1. Background
Cancer is one of the leading cause of death globally. Chemotherapeutic drugs have been the mainstay of cancer treatment regimens since the 1960s (1). While these drugs were credited with a higher level of success than experienced before they have fallen far short of expectations. Most chemotherapeutic agents target the division of cancer cells and disrupt mitosis (2). However, they are accompanied by serious and debilitating side effects including headache, nausea, hair loss, blood cell disorders, and lowered immune levels (3). Often, side effects are the primary reason for non-adherence to drug schedules by patients, leading to poor outcome (4-6). The limited effectiveness of conventional cancer treatment methods and the development of resistance is a root cause of cancer associated mortality (7-9). In contrast, phytochemicals have given a more promising outcome in the treatment and cure of cancer by eliminating the negative impacts of chemotherapy, targeting metastasis, and tumor induction (10). Several compounds from our diet such as epigallocatechin-3-gallate (green tea), curcumin assist in reducing cell proliferation, and initiate apoptosis thereby producing anti-neoplastic effects (11, 12). Cancer occurrences worldwide can be brought down by 7 to 31% by increasing fruits and vegetables in our daily diet (13).
Considering that cancer is a multifactorial disease, therefore, one approach using a stand-alone agent may be inadequate to ensure efficacy. A multi-pronged approach using different agents in combination with conventional chemotherapeutic agents may enhance efficacy at a lower dose, reduce nonspecific cytotoxicity, alleviate adverse side effects, and impede the development of chemoresistance. However, when different compounds are used in combination, several different interactions (additive, synergistic, or antagonistic) are possible rendering certain combinations ineffective (14). It is important to achieve a combination of agents that will synergistically interact with each other and elevate the level of anti-cancer activity. Several studies which were attempted to evaluate a cocktail of phytochemicals and/or phytochemicals with chemotherapeutic agents have shown its massive potential for cancer treatment (15, 16).
Cisplatin belongs to a class of platinum-containing chemotherapeutic compounds and is widely used for the treatment of solid malignancies. Cisplatin has lots of side-effects such as nephrotoxicity, nausea and vomiting, hearing loss, electrolyte imbalance, and hemolytic anemia, which can limit its use (17). A majority of patients eventually develop cisplatin-resistant disease necessitating a combinational therapy approach (14). 5-fluorouracil has broad spectrum activity against solid tumors and interferes with nucleoside metabolism to bring about cell death, producing side effects similar to cisplatin (18). Sulforaphane belongs to the isothiocynate family of polyphenols and can be obtained from cruciferous vegetables including cabbage, cauliflower, and broccoli (19). In addition, It mediates cell cycle arrest, apoptosis, and inhibits (20, 21). Quercetin is a flavonoid, which is found ubiquitously in several dietary sources including apples, onions, honey, red grapes, berries, most citrus, and green leafy vegetable (22). It has been found to have anti-cancer, anti-inflammatory, anti-microbial, anti-angiogenic, and apoptosis-inducing properties (23, 24).
2. Objectives
The present study aimed to evaluate the effect of quercetin and sulforaphane in combination with each other as well as with the chemotherapeutic agents (cisplatin and 5-fluorouracil) on cervical cancer cells, HeLa. This would help ascertain the nature of the interaction between the phytochemicals and the chemotherapeutic agents and facilitate the calculation of the combination index.
3. Methods
This research project has been approved by the departmental research committee. Necessary ethical approvals have been taken to conduct this research.
3.1. Cell Culture
HeLa, the human cervical carcinoma cell line, was maintained in DMEM (Dulbecco’s Modified Eagle’s medium) (Sigma, USA) supplemented with 10% fetal bovine serum (FBS) (Sigma, USA) and 100X Pen-strep (Sigma, USA) in a saturated atmosphere of 5% CO2 in air at 37°C.
3.2. Preparation of Drug Solutions
Quercetin and sulforaphane were obtained from Sigma (USA). A 10 mM main stock of the agents were prepared and stored at -20°C. Sulforaphane was prepared in media while quercetin was prepared in DMSO. Further, dilutions of these agents were made in complete medium to required concentrations for treatments. 1.6 mM of cisplatin (Cadila Pharmaceuticals Ltd, India) and 384.37 mM of 5-fluorouracil (Biochem Pharmaceuticals, India) were used as the stock solution to obtain further dilutions in DMEM.
