1. Background
Now, cancer is considered one of the most important issues in health care for our country and around the word (1), and according to the latest statistical review, it is the third cause of mortality after cardiovascular disease and unintentional injuries (2). Therefore, the study of psychopathology and health, as well as factors affecting these components, is necessary and urgent. It is clear that cancer is an extremely distressing experience for the patient and affects various aspects of the quality of life, including physical, psychological, social, economic, and sexual function. Patients’ quality of life is affected by their perception of life, values, goals, standards, and interests (3). Studies of patients with cancer indicate that the severity of the disease and the accompanying mental stress is associated with the quality of life (4, 5). Research has recently shown that some personality, behavioral, and psychotherapy variables may provide direct and indirect favorable contexts to the disease and improve the quality of its sufferers (6).
One of these psychological factors is personality characteristics. A number of experts have described personality, using 5 major dimensions: neuroticism, extraversion, openness to experience, agreeableness, and conscientiousness (7). Personality characteristics such as extroversion can be advantageous because they strengthen the individual’s ability to benefit from social relationships and emotions as well as their ability to experience enjoyable events (8, 9), thus, improving the different aspects of health and quality of life. On the other hand, neuroticism can increase the individual’s vulnerability to stressor events, and make them prone to experiencing negative emotions and frustration and, thereby, undermine their health and quality of life (8). Therefore, personality characteristics can directly affect the patient’s quality of life, but on the other hand, other studies have shown that personality characteristics, by mediating other psychological variables such as cognitive emotion regulation strategies and goal adjustment, can indirectly affect people’s quality of life (10).
Emotion regulation consists of strategies that cause the reduction, maintenance, or increase of emotion and refers to the processes, by which the current emotional state of an individual is affected (11). Generally, emotion regulation is critical in initiating, motivating, and organizing adaptive behavior, and in preventing stressful levels of negative emotions and maladaptive behavior (12). A number of research studies have shown that the regulation of emotions by cognitions or thoughts is inextricably associated with human life and helps people to keep control over their emotions during or after the experience of threatening or stressful events (13, 14). For this reason, experts believe that those who are not able to properly manage their emotional response to life events suffer from psychological damage more than others (15). So, emotional regulation is an important factor in the determination of mental health and effective action (16) that plays a vital role in the patient’s adaptation to stressor events and makes a person prone to be affected by acute and chronic physical diseases such as cancer by influencing the stress level and decreasing the safety system performance. The results of several studies (17, 18) show that patients with cancer use more maladaptive strategies, such as rumination and catastrophizing, and are more tolerant of depression and negative emotions (19). Also, the investigations showed that emotional regulation has a positive significant relationship with the personality dimensions of extraversion, openness to experience, agreeableness, and conscientiousness and a negative significant relationship with neuroticism (20).
Another psychological variable, which plays a mediating role in relationship between personality characteristics and quality of life, is goal adjustment. Research carried out on self-regulation and human adaptive behavior often insists on the importance of achieving the goals, processes, and associated variables (21). The ability to discard an unattainable goal will help a person to prevent the accumulation of failure based on experiences. Moreover, discarding the goal leads to redefining the goal and the person discovers that this goal is not necessary in her/his life for her/his satisfaction (22). In this regard, many researchers have pointed to the lack of suitable goal adjustment in reduced quality of life, increased depression and confusion, and decreased mental health (23). The results showed that patients with cancer have a problem in adjusting their goals or the abandonment of unattainable goals, which causes them to experience mental rumination, depression, and negative emotion (18).
There has been an increasing incidence of cancer in society, and its impact on various aspects of the lives of people suffering from the disease is significant. Most of the above-mentioned recent studies have focused on the role of personality factors that directly affect the quality of life of people with chronic diseases and few of them have examined the indirect effect of these factors on mental health and quality of life. Therefore, this study aimed at examining the indirect effects of personality characteristics by mediating the cognitive emotion regulation strategies and goal adjustment in improving quality of life for patients with cancer.
