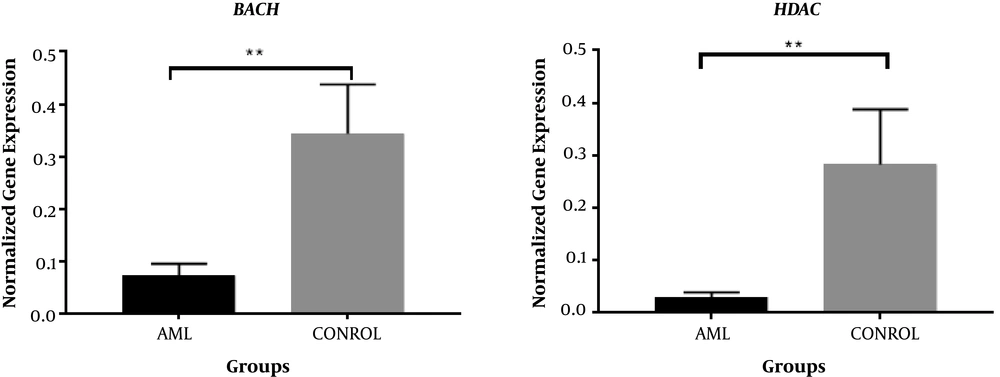
In this study, the comparison between the two groups of patients showed a decrease in the expression levels of Bach2 and HDAC3 genes. Demographic and clinical characteristics for both patients and control groups are indicated in Table 2. There was no significant correlation between demographic characteristics and expression level of Bach2 and HDAC3 genes (P > 0.05). Therefore, other factors did not significantly affect the changes in expression levels of these genes. Comparison of the relative gene expression in patients and control groups revealed that expression level of both Bach2 (P = 0.0017) and HDAC3 (P = 0.0026) genes are down-regulated in AML patients by 4.97 and 6.14-fold, respectively (Figure 1 and Table 3).
| Variable | Patients (n = 24) | Controls (n = 15) | P Value |
|---|---|---|---|
| Age | 54 ± 16.64 | 52 ± 15.12 | 0.8821 |
| BMIb | 24.07 ± 3.84 | 25.13 ± 4.18 | 0.7862 |
| Gender, %c | 0.9384 | ||
| Male | 54.2 | 54 | |
| Female | 45.8 | 46 | |
| Smoking, %c | 0.8306 | ||
| Yes | 12.5 | 13.5 | |
| No | 87.5 | 86.5 | |
| Family historyb | 0.0951 | ||
| Yes | 4 | 0 | |
| No | 20 | 15 | |
| WBCb, 109/L | 7.29 ± 5.03 | 7.42 ± 1.87 | 0.9999 |
| Plateletb, 109/L | 78.62 ± 61.06 | 247 ± 48.45 | 0.0196 |
| Hemoglobinb, 109/L | 9.14 ± 1.98 | 12.4 ± 0.87 | 0.0388 |
Clinical Characteristics of AML Patients Who Participated in the Studya
| Target Genes | AML | Control | P Value | Fold Change |
|---|---|---|---|---|
| Bach2 | 0.07428 ± 0.0222 | 0.344 ± 0.09348 | 0.0017 | 4.97 |
| HDAC3 | 0.0306 ± 0.0088 | 0.2831 ± 0.1048 | 0.0026 | 6.14 |
Pairwise Comparison of Bach2 and HDAC3 Expression Level Changes in PBMCs of Patients and Control Groupsa
5. Discussion
In the present study, we compared the expression levels of Bach2 and HDAC3 genes in AML patients and healthy controls. A decrease was found in the expression levels of the genes in patients by 4.97 and 6.14-fold, respectively.
AML is a heterogeneous disorder, in which cells-of-origin of the tumor undergo dynamic and continuous genetic and epigenetic evolution and each AML case might be regarded as a complex mosaic structure of cells consisted of various compositions of sequentially acquired genetic and epigenetic variations (22). Therefore, identification of the epigenetic abnormalities involved in developing leukemia is critical for unrevealing its complex biology. T cells act as key factors in immune response in tumor surveillance. The balance between co-stimulatory and co-inhibitory signals (immune checkpoints) regulates the ultimate anti-tumor T cell responses (23, 24). Cancer cells can develop a mechanism to deregulate the expression of the negative regulatory immune checkpoint receptors such as CTLA-4, PD-1, TIGIT, TIM-3, and LAG-3 on T cell surface and consequently avoid their elimination by the immune system. This mechanism is highly associated with T cell exhaustion, which is linked to their decreased capacity of the cytokine production, cytotoxicity, and compromised anti-tumor activity. In recent years, immune checkpoint blockade compounds have revolutionized cancer immunotherapy (25-27).
