1. Background
Although there are numerous medicines used in cancer treatment, the major problem is differentiating cancer cells from healthy ones to reduce collateral toxicity to healthy cells (1).
Nanomedicine, utilizing different methods and materials such as nanocarriers, can potentially advance cancer management by developing the therapeutic behavior of active pharmaceutical ingredients (2). Despite great advances in the field of cancer nanomedicine, various clinical challenges are still present in clinical translation (3). As a result, a new generation of nanomedicine is a vital requirement to tackle existing problems (4).
Health-related quality of life (HRQOL) is recognized as a clinical parameter in cancer patients and various methods are applied to measure the quality of life (QOL), including the European Organization for Research and Treatment of Cancer (EORTC QLQ-C30) questionnaire, which reports C30 index score (5, 6). This questionnaire contains 30 items evaluating functional domains (role, social, physical, cognitive, and emotional), symptom scales (fatigue, nausea, and pain), single items (dyspnea, sleep disturbances, appetite loss, constipation, diarrhea and financial impact of disease, and treatment), and a single global QOL scale (7, 8).
Nanochelating technology (9), as a branch of nanotechnology (10), has recently been able to introduce a nanomedicine without carriers, BCc1 nanomedicine, in cancer treatment. The previous studies revealed that the optimal dose of this nanomedicine, with a size of 44 nm, creates apoptosis in cancer cells without any side effect in healthy cells (11). In addition, the mixture of this nanomedicine (high dose) with doxorubicin (low dose) showed a synergistic effect leading to an increase in life span, although the applied doxorubicin dose was almost 50 times less than its routine dose (12). The application of this nanomedicine in a clinical trial has already revealed that gastric patients treated by BCc1 nanomedicine significantly enjoyed higher overall survival than placebo (13). In the same study, the QOL of the very same patients was assessed, using the EORTC QLQ-STO22 questionnaire (14).
2. Objectives
In the present study, we aimed at investigating the QOL according to the EORTC QLQ-STO30 questionnaire before and after treatment with BCc1 nanomedicine in metastatic and non-metastatic gastric cancer patients, and also assess the synergistic effect between EORTC QLQ-STO30 questionnaire and EORTC QLQ-STO22 questionnaire.
3. Methods
3.1. Design and Data Collection
A randomized, double-blind, placebo-controlled and parallel trial was carried out at Cancer Research Center of Shahid Beheshti University of Medical Sciences. The current clinical trial study was designed based on two groups of patients with adenocarcinoma gastric cancer (metastatic and non-metastatic), separately divided into two sub-groups (BCc1 nanomedicine and placebo). The patients were selected from 6 various oncology centers; Firouzgar, Naft Company, Imam Reza, Bu Ali, Shahid Fayaz Bakhsh, and Shohadaye Tajrish Hospitals in Tehran, Iran.
Recruitment, randomization, allocation, and sample collection were performed according to the previous study (13), then, all the patients signed the written consent form dictated by the Ethics Committee of Shahid Beheshti University of Medical Sciences after they were briefed on the pros and cons of BCc1 nanomedicine.
3.2. Patients’ Characteristics
The patients’ characteristics, both metastatic and non-metastatic, are thoroughly explained in the previous study (13).
3.3. Quality of Life Assessment
The main goal of the current study was QOL assessment of metastatic gastric cancer patients (before treatment and 8 weeks after treatment) and non-metastatic gastric cancer patients (before treatment and 20 weeks after treatment) according to EORTC QLQ-STO30 questionnaire.
3.4. Sample Size
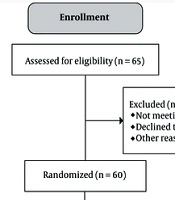
Totally, 120 gastric cancer patients were randomly recruited for the present study, and they were divided into two groups, namely metastatic (60 patients, Figure 1) and non-metastatic (60 patients, Figure 2).
3.5. BCc1 Nanomedicine
The synthesis of BCc1 nanomedicine was performed in Sodour Ahrar Shargh Company based on “chelate compounds” patent (9) and placebo capsules were provided from Tehran Darou Pharmaceutical Co. The shape and size of BCc1 nanomedicine and placebo capsules were exactly identical. During the study, 3000 mg/per day of BCc1 nanomedicine was given to metastatic patients and 1500 mg/per day was given to non-metastatic patients.