3.3. Cell Viability Assay Following Co-Administration of Different Agents
The anti-proliferative effect of quercetin (EC50 100 µM/24h), sulforaphane (EC50 12 µM/24h), cisplatin (EC50 12.5 µM/24h), and 5-fluorouracil (EC50 100 µM/24h) was previously assessed by using the MTT assay individually on HeLa cells (25, 26). Three sublethal doses of each chemotherapeutic agents and phytochemicals were combined to yield a range of nine different combinations per pair as demonstrated in Table 1. The concentrations tested for quercetin and 5-fluorouracil were 10, 25, and 35 µM, respectively. The concentrations of used cisplatin were 1, 2, and 5 µM while the used sulforaphane was 1, 2, and 5 µM. 96-well plates were used to seed ~10,000 HeLa cells/well and incubated overnight at 37°C. Then they were treated with different combinations of agents for 24 hours. MTT (at final concentration of 0.5 mg/mL) (Sigma, USA) was added and incubated for 2 hours at 37°C followed by addition of 100 µL DMSO (Sigma, USA). Absorbance microplate reader (BioTek, USA) was used for the measurement of absorbance at 570 nm. The effect of the drug was calculated as follows: percentage cell viability is equal to (OD of the treated cells /OD of the untreated cells) × 100. The assay was performed thrice and the average was represented in the data.
| Quercetin | Sulforaphane | ||||||
|---|---|---|---|---|---|---|---|
| - | 10 µM | 25 µM | 35 µM | 1 µM | 2 µM | 5 µM | |
| Cisplatin | |||||||
| - | - | Q (95) | Q (92.8) | Q (87.5) | S (96.1) | S (88.2) | S (67.7) |
| 1µM | C (89.5) | C1Q1 (84.7) | C1Q2 (79.8) | C1Q3 (74.5) | C1S1 (87.3) | C1S2 (62) | C1S3 (43.6) |
| 2 µM | C (85.5) | C2Q1 (60) | C2Q2 (58.6) | C2Q3 (57.05) | C2S1 (73.0) | C2S2 (69.0) | C2S3 (32.3) |
| 5 µM | C (73.9) | C3Q1 (41.17) | C3Q2 (38.82) | C3Q3 (31.9) | C3S1 (66.0) | C3S2 (44.2) | C3S3 (23.1) |
| 5-Fluorouracil | |||||||
| 10 µM | F (98.2) | F1Q1 (71.3) | F1Q2 (69.4) | F1Q3 (58.4) | F1S1 (84.9) | F1S2 (78.9) | F1S3 (47.3) |
| 25 µM | F (96) | F2Q1 (65.1) | F2Q2 (62) | F2Q3 (58.1) | F2S1 (82.7) | F2S2 (74.0) | F2S3 (41.7) |
| 35 µM | F (94.7) | F3Q1 (70.2) | F3Q2 (58.4) | F3Q3 (55.1) | F3S1 (77.2) | F3S2 (61.8) | F3S3 (40.9) |
| Quercetin | |||||||
| 10 µM | Q (95) | - | - | - | Q1S1 (89.4) | Q1S2 (75.0) | Q1S3 (69.5) |
| 25 µM | Q (92.8) | - | - | - | Q2S1 (78.0) | Q2S2 (74.0) | Q2S3 (64.5) |
| 35 µM | Q (87.5) | - | - | - | Q3S1 (76.0) | Q3S2 (69.7) | Q3S3 (52.5) |
Abbreviations: C, Cisplatin; F, Fluorouracil; Q, Quercetin; S, Sulforaphane.
aValues are presented as (%.)
3.4. Calculation of Combination Effects Following Co-Administration of Different Agents
Combination index (CI) was used to express the effect of concurrent use of drugs and is indicative of the drug interaction as defined by Chou and Talalay (14). CI was calculated by using the following formula:
CI = CAx/ICx,A + CBx/ICx,B
CAx and CBx refer to the concentrations of A and B drugs administered concomitantly to achieve x% drug effect, respectively. ICx, A and ICx, B denote the individual concentrations of the drugs that result in the same effect. A CI value < 1, = 1, or > 1 implies, synergy, additivity, or antagonism of the two drugs.