2. Methods
2.1. Patients
The population of this study includes patients with cancer, who attended the Reza clinic, Isar, Imam Reza hospital and a privet office in Mashhad, Iran during the study. To select the sample of this study, the first step was to approach these institutions and obtain their consent and cooperation in collecting data. The researcher was given a list of patients with cancer, by Reza Radiotherapy and Oncology Center, who were admitted to this hospital during the study. From this list, patients with the required profile were selected (i.e., aged between 20 - 60 years; at least a middle school qualification; awareness of their disease and lack of an acute condition with a physician’s diagnosis). The same selection criteria were applied at the other centers. A total of 160 patients were selected by eligibility and obtaining informed consent. They were asked to complete research questionnaires and, finally, the data were analyzed from 156 respondents (49 male and 107 female). The mean age was 45 years (SD 10:8), ranging from 20 to 60 years. A large group was married (84%). Other patients were divorced (8%) and single (8%). A relatively high percentage had a middle vocational or secondary education (40%). Other patients had higher vocational or university education (35%), finished primary education (23%), and lower vocational or secondary education (2%). Most patients were diagnosed with breast cancer (47%), followed by ovarian cancer (11%) gastric cancer (9%), leukemia cancer (7%), liver cancer (6%), lymphoma (5%), brain tumor (5%), esophageal (4%), colorectal cancer (2%), kidney cancer (2%), and prostate cancer (2%). Also, since diagnosis time, 67% of the patients had spent less than 1 year after diagnosis, 15% between 1 and 3 years after diagnosis, 9% between 4 and 6 years after diagnosis and 9% had spent 6 or more years after diagnosis. The patients had surgery and radiotherapy (37%), radiotherapy and chemotherapy (27%), surgery (14%), chemotherapy (13%), radiotherapy and surgery (6%), radiotherapy (3%). About one-fifth of the patients (31%) reported a cancer recurrence in the years following diagnosis. This study was granted ethical approval by ethical committee of Department of Psychology, Ferdowsi University of Mashhad.
2.2. Research Tools
1) Short form of the cognitive emotion regulation questionnaire: this multi-dimensional questionnaire has been developed to identify the cognitive coping strategies of individuals after experiencing adverse events or situations (24). The questionnaire consists of 18 items and evaluates 9 subscales of cognitive strategy, including blaming themselves, acceptance, rumination, positive refocusing, refocusing on planning, positive reassessment, perspective taking, catastrophizing, and blaming others using a 5-point Likert scale (1 = almost never to 5 = almost always). The validity of this questionnaire and its reliability was obtained by Cronbach’s alpha coefficients for subscales from 0.68 to 0.86 (25). In a previous study, the Cronbach’s alpha coefficients were reported from 0.62 to 0.80 (13).
2) The world health organization quality of life scale: this scale is designed to assess the quality of life. A short form of this questionnaire includes 26 questions and evaluates the 4 domains: physical health, psychological health, social relationships, and environment. After performing the necessary calculations in each domain, a score of 4 to 20 was obtained separately, where 4 indicated the worst and 20 indicated the best condition in the given domain (world health organization quality of life) (26). The validity of the questionnaire has been established in the country and its reliability was obtained, using Cronbach’s alpha coefficients from 0.55 to 0.84 (27).
3) NEO 5 factor personality: this tool is the most widely used one in the field of personality assessment and enjoys broad empirical support. The questionnaire was set with 60 items scored by a 5-point Likert scale (1, completely agree and 5, completely disagree) and each of the big 5 personality characteristics was measured by 12 items (extraversion, agreeableness, conscientiousness, neuroticism, and openness to experience) (28). The validity of this questionnaire was established in the country (29) and its reliability was tested, using Cronbach’s Alpha coefficient, giving the results 0.56 to 0.87 (30).
4) Scale of goal adjustment: this scale includes 10 questions scored by a 5-point Likert scale (Totally disagree = 1 to strongly agree = 5). The scale consists of 2 subscales including ‘withdrew from the target’ (4 items), and ‘recommitment to this goal’ (6 questions). Its reliability was estimated at from 0.76 to 0.84 (23). The content validity of the scale was approved by the professors at Ferdowsi Psychology University of Mashhad. In this study, Cronbach’s Alpha was 0.72.
2.3. Statistical Methods
The statistical analyses were performed, using SPSS v. 19 with LISREL v. 8.5.