Bach2 is a highly conserved transcription factor with a critical role in the regulation of differentiation and maturation of B and T cells. Therefore, a significant decrease in the expression level of Bach2 in the studied patients can be effective in the process of lymphocyte maturation and autoimmune disease. In other studies on the immune diseases, a decrease in Bach2 and an increase (P < 0.001) in PRDM1 mRNA were found in pancreatic tissues, whereas BACH2+/CD4+ T-lymphocytes were decreased (P < 0.01) in the circulation and tissues (22).
Blimp-1 is a zinc-finger containing transcription repressor with a pivotal role in the development of mouse embryo, which controls differentiation of the antibody-producing plasma cells and myeloid lineage and also regulates the expression of some genes, such as INF-β and IL-10 (28). It has been reported that Blimp-1 up-regulates the expression of PD-1 and TIGIT immune checkpoints on the activated T cells leading to T cell exhaustion in AML (10). PD1 is an inhibitory receptor and shows a wide expression pattern. PD1 is mainly involved in limiting T cells activity in peripheral tissues to avoid autoimmunity and restrict the inflammatory responses (29). Another inhibitory checkpoint, TIGIT, belongs to the immunoglobulin superfamily of proteins, which is expressed on lymphocytes and also plays important roles in autoimmunity and antitumor responses (30). Bach2 is a highly conserved transcription factor with a critical role in regulation of differentiation and maturation of B and T cells. Recently, mutations in the Bach2 gene have been found as effective in BACH2-related immunodeficiency and autoimmunity (BRIDA) syndrome in humans, characterized by deficiency of lymphocyte maturation (31). In the absence of Bach2, CD4+ T cells indicate the increased differentiation to effector cells producing higher levels of Th2-related cytokines, such as interleukin 4 (IL-4) and interleukin 10 (IL-10) and also a reduction in the generation of regulatory T cells (24). Bach2 can repress the expression of Blimp-1 possibly done by direct interaction with the proteins, like NCoR1 and NCoR2, which form corepressor complexes with HDAC3 and other histone deacetylases (14). Bach2 is suggested to cooperate with HDAC3-containing co-repressor complexes in B cells to regulate the stage-specific expression of PRDM1 by writing epigenetic modifications at the Prdm1 locus (23). Histone deacetylases are epigenetic factors associated with gene silencing through modulating the chromatin structure. In addition, they control DNA damages and maintain the genomic stability (32, 33). HDAC3 belongs to the class 4 HDACs and its blockage has been considered as a therapeutic strategy to treat various types of cancers, including multiple myeloma (34, 35). Accordingly, we suggested that investigating the expression levels Bach2 and HDAC3 genes in AML patients and healthy cases may explain epigenetic mechanisms involved in T cell exhaustion in AML and its pathogenesis. In the present study, we compared the expression levels of Bach2 and HDAC3 genes in AML patients and healthy controls and it was found that they have undergone a relative down-regulation in AML group by 4.97 and 6.14-fold, respectively. The expression of Prdm1 gene is negatively regulated by Bach2. Moreover, HDAC3 usually represses the transcription of several genes and its epigenetic expression reduction is associated with increased transcription of Prdm1 gene (14). Therefore, the complex entity of AML can be explained by the dysregulation of multiple gene networks including several genes.
5.1. Conclusions
Bach2 and HDAC3 are just two examples of the dysregulated genes among a large group that their decreased expression in the patients may explain the elevated expression of Prdm1 and also up-regulation of some immune checkpoints. It should be noted that the currently-used chemotherapy is regarded as the main choice for treatment of AML, however taking some chemotherapy agents by the patients may somehow affect the expression level of both Bach2 and HDAC3 genes in patients.