3.5. Cell Cycle Analysis Using PI Staining Via Flow Cytometry Following Co-Administration of Phytochemicals and Chemotherapeutic Agents
A total of 2 × 106 cells were treated with the compounds alone and with the combinations CIQ2, C1Q3, F1Q2, F1Q3, C1S2, C1S3, F1S2, F1S3, Q1S2, and Q2S2 for 24 hours. Following the harvest of attached and floating cells, they were washed with PBS, resuspended in 1ml of PBS, and fixed in 70% ethanol at 4°C. Then Cells were washed in PBS twice, counted and stained with a solution containing PI (1 mg/mLl) 0.1%, Triton X-100, and 100mg/mL of RNase A for 45 minutes at 37°C. Cells were processed using a BD FACS and data were analyzed with FlowJo software. From DNA histograms analysis, the percentage of cells in the different phases of the cell cycle was evaluated. The Sub-G1 peak corresponds to < 2n DNA content and was therefore considered to be suggestive of the apoptotic population.
3.6. Scratch Wound Assay Following Co-Administration of Different Agents
The effect of the various combinations of the agents on tumor cell migration was examined by performing the cell migration assay as previously described (27). Cells were seeded in 6-well plates at a density of ~ 5 × 105 cells per well and cultured until completely confluent. A yellow tip was used to score a constant diameter wound or cell-free line. As were shown in Table 1, Cells were treated with the following combinations: CIQ2, C1Q3, F1Q2, F1Q3, C1S2, C1S3, F1S2, F1S3, Q1S2, and Q2S2. Untreated cells were used as control. Migration of the cells across the cell- free line was monitored microscopically at 0, 24, 48, and 72 hours and images were obtained every 24 hours. Monitoring was continued until the cell-free line in the control wells reached complete closure. The wound width was measured by using MS paint and the arrow was drawn to indicate the cell-free zone. The percentage of wound closure/widening was calculated and represented as a graph.
3.7. Statistical Tools
Experiments were conducted in triplicate. One way ANOVA was used to obtain the P values for all the results obtained using Graph Pad.
4. Results
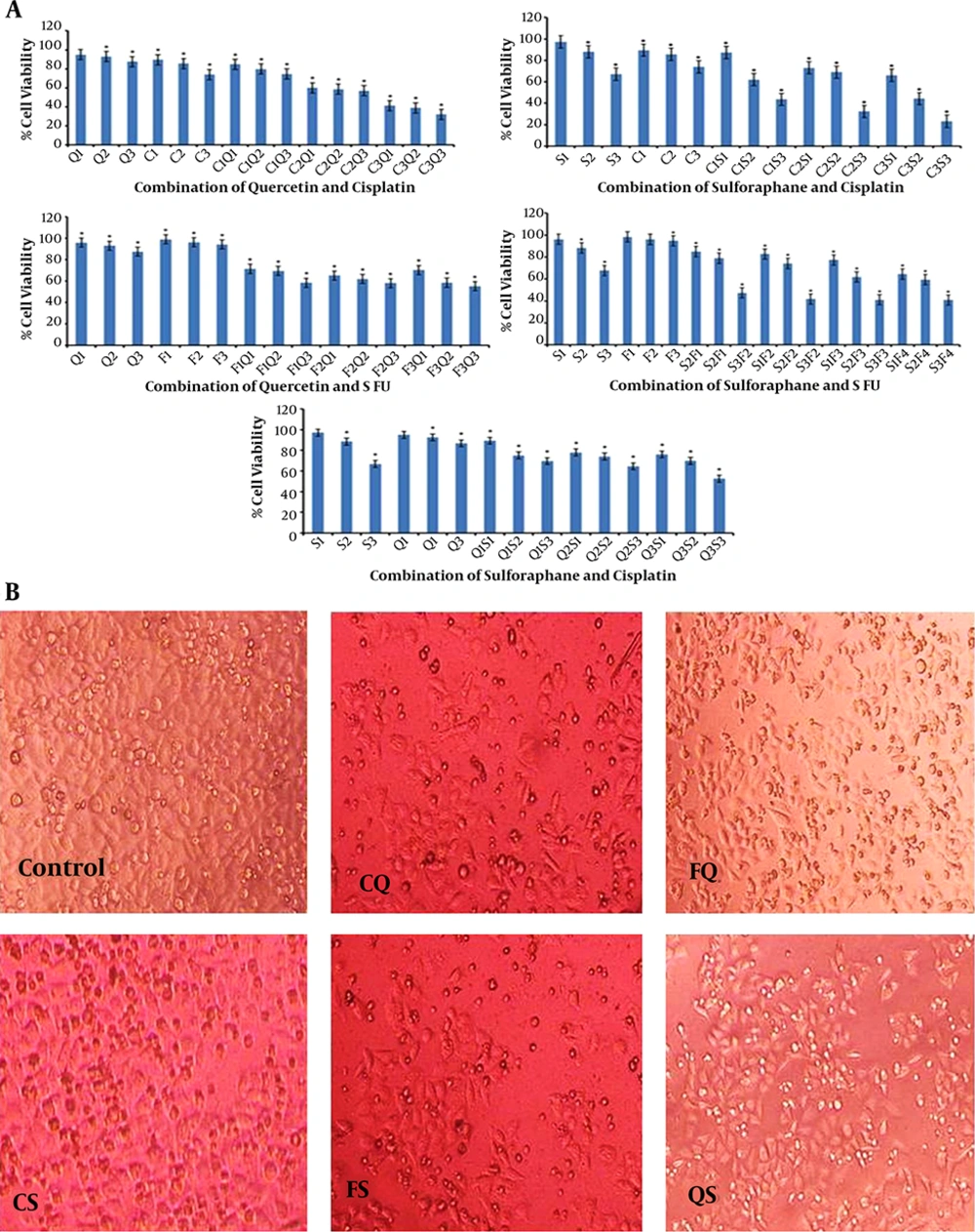
4.1. Quercetin Potentiates the Action of Cisplatin and 5-Fluorouracil In HeLa Cells
