1. Context
One of the problems of health systems all around the world is the increase in cancer load and its incidence rate, which is a serious threat to people’s health (1, 2). Cancer is one of the major causes of mortality around the world (2-4). According to the World Health Organization (WHO), the cancer incidence rate is expected to increases 10 to 15 million new cases from 2000 to 2020 (1, 2). More than 90% of patients with fatal diseases including cancer have the dream of a peaceful death in an environment similar to their home. However, even in developed countries, only 20% to 30% of patients die at home, and according to Higginson et al., it is estimated that by 2030, this amount will decrease to 10% (5). Many patients with cancer are admitted to hospitals to receive specialty care, and after receiving specialized and costly care, pass away without obtaining the desirable results, after experiencing a lot of pain. But, unfortunately, for most patients with cancer, death is inevitable in many cases despite applying advanced therapies and modern technologies for treating these diseases. Therefore, today, the main approach to taking care of these patients is to provide supportive and palliative care (6).
Palliative care has rapidly expanded in the United Kingdom (UK) since the late 1960s (7). In May 2005, the World Health Assembly mandated that all countries design and implement national cancer control programs. Accordingly, cancer support and palliative care are considered one of the 6 principles of cancer control programs in every country (8). The WHO recommended to all countries to prioritize these care services in their public health programs (9). Moreover, this organization believes that countries should have appropriate policies and a systematic framework for implementing these services in their health systems based on the available resources (10). According to the estimations made by the WHO, about 80% of those in need of care need only primary and non-specialized care, and only 20% of them need specialized care (11).
Palliative and supportive care are provided with regard to the specific condition of the patient, increasing QOL in dying patients with a comprehensive, patient-oriented, multidimensional, and humanistic approach, a concept that has mostly been ignored in providing health services (12, 13). The results of a study in 2007 showed that patients, who were provided with care at supportive and palliative care centers, lived 29 days longer than other similar patients (14). On the other hand, researchers also pointed out that supportive and palliative care can reduce the cost of treatment and health care (15-17). While many high-income countries have developed and implemented national policies to provide cancer supportive and palliative care (18-20), many middle and lower-income countries still have no policy and plan at local and national levels despite the high burden of the disease (21). In 2004, the first international resolution was issued in the field of palliative care (WHA 67.19) (22).
The member states of the WHO demanded evidence-based tools to integrate palliative care into national health systems. For this purpose, the WHO’s practical guideline was developed. This guideline explains how to plan and implement palliative care services at the national or international level through a step-by-step approach for low and middle-income countries. The chapters of this guideline include stewardship/policy actions, workforce, health care financing, service delivery, information and research, and access to medicines (22). In all countries, the care delivery approach is an important issue, and policymakers and health care decision-makers are trying to provide the highest quality care as one of the basic priorities of each country’s health system, depending on the available resources (23). The provision of these services requires integrating and merging these services with the existing infrastructure of the health system, as well as considering the financial and human resources in the service delivery structure (24).
Many studies show that palliative care policies and the integration of these services in each country’s health system can bring about benefits such as reducing undesired hospitalization, improving the quality of life (QOL), increasing the rate of survival, and reducing the economic burden of cancer on the shoulders of the patients’ families and the health system (25-28). Despite many international recommendations around providing palliative care services from the very beginning of the disease and the integration of these services with the health system of each country, there are still many obstacles to achieve this important goal (29). Although the integration of palliative care in the early stages of cancer is routinely a part of the standard procedure in many countries such as Britain, in many developing countries such as Iran, palliative care services are in the early stages and their referral systems are very different from the ones in western countries (27, 30). In Iran, palliative care is a new concept, and there is no codified policy to provide such specialized services according to the demands, and there are only a few centers providing these services (31).
Palliative care is provided sporadically and is not efficiently protected by the health system, and the patients usually do not receive the necessary care. The existence of organized care programs and the integration of these services into the health system of the country are considered unmet needs (32). Since the application of an appropriate model in each care system depends on the health status and with regard to the economic situation, as well as the cultural and social status of the country, it is not possible to mention a set of fixed and pre-arranged goals for palliative care systems in the world (31). Therefore, the best choice can be made based on successful global experiences, studying the needs, considering the specific conditions of the country and, consequently, the policies of the health system of the society. Health policymakers play a significant role in the realization of this important goal (33). This study was conducted with the aim of comparing the policies and the strategies related to cancer supportive and palliative care in the selected countries, using the WHO practical guideline in order to assess the advantages, weaknesses, and limitations of these plans.