3.6. Statistical Methods
The mean scores of all patients were computed and compared between the two groups (BCc1 nanomedicine and placebo), using the paired-samples t-test (parametric statistic) and Wilcoxon signed ranks test (non- parametric statistic). A P value of ≤ 0.05 was regarded as significant for covariate selection. All analyses were carried out by SPSS software (version 25; SPSS Inc., Chicago, IL, USA) (15).
4. Results
As shown in Table 1, the mean difference of global QLQ-STO30 was 73.27 ± 14.12 before the treatment in all the metastatic patients, who took BCc1 nanomedicine with and without chemotherapy, while it was 70.17 ± 12.49 after the treatment; the results showed an overall QOL improvement of 2.86 (P = 0.03). On the contrary, the mean difference of global QLQ-STO30 was 73.63 ± 14.12 before the treatment in all the metastatic patients, who took placebo with and without chemotherapy, while it was 78.84 ± 11.73 after the treatment; the results showed an overall QOL deterioration of 5.21 (P = 0.04).
| Mean | Std. Deviation | Std. Error | Sig. | |
|---|---|---|---|---|
| QLQ-STO30 in Metastatic Gastric Cancer Patients | ||||
| Global QOL (BCc1 nanomedicine) | ||||
| Before | 73.27 | 14.125 | 2.039 | |
| After | 70.17 | 12.499 | 2.321 | |
| Global QOL (placebo) | ||||
| Before | 73.63 | 14.291 | 3.279 | |
| After | 78.84 | 11.739 | 2.693 | |
| Median Difference (Before-After) | ||||
| Overall QOL (BCc1 nanomedicine) | -2.862b | 6.797 | 1.262 | 0.031 |
| Overall QOL (placebo) | 5.211b | 10.602 | 2.432 | 0.046 |
aA P value of ≤ 0.05 was regarded as significant for covariate selection.
bLower scores show a better global quality of life.
As shown in Table 2, the mean difference of global QLQ-STO30 was 71.73 ± 14.11 before the treatment in all the non-metastatic patients, who took BCc1 nanomedicine with and without chemotherapy, while it was 69.35 ± 12.41 after treatment; the results showed an overall QOL improvement of 2.38 (P = 0.25). On the contrary, the mean difference of global QLQ-STO30 was 71.53 ± 12.54 before the treatment in all the non-metastatic patients, who took placebo with and without chemotherapy, while it was 74.53 ± 11.26 after treatment; the results showed an overall QOL deterioration of 3 (P = 0.09).
| Mean | Std. Deviation | Std. Error | Sig. | |
|---|---|---|---|---|
| QLQ-STO30 in Non-Metastatic Gastric Cancer Patients | ||||
| Global QOL (BCc1 nanomedicine) | ||||
| Before | 71.73 | 14.110 | 2.767 | |
| After | 69.35 | 12.416 | 2.435 | |
| Global QOL (placebo) | ||||
| Before | 71.53 | 12.540 | 2.877 | |
| After | 74.53 | 11.266 | 2.585 | |
| Median Difference (Before-After) | ||||
| QOL (BCc1 nanomedicine) | -2.385b | 10.439 | 2.047 | 0.255 |
| QOL (placebo) | 3.000b | 7.461 | 1.712 | 0.097 |
aA P value of ≤ 0.05 was regarded as significant for covariate selection.
bLower scores show a better global quality of life.
As shown in Table 3, in the metastatic patients, who simultaneously took BCc1 nanomedicine and received chemotherapy, the mean difference of global QLQ-STO30 was 73.77 ± 12.77 before the treatment, while it was 69.62 ± 11.55 after the treatment; the results indicated an overall QOL improvement of 4.15 (P = 0.05). On the contrary, in the metastatic patients, who simultaneously took a placebo and received chemotherapy, the mean difference of global QLQ-STO30 was 74.77 ± 12.77 before the treatment, while it was 77.50 ± 11.86 after the treatment; the results indicated an overall QOL deterioration of 2.66 (P =s 0.37).
| Mean | Std. Deviation | Std. Error | Sig. | |
|---|---|---|---|---|
| QLQ-STO30 in Metastatic Gastric Cancer Patients (Patients Received Intervention and Chemotherapy Simultaneously) | ||||
| Global QOL (BCc1 nanomedicine) | ||||
| Before | 73.77 | 12.775 | 3.543 | |
| After | 69.62 | 11.558 | 3.206 | |
| Global QOL (placebo) | ||||
| Before | 74.83 | 13.496 | 3.896 | |
| After | 77.50 | 11.867 | 3.426 | |
| Median Difference (Before-After) | ||||
| Overall QOL (BCc1 nanomedicine) | -4.15b | 6.866 | 1.904 | 0.05 |
| Overall QOL (placebo) | 2.66b | 9.976 | 2.880 | 0.37 |
aA P value of ≤ 0.05 was regarded as significant for covariate selection.
bLower scores show a better global quality of life.