HeLa cells were simultaneously treated with different combinations of sub-lethal doses of quercetin (Q1, Q2, Q3) with cisplatin (C1, C2, C3) and quercetin with 5-fluorouracil (F1, F2, F3) for 24 hours. All the tested combinations led to a synergistic decline in cell viability of HeLa cells, compared with either of the compounds alone (Figure 1 and Table 1). While 5 µM cisplatin alone corresponded to a viability percentage of 73.9%, in combination with quercetin the viability was lowered to 41.1% with C3Q1, 38.8% with C3Q2, and 31.9% with C3Q3. The lowest concentration of cisplatin tested had a viability percentage of 89.5% whereas it was 74.5% with C1Q3 showed that quercetin was able to potentiate the action of cisplatin resulting in a sharp decline. The CI was calculated for each of the 9 combinations and found to be less than 1 which indicates a synergistic interaction. Quercetin also demonstrated a synergistic interaction with 5-fluorouracil across all the combinations tested (Figure 2). 10 µM 5-fluorouracil exhibited very low lethality against HeLa cells with 98.8% of the cells surviving; however, when administered in combination with quercetin the decline in viability was steep recording 71.3% with F1Q1 and 69.4% with F1Q2 and F1Q3.
A, concurrent treatment of cisplatin with i. quercetin and ii. sulforaphane potentiates the effect of cisplatin in HeLa cells (combination index (CI < 1). Concurrent treatment of 5-fluorouracil with iii. quercetin iv. sulforaphane potentiates the effect of 5-fluorouracil in HeLa cells (CI < 1). v. Concurrent treatment of quercetin and sulforaphane potentiates each other’s effect on HeLa cells (CI < 1). Values are means ± SD of three independent experiments (* represents P ≤ 0.5). B, representative pictures of morphological features of cell death and apoptosis seen as an outcome of treatment with various combinations of cisplatin, 5-fluorouracil with the phytochemicals in comparison to untreated control (CQ-cisplatin with quercetin, FQ-5 fluorouracil with quercetin, CS-cisplatin with sulforaphane, FS-5-fluorouracil with sulforaphane, and SQ-sulforaphane with quercetin).
4.2. Sulforaphane Potentiates the Action of Cisplatin and 5-Fluorouracil In HeLa Cells
Concurrent treatment of HeLa cells with sublethal doses of cisplatin and sulforaphane as well as sulforaphane and 5-fluorouracil was found to bring about a synergistic decline in cell viability. The CI was calculated for each of the combinations and found to be less than 1 (Figure 1 and Table 1). 5 µM sulforaphane (S3) individually caused 67% viability, while all three concentrations of 5-fluorouracil tested had viability greater than 90%. In contrast, combinations of 5-fluorouracil with S3, led to sharp drop in cell viability to 47.3%, 41.7%, and 40.9% for F1S3, F2S3, and F3S3, respectively. This indicates the synergistic interaction of cisplatin and 5-fluorouracil with sulforaphane across all the combination dosages tested.