1.1. Conceptual Framework
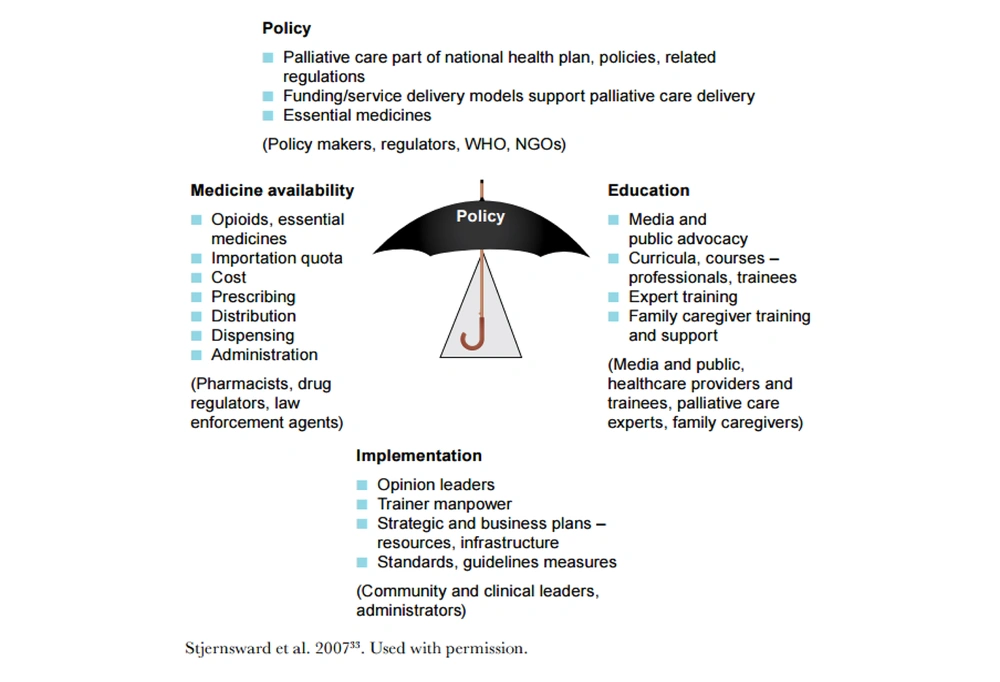
The present study is based on the conceptual framework of “The World Health Organization Guide” with the approach of integrating palliative care in the health system (2014). This guide includes 6 policy orientations (development planning strategies), health system funding (development costs), service providers (hospitals, home care, etc.), human resources development (training programs), access to medicines (the rules and the access to medicines, especially opiates), and finally, information and research (evaluating information systems, multidisciplinary studies). At the stage of integration into the health system, each orientation has been classified into basic, moderate, and advanced levels (22). Palliative care program development has been subjected to many changes internationally; it is correlated with Human Development Index levels. Without policy support for palliative care and funding mechanisms, the development will be limited to what has been achieved by the pioneers’ devotion to building hospices and palliative care service centers in their communities (34). The public health model for palliative care development is shown in Figure 1.
2. Evidence Acquisition
This study is a comparative study carried out to analyze the policies of cancer supportive and palliative care in various countries around the world. The studied countries were purposefully selected based on the reports of the economist intelligence unit, which studies the status of palliative care in 80 countries around the world, and classified as the countries by taking into account 20 quantitative and qualitative indicators in 5 classes, including healthcare and palliative care environment, care affordability, human resources, care quality, and society engagement. Accordingly, based on the availability of information and the existence of government services for examining the pattern of palliative care services, the selected countries are as follow: the UK from the group 4b with an approach to integrating services; Malaysia from the group 4a with generalized palliative care provision in some areas of the country; and South Africa from the group 4a with isolated palliative care provision in some areas. On the other hand, each of the studied countries is located in one of the 6 regions of the WHO. The UK is considered a developed and advanced country, Malaysia as a developing and pioneer country in Asia, and South Africa as a developing and pioneer country in Africa.
The data were collected through reviewing scientific and administrative documents, WHO website and reports, government websites (UK, Malaysia, and South-Africa), and other authoritative websites. The search was done through texts in English and the databases, including Science Direct, Scopus, and PubMed between 2000 and December 2018. In order to review the content of the policies and the strategies related to cancer supportive and palliative care, the WHO guideline is used, which is based on the integration of palliative care into the health system and includes stewardship/policy actions, workforce, health care financing, service delivery, information and research, and access to medicines (22) compared in the selected countries. The contents of the documents are analyzed based on the 5 chapters of this guideline, which are presented in Table 1.