3. Results
In this section, the descriptive statistics of the research variables are presented. Based on the correlation coefficients in Table 1, the relationship between adaptive strategies of cognitive emotion regulation with goal adjustment was the strongest relationship and maladaptive strategies of cognitive emotion regulation with extraversion were the weakest one. Also, there was no significant relationship between the 3 dimensions of personality, openness, agreeableness, and conscientiousness and any of the mediators or endogenous variables.
| Statistical Indicators | M ± SD | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 |
|---|---|---|---|---|---|---|---|---|---|---|
| 1- Neuroticism | 35.37 ± 12.87 | 1 | ||||||||
| 2- Extraversion | 50.43 ± 3.47 | 0.13 | ||||||||
| 3- Opening | 26.78 ± 3.69 | -0.08 | 0.17a | 1 | ||||||
| 4- Agreeableness | 30.48 ± 5.13 | -0.08 | 0.13 | 0.08 | 1 | |||||
| 5-Conscientiousness | 32.41 ± 5.24 | 0.03 | 0.10 | 0.10 | 0.47b | 1 | ||||
| 6- Adaptive strategies | 51.34 ± 30.35 | -0.50b | 0.60b | -0.09 | 0.08 | 0.04 | 1 | |||
| 7- Maladaptive strategies | 63.92 ± 31.63 | 0.33b | -0.15a | -0.07 | 0.16 | -0.17 | -0.25b | 1 | ||
| 8- Goal adjustment | 34.89 ± 15.82 | -0.55b | 0.58b | -0.05 | 0.11 | 0.07 | 0.93b | -0.62b | 1 | |
| 9- Quality of life | 114.85 ± 16 | -0.80b | 0.20a | 0.02 | 0.10 | 0.06 | 0.62b | -0.61b | 0.69b | 1 |
The Correlation Matrix of Variables
3.1. Given Causal Model Test
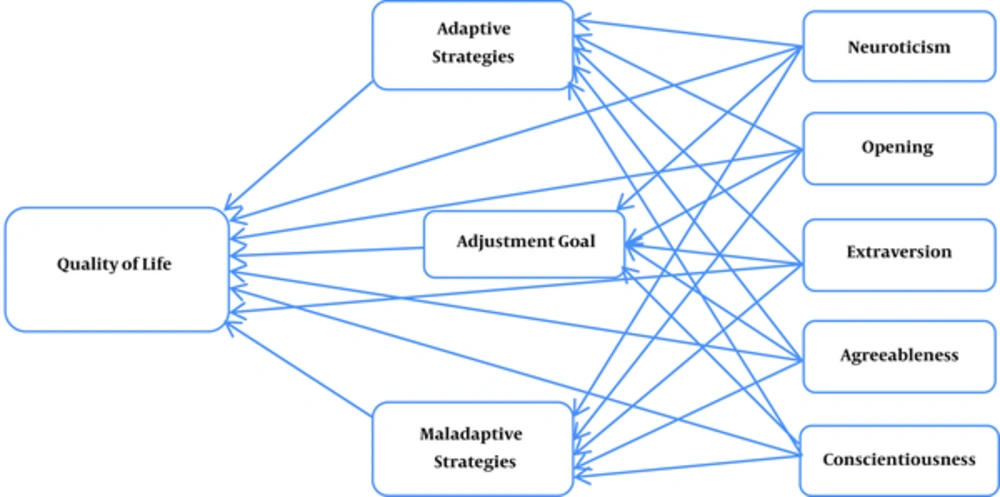
The proposed model in Figure 1 was used to test this model and path analysis.