4.3. Sulforaphane Potentiates the Action of Quercetin in HeLa Cells
In order to ascertain whether a combination of quercetin and sulforaphane would have a far stronger effect on HeLa cells than either of them individually, concurrent treatments were initiated. Higher doses of quercetin with the same dose of sulforaphane progressively decreased cell viability (Q1S3-69.5%, Q2S3-64.5%, Q3S3-52.5%). The same trend was observed when sulforaphane concentration was increased while keeping quercetin dose constant (Q2S1-78%, Q2S2-74%, Q3S3-52.5%). This underscores their synergistic interaction and is exemplified by the CI index calculation which is less than 1 (Figure 1 and Table 1).
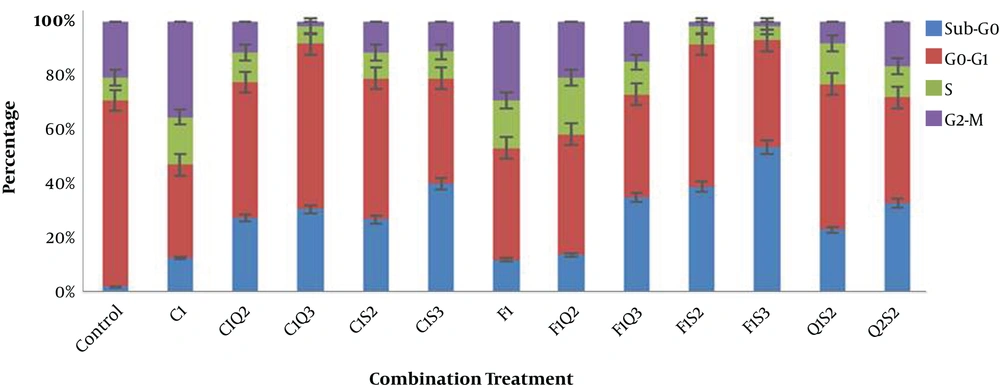
4.4. Phytochemicals in Combination with Cisplatin and 5-Fluorouracil Impact the Cell Cycle
The data were obtained after subjecting the stained and treated cells to flowcytometry and analyzed using FlowJo software. Based on the findings, in comparison to the control cisplatin and 5-fluorouracil promoted a G2M phase arrest marked by an increase in the population of cells in the G2 phase. C1Q2 and C1Q3 combinations caused G1 phase arrest evidenced by an increase in the G1 phase cell population. C1Q2 and C1Q3 had 25.1% and 36.1% of the population in subG0, respectively; whereas F1S2 and F1S3 had 37.1% and 51.8% of that. Based on the results, an increase in the subG0 population correlated with an increase in the concentration of the doses used. In addition, it was found that the combinations of quercetin and sulforaphane with each other and the chemotherapeutic agents disturbed the cell cycle and greatly increased the proportion of apoptotic sub-G0 population underscoring their apoptosis inducing property (Figure 2). The results of the cell cycle analysis supported the data obtained from cell viability and morphology assessments.
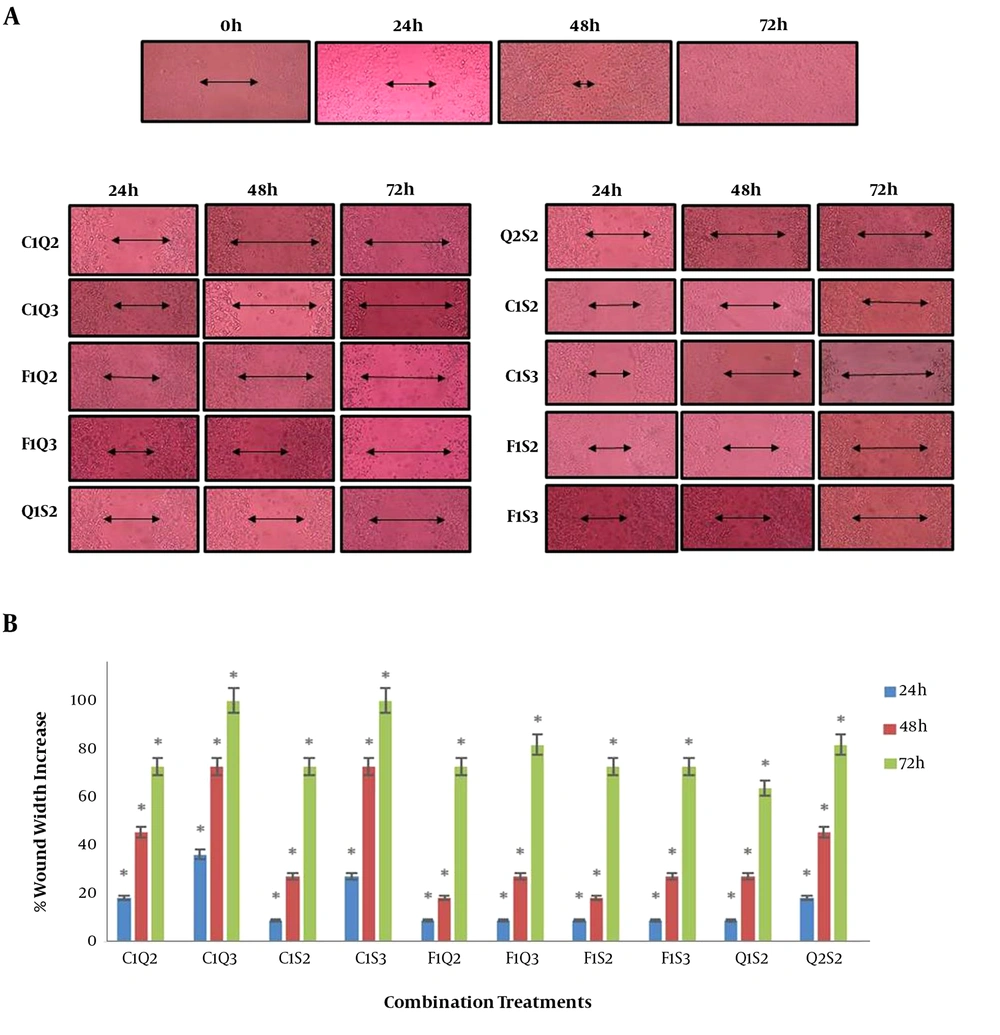
4.5. Phytochemicals in Combination with Each Other and with Cisplatin and 5-Fluorouracil Demonstrate Antimigratory Effect