As shown in Table 4, in the non-metastatic patients, who simultaneously took BCc1 nanomedicine and chemotherapy, the mean difference of global QLQ-STO30 was 71.73 ± 15.31 before the treatment, while it was 71.00 ± 17.90 after the treatment; the results indicated an overall QOL improvement of 0.72 (P = 0.716). On the contrary, in the non-metastatic patients, who simultaneously took placebo and chemotherapy, the mean difference of global QLQ-STO30 was 77.10 ± 9.12 before the treatment, while it was 78.20 ± 11.15 after the treatment; the results indicated an overall QOL deterioration of 2.1 (P = 0.43).
| Mean | Std. Deviation | Std. Error | Sig. | |
|---|---|---|---|---|
| QLQ-STO30 in Non-Metastatic Gastric Cancer Patients (Patients Received Intervention and Chemotherapy Simultaneously) | ||||
| Global QOL (BCc1 nanomedicine) | ||||
| Before | 71.73 | 15.317 | 4.618 | |
| After | 71.00 | 17.905 | 5.399 | |
| Global QOL (placebo) | ||||
| Before | 77.10 | 9.122 | 2.885 | |
| After | 78.20 | 11.153 | 3.527 | |
| Median Difference (Before-After) | ||||
| Overall QOL (BCc1 nanomedicine) | -4.15b | 6.866 | 1.904 | 0.05 |
| Overall QOL (placebo) | 2.1b | 8.117 | 2.567 | 0.434 |
aA P value of ≤ 0.05 was regarded as significant for covariate selection.
bLower scores show a better global quality of life.
As shown in Table 5, in the metastatic patients, who took BCc1 nanomedicine without chemotherapy, the mean difference of global QLQ-STO30 was 73.29 ± 16.12 before the treatment, while it was 71.14 ± 13.57 after the treatment; the results showed an overall QOL improvement of 2.14 (P = 0.28). On the contrary, in the metastatic patients, who took placebo without chemotherapy, the mean difference of global QLQ-STO30 was 71.57 ± 16.46 before the treatment, while it was 81.14 ± 12.06 after the treatment; the results showed an overall QOL deterioration of 9.57 (P = 0.06).
| Mean | Std. Deviation | Std. Error | Sig. | |
|---|---|---|---|---|
| QLQ-STO30 in Metastatic Gastric Cancer Patients (Patients Only Received BCc1 Nanomedicine or Placebo) | ||||
| Global QOL (BCc1 nanomedicine) | ||||
| Before | 73.29 | 16.127 | 4.310 | |
| After | 71.14 | 13.575 | 3.628 | |
| Global QOL (placebo) | ||||
| Before | 71.57 | 16.461 | 6.222 | |
| After | 81.14 | 12.061 | 4.559 | |
| Median Difference (Before-After) | ||||
| Overall QOL (BCc1 nanomedicine) | -2.143b | 7.188 | 1.921 | 0.285 |
| Overall QOL (placebo) | 9.571b | 10.937 | 4.134 | 0.060 |
aA P value of ≤ 0.05 was regarded as significant for covariate selection.
bLower scores show a better global quality of life.
As shown in Table 6, in the non-metastatic patients, who took BCc1 nanomedicine without chemotherapy, the mean difference of global QLQ-STO30 was 73.14 ± 13.04 before the treatment, while it was 67.93 ± 6.71 after the treatment; the results showed an overall QOL improvement of 5.21 (P = 0.113). On the contrary, in the non-metastatic patients, who took placebo without chemotherapy, the mean difference of global QLQ-STO30 was 65.86 ± 16.45 before the treatment, while it was 70.86 ± 12.02 after the treatment; the results showed an overall QOL deterioration of 5 (P = 0.13).