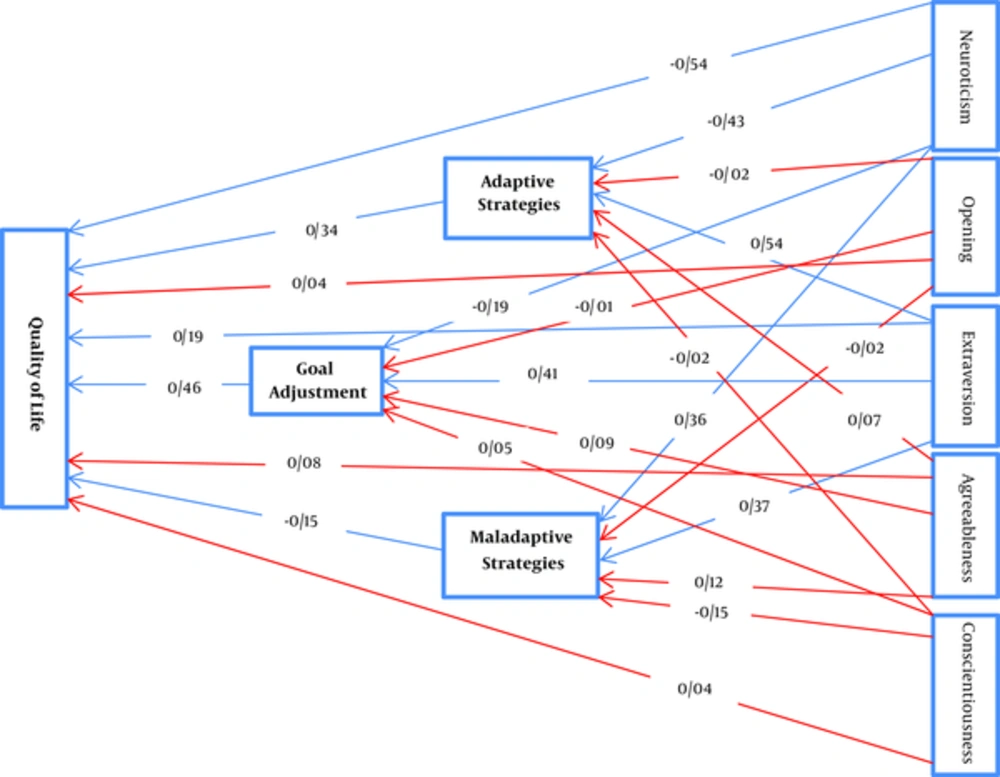
The suitability of the proposed model was tested, using Chi-square, comparative fitness index (CFI), goodness of fit index (GFI), adjusted goodness of fit index (AGFI), and root mean square error of approximation (RMSEA). The results of the initial tests of the proposed model indicated a lack of fit, as can be seen in Figure 2.
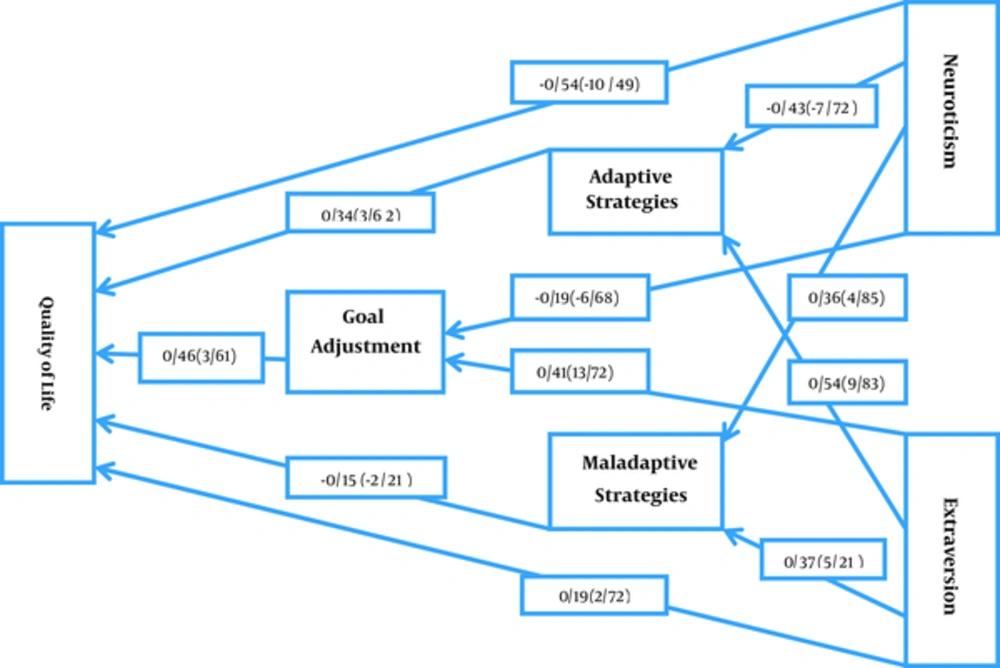
Several adjustments were made based on the theoretical and experimental principles to adjust the initial model. The overall indices of the adjusted model in Table 2 shows the overall fit of the model (X2 = 129.71, df = 98, GFI = 0.82, AGFI = 0.82, GFI = 0.87, RSMEA = 0.082).