HeLa cells were simultaneously treated with two different combinations of chemopreventive agent and cisplatin/5-fluorouracil for 24 hours. The antimigratory effect of the combinations was compared to untreated controls at 0, 24, 48, and 72 hours of treatment. The data indicated that the tested combinations inhibited cell migration more significantly compared to treatment with each agent individually. The combinations showed evident antimigratory effect on HeLa cells with the cell-free zone remaining unclosed and further widened consequent to the cell death. Doubling of the width of the initially cell-free line in C1Q3 and C1S3 was observed, highlighting that these two combinations have very high antimigratory potential. In all cases, the combinations showed antimigratory and cytotoxic outcomes with higher concentrations producing better results (Figure 3). One way ANOVA was performed and the migration inhibition in treated samples in contrast to the control was found to be significant.
A, cell migration analysis using scratch wound assay. Pictures show the changes in the cell-free zone over time. The first panel shows the closure of wound in untreated control cells. Complete closure was obtained in 72 hours. The change in wound width over time for each of the tested combinations is documented in the panels below. B, graphs indicate the percentage increase in the cell-free zone over time in in the wells treated with different combinations (* represents P ≤ 0.1).
5. Discussion
Cancer remains a main public health concern and is a major cause of death globally. Despite the progress that has been made in the field of cancer treatment and prevention, cancer morbidity and mortality can be largely attributed to the limitations of available treatment strategies, their side effects, and drug resistance (25, 28). It is necessary to identify pharmacologically safe agents that can act on all the stages of carcinogenesis. It seems that polyphenols could fill this lacuna, as several studies have highlighted the success of polyphenol-diet rich in combatting and preventing cancer. Polyphenols are reported to have anticarcinogenic properties against different types of cancers (21, 25). As carcinogenesis is a multistep process so it is doubtful that a single-agent would validate as an effective treatment. Combination treatment with different polyphenols or with polyphenols and other anti-cancer drugs is a rational option in order to augment their effectiveness at a lower dose by increasing effective targeting, reducing adverse effects, and chemoresistance (29-31).