| Mean | Std. Deviation | Std. Error | Sig. | |
|---|---|---|---|---|
| QLQ-STO30 in Non-Metastatic Gastric Cancer Patients (Patients Only Received BCc1 Nanomedicine or Placebo) | ||||
| Global QOL (BCc1 nanomedicine) | ||||
| Before | 73. 14 | 13.049 | 3.488 | |
| After | 67.93 | 6.719 | 1.796 | |
| Global QOL (placebo) | ||||
| Before | 65.86 | 16.456 | 6.220 | |
| After | 70.86 | 12.020 | 4.543 | |
| Median Difference (Before-After) | ||||
| Overall QOL (BCc1 nanomedicine) | -5.214b | 11.464 | 3.064 | 0.113 |
| Overall QOL (placebo) | 5.00b | 7.746 | 2.928 | 0.139 |
aA P value of ≤ 0.05 was regarded as significant for covariate selection.
bLower scores show a better global quality of life.
5. Discussion
According to the statistics report of the American Cancer Society in 2015, the overall US mortality from all cancers had decreased to 26% over the period between 1990 and 2015 (16). However, scientific studies are consistently being conducted to treat all kinds of cancer more efficiently (17, 18).
HRQOL (19) is currently considered a prominent evaluation criterion during the treatment of malignancy forms including cancers; so, it is regarded as an assessment index in the treatment of these patients. In a study, Leung Li reported that the QOL (assessed using EORTC QLQ-C30, QLQ-HCC18, C30 index score, or HCC18 index score) is correlated with liver function in hepatocellular carcinoma (HCC) patients (6). In another study, Sadighi proved that docetaxel-based treatments show better global QOL compared with epirubicin-based treatments (20).
It is already proved that the application of nanomedicines (21) in the field of cancer transforms therapeutic agents in a way that they selectively attack diseased cells. This transformation from active pharmaceutical ingredient to nanostructures is extremely varied with potential applications so as to boost the drug delivery system in the selected drugs. However, reproducible and large-scale synthesis of nanomedicine still remains a challenge to distribute a homogeneous batch of nanomedicines, especially with regard to the fact that these nano-platforms often need special conditions to be produced through self-assembly (22).
Nanochelating technology, as a new method, has proved to have a significant impact on the treatment of various diseases by synthesizing different nanostructures with effective properties, using controlled self-assembly methods (23-25). For instance, BCc1 nanomedicine with chelating properties and dominant affinity for iron elements have high potentials to induce therapeutic behavior for the treatment of cancer (26).
Gastric cancer (27) is among the 5 prevalent cancers in both males and females in Iran, and unfortunately, owing to the delayed visits to specialists, the disease progression in these patients is high and consequently their overall survival is low (28, 29). Due to this fact, the first clinical trial study on BCc1 nanomedicine was conducted on these patients. Considering the apoptosis mechanism of BCc1 nanomedicine in killing cancer cells, the results of an 18-month follow-up in this study showed that the overall survival in BCc1 nanomedicine group was significantly higher without leaving any side effect on the patients, such as nausea, diarrhea, vomiting, and anomie (13).
In the current study, the QOL in metastatic and non-metastatic gastric cancer patients was assessed after the treatment with BCc1 nanomedicine according to the EORTC QLQ-STO30 questionnaire. The results of the study implicated that the patients, who received BCc1 nanomedicine in their therapeutic regime, significantly enjoyed higher QOL.
In the previous study, the assessment of the QOL by EORTC QLQ-STO22 questionnaire showed a mean difference improvement of 3.25 (metastatic patients) and 2.29 (non-metastatic patients) in BCc1 nanomedicine group despite a mean difference decline of 4.42 (metastatic patients) and 3 (non-metastatic patients) in the placebo group. The results of the EORTC QLQ-STO30 questionnaire analysis in the present study confirm the results of the EORTC QLQ-STO22 questionnaire conducted in the previous study; therefore, it can be claimed that using BCc1 nanomedicine in gastric cancer patients can improve their QOL.
As the present study was designed based on the randomized and double-blind method (30), BCc1 nanomedicine and placebo capsules had to be prescribed without interfering in the physicians’ protocol, and as a result, some patients received chemotherapy and some not. Therefore, an analysis was performed to evaluate the QOL of the patients, who received BCc1 nanomedicine or placebo without chemotherapy, the results of which indicated an improvement in the QOL of these patients supporting the hypothesis that BCc1 nanomedicine can be introduced as an independent nanomedicine in cancer treatment after some further studies in the future.