| Indicators | CFI | AGFI | GFI | RMSA | χ2/df | Df | χ2 |
|---|---|---|---|---|---|---|---|
| Results | 0.82 | 0.82 | 0.81 | 0.082 | 1.32 | 98 | 129.71 |
Goodness of Fit Indicators for the Proposed Model
The final proposed model can be seen in Figure 3.
All path coefficients of the exogenous variables (neuroticism and extraversion) were significant to mediator variables (adaptive strategies, maladaptive strategies, and goal adjustment) and the endogenous variable (quality of life) (P < 0.05). All the path coefficients of the intermediate variables (adaptive strategies, maladaptive strategies, and goal adjustment) were significant to endogenous variable (quality of life). In the adjusted model, the neuroticism variable had the highest negative direct effect on quality of life and the extroversion variable had the greatest positive direct effects on cognitive emotion regulation strategies. Also, among the variables, the neuroticism pattern had the greatest overall effect on quality of life.
4. Discussion
This study was conducted with the aim of investigating the mediating effect of cognitive emotion regulation strategies and goal adjustment on the role of personality characteristics in the quality of life of patients with cancer. To examine the research hypothesis- personality characteristics mediate the cognitive emotion regulation strategies and goal adjustment in the life quality of cancer patients- a theoretical model was proposed and tested, using a path analysis method. The results of the proposed model indicated the lack of fit of the model. Hence, to fit indicators for primary model, several adjustments were made based on the theoretical and experimental principles. The model was finally approved. In the adjusted model, the neuroticism variable had the greatest negative direct effect on quality of life and the extroversion variable had the greatest positive effect on cognitive emotion regulation strategies. Also, among the variables of the model, neuroticism had the greatest overall effect on quality of life. Supporting this finding, we can say that most studies on personality dimensions have focused on 2 aspects, namely neuroticism and extroversion. In fact, it seems that both dimensions were significant predictors of stress and coping style on people (9, 13, 31, 32), but other personality dimensions (openness, agreeableness, and conscientiousness) were not significant predictors. Fit statistics of life quality in patients with cancer indicated the suitability of the model and, hence, the proposed modified model was an appropriate predictor for quality of life in patients with cancer. No previous study has produced a model that predicts the relationships between these factors. The proposed model in this study is consistent with the models presented in other studies (4, 18, 31, 33).
The direct effect of neuroticism on quality of life was greater than the indirect effect of this variable, which is consistent with previous research (8, 34). In fact, neuroticism can increase an individuals’ readiness to experience stressor events and make them prone to experience negative emotions and frustration (35). These features make a person vulnerable, especially in the domain of personal and social relationships. Neuroticism, by increasing negative feelings and frustration, causes people to fail to use their cognitive and communicative capabilities calmly and confidently to assess their feelings and emotions and, thereby, they undermine their health and quality of life. Considering the fact that anxiety and depression are factors reducing the quality of life, it seems unsurprising that neuroticism is negatively associated with quality of life.
Also, extroversion has a direct effect on quality of life greater than the indirect effect of this variable, which is consistent with the findings of previous researchers (36). Character is the most powerful and stable predictor of mental health. Among personality characteristics, extraversion seems important in predicting positive affect, and it increases the likelihood of experiencing positive emotions in social situations; so, it is associated with mental health and quality of life. In fact, extroversion enhances the experience of enjoyable events and positive emotions through strengthening a person’s social relations and emotions, and in this way, it helps the person to use communication and cognitive abilities to assess their emotions and feelings in a more relaxed and optimistic manner and use it to reduce possible stressors and worrying conditions such as cancer.