The ability of polyphenols to modulate diverse signal transduction pathways involved in carcinogenesis indicates that combinations of polyphenols can significantly thwart tumor growth and is supported by promising pre-clinical data. Assessing cell cycle distribution and cell proliferation is important for studying cell growth differentiation and apoptosis. This enables one to investigate underlying basic mechanisms as well as to evaluate therapeutic efficacies of anti-cancer drugs. In this study, we found that concurrent administration of a combination of chemotherapeutic drugs like cisplatin and 5-fluorouracil with the phytochemicals quercetin and sulphoraphane synergistically decreased cell viability and initiation of apoptosis (Figure 1). Further, quercetin and sulforaphane also exhibited synergism at the tested doses. The enhanced growth inhibitory effects in comparison to the individual doses were found for all tested combinations as well as they werecorrelated with microscopic examination of the cells, which demonstrated the characteristic rounding off of cells and nuclear condensation associated with apoptosis. During cell cycle progression, proliferating cells sequentially undergo a transition of G1→S→G2→M phases for the synthesis of DNA, preparation of cell division, and subsequent mitosis. Results of this study showed that cisplatin induced a G2M phase arrest in HeLa cells (Figure 2); this finding is similar to previous results (32). Cisplatin-induced apoptosis is evident from the sub-G0 population increase and morphological analysis performed and is consistent with earlier findings (33, 34). Quercetin induces G2M phase arrest and apoptosis as well as evident from our earlier study (35). According to our previous study and others’ reports, Sulforaphane induces G2 phase arrest and shows an accumulation of sub-G0 cells (19). Flowcytometry confirmed the distortive impact of the tested combinations on the cell cycle and in some cases spike in G1 phase and established apoptosis through the increasing sub-G0 population (Figure 2). It has been suggested that human papillomavirus (HPV) requires cells to enter M phase in order to become infective; further, a role for combination therapy, which can initiate cell cycle arrests at G1 has been suggested in the other studies, as documented in this study (36). Cisplatin has demonstrated synergy with several phytochemicals, especially, pretreatment with quercetin has found to sensitize the cells to cisplatin (37, 38). In the present study, we highlighted that co-administration of cisplatin and quercetin also potentiates the action of cisplatin. This is particularly useful as most chemotherapeutic regimens might preclude pre-treatment with phytochemicals but may be more amenable with co-administration strategies.
Next we have sought to understand the role of these combinations of agents on migration of HeLa cells by performing the classic wound migration assay using selected combinations. The untreated cells showed progressive closure of the wound with complete confluency in the cell-free zone reached in 72 hours. In comparison to this, it was found that the combination treatments were able to mitigate the migration of cells and no wound closure was seen. In contrast, the exposure to these combination cocktails resulted in broadening of the wound (Figure 3). This can be explained due to the apoptosis induction. The results demonstrated an increased anti-migratory potential of the combinations in contrast to the individual agents and the control. Quercetin and sulforaphane have been shown earlier to exhibit synergy in wound healing (39). This further reinstates the potential of combination therapy on the different hallmarks of cancer. In addition, molecular biology exploration would allow us to understand the pathway through which these agents impact the hallmarks and exhibit synergy.
According to the results of the previous studies, the natural agent sulforaphane enhanceed the therapeutic index of the chemotherapeutic agent, gemcitabine, and exerts differential effects in combination with eugenol (21, 25). An effort to catalogue all possible phytochemical and chemotherapeutics combinations in various dosages is required to ascertain the best possible synergistic combinations with the highest anticancer potential. However, the success of in vitro studies needs to be authenticated by in vivo studies in order to account for the effect of pharmacokinetic and genotypic variations, the bioavailability of the compound, and other metabolic alterations.
In this study, we showed that quercetin is able to synergistically potentiate the effect of the chemotherapeutic agents, cisplatin, and 5-fluorouracil with a significant decrease in the viability of HeLa cells and alteration in the cell cycle distribution. In addition, the combinations were found to mitigate cell migration with maintenance of the cell-free zone. Further, sulforaphane was also found to potentiate the effect of the chemotherapeutic drugs by increasing cell death, altering the cell cycle, and inhibiting cell migration. Furthermore, sulforaphane and quercetin were also able to potentiate the activity of each other in the absence of chemotherapeutic agents. This study emphatically showed that combination studies utilizing natural agents with chemotherapeutic agents hold great promise. Such synergistic combinations will facilitate the development of a multi-pronged therapeutic approach, which may help overcome the problems associated with chemotherapy. Further, in vivo exploration of these combinations is warranted and will allow detailed assessment of their effect.