The significant indirect positive effect of extroversion on the life quality of cancer patients through the mediating adaptive strategies of cognitive emotion regulation suggests that people with high extraversion characteristics follow active coping strategies and seek social support in dealing with stressor conditions such as cancer, and experience more enjoyable events. So, this will improve their quality of life. This finding is consistent with previous research results (8). Survey results have also shown that extroverted people tend to use more adaptive forms of coping, such as seeking social support, positive thinking or reinterpretation, subrogation, and control (9). In fact, the coping style that extroverted people use when faced with stress increases their positive emotions and reduces negative emotions.
Moreover, the significant indirect negative effects of neuroticism on the quality of life of patients with cancer by mediating the maladaptive strategies of cognitive emotion regulation are consistent with several studies (29, 37). These findings indicate that individuals with high neuroticism features in dealing with the stressor conditions like the experience of cancer follow passive and ineffective coping strategies and also experience more negative events. Thus, this leads to a reduction in their quality of life. In other words, individuals with high neuroticism when faced with stressor events use passive strategies, such as avoidance, self-blame, wishful thinking, practices based on interpersonal pugnacity such a hostile response, and evacuation of negative emotions. Therefore, the higher levels of neuroticism intensify the experience of negative emotions and reduce health and quality of life.
Moreover, goal adjustment had a positive effect on the quality of life of patients with cancer. These results are consistent with previous research, demonstrating a lack of appropriate targeting of reduced quality of life and a positive meaning in life by following significant goals (18). A chronic disease such as cancer may strongly interfere with achieving specific health goals, having a sense of confidence and competence, being able to perform daily activities, and sense of connection with others. It can be assumed that under such circumstances, it is recommended that patients stop the pursuit of unattainable goals and invest time and effort in meaningful goals that are achievable. Therefore, health care professionals who work with patients with cancer can help them by assisting them to identify and establish new achievable and meaningful goals.
Finally, the positive relationship of adaptive strategies of Cognitive Emotion Regulation and the negative relationship of maladaptive strategies of cognitive emotion regulation on the quality of life of patients with cancer is consistent with the findings of previous research (38). These findings may indicate that the cognitive emotion regulation strategies used by patients with cancer are important for their health in adjusting their emotions. Thus, patients who are more able to think about pleasant topics, instead of thinking about the cancer experience, and those who consistently do not ruminate negative feelings or think about experiences associated with cancer, have s better physical and mental health condition (39). In fact, using adaptive strategies causes patients to assess negative events with a different view and attend to positive aspects and their potential benefits in the long-term; as a result, they experience less stress and discomfort and deal with events better. Also, the use of maladaptive strategies makes patients with cancer prone to anxiety and instead of responding appropriately to stressor events, reacts to them with anxiety (13). This finding can be explained by cognitive coping styles that are closely related to the cognitive emotion regulation strategies. In this context, problem-focused skills are included in cognitive skills that are assessed according to the location, evaluation, emotion, and objectification of emotions and cause the patient to take a more realistic view. So, the more patients use effective coping strategies, the more they show the psychological and physical symptoms of anxiety, inability to feel pleasure or satisfaction in life, and well-being, and the positive affect will be higher.
In conclusion, our findings could have implications for the health care providers that are connected to patients with cancer. It should be noted that 2 major factors affecting the quality of life of patients with cancer are goal adjustment and Cognitive Emotion Regulation Strategies. Therefore, treatment programs should pay special attention to education of goal adjustment and cognitive strategies, especially adaptive strategies. Training goal adjustment for patients with cancer to encourage them to abandon unattainable goals and re-engage with meaningful purpose in life can help them find positive meaning in their lives. On the other hand, training the emotion regulation for patients with cancer causes them to reduce their negative emotions by knowing their emotions, correct usage, and adoption of them, and express their emotions, especially positive emotions in life situations, and consequently reduce the level of their physical symptoms.
Limitations of this study include prolongation of response to the questionnaire due to physical condition of patients receiving chemotherapy, including drowsiness, nausea, and lethargy. Since in the quality of life model, developed in this study, neuroticism had the most negative effect on the quality of life of patients with cancer, it is suggested that psychological interventions be made to reduce neuroticism and, subsequently, improve the quality of life of this group.