| Component | UK | Malaysia | South Africa |
|---|---|---|---|
| Stewardship/policy actions | The Ministry of Health is responsible for providing palliative care protocols and guidelines. | The Ministry of Health plans public health and medical care programs but has little legal power in the private sector. | Providing palliative care services mainly through charity centers or the National Palliative Care Association |
| 1991- The formation of the National Council for Hospice and Palliative Care Services, renamed to the National Council for Palliative Care in 2004 | Major palliative care services are provided by the charity and non-profit sectors. | 2016 - Approving a policy framework for palliative care | |
| The responsibility of the health and its public policies in the UK is given to the Parliament, the Ministry of Health, and the National Health Service. | |||
| 1970- The establishment of the National Hospice Organization supervised by National Health Service | |||
| 1995- The establishment of the first palliative care unit at Queen Elizabeth Hospital | |||
| 2004- Designing a national program for the development of palliative care | |||
| 2008- Developing end-of-life strategies and launching a national strategy for children’s palliative care | |||
| The UK Foreign Office has a legal duty to promote comprehensive health services. | |||
| Issuing an executive order by the government, on the necessity of palliative care provision for any life-limiting illness | |||
| The integration of palliative care into the health system | |||
| Workforce | The first country to have palliative care | 2016- 18 trained palliative care experts | Offering palliative care education at various levels, and by various organizations such as the University of Cape Town |
| Pioneer in the field of palliative medicine | Developing an advanced Diploma Program for nurses, physiotherapists, and therapists | Most hospices relying on professional volunteers | |
| 6000-7000 palliative care specialists, about 5000 nurses, 750 physicians, and 70000 social volunteers | Training 38 nurses and federal specialists | ||
| Palliative care academic and higher education centers such as Cicely-Saunders Institute | Major human resources providing palliative care consisting of voluntary activities | ||
| Holding virtual training courses and specialized training in undergraduate and postgraduate degrees | Non-governmental organizations such as the Hospis Malaysia and the National Cancer Society Malaysia are the main providers of palliative care | ||
| Training physicians for specialized palliative care in a 4-5-year course | |||
| Specialized pediatric palliative care | |||
| Health care financing | More than 220 charitable organizations and private institutions | The health care system includes government and private financing | Private hospitals and clinics provide services, as well as government centers. |
| Providing completely free palliative care services | Patients meeting the criteria set by the Ministry of Health receive care through federal funding. | Hospice centers are charitable and non-governmental organizations | |
| Palliative care provision through the efforts of the voluntary sector | All palliative care services at home or private centers are provided by non-governmental organizations. Costs are paid by the family, grants, and the tax paid by NGOs. | ||
| palliative care burden mostly on the Charity sector | |||
| 29 out of 99 public hospitals provide palliative care services based on the Ministry of Health guidelines through federal funding. | |||
| Service delivery | End-of-Life care through the framework of the NHS Operational planning in 2008-2009 | Providing 82% of outpatient care and 35% of emergency care by the public sector | Providing health services at 3 levels. |
| Providing palliative care services usually for people, whose estimated survival time is 2 years or less | Providing about 18% of outpatient care and 62% of emergency care by the private sector | Providing various types of palliative care services, such as outpatient care, home care, daycare, clinics, hospital support team, the Ministry of Education, patient support groups, family support group after patients’ death, parent support groups, orphan support groups, and hospice care for the homeless. | |
| Classification of palliative care services in 3 levels | Providing comprehensive services, including health promotion, disease prevention, pharmaceutical treatment, and health care through clinics and hospitals by the Ministry of Health and Medical Education | ||
| Providing physical care, spiritual care, socio-cultural care and psychological care, and support for the patient’s family and caregivers. | Several government ministries provide health services. | ||
| Full-time access to palliative care services, including telephone consultations or examinations by palliative care specialist nurses and doctors at patients’ home | The private sector providing health services is mainly located in urban areas. | ||
| Providing specialty and general persistent palliative care | Using traditional medicine services, such as Chinese and Malay specialists by a large population | ||
| Information and research | April 2013- Establishing the National End of Life Care Intelligence Network | June 1996 - Palliative care workshop at Queen Elizabeth Hospital | The 2nd Edition of the standards manual for healthcare in cooperation with the Council for Health Services Accreditation of Southern Africa |
| Background Electronic Palliative Care Coordination Systems within the palliative care system | 2016 - Publishing the report by Hospis Malaysia, under the title of Palliative Care Needs Assessment | 2000- Launching national and regional plans to improve care quality and accessibility | |
| Providing research projects in academic centers and publishing scientific journals | November 2015- Implementing the accreditation process using the electronic self-assessment tool | ||
| Holding congresses and scientific meetings | 2010- The evaluation of the mentorship program | ||
| Improving the research capacity in the field of palliative care | |||
| Assessing the quality of provided services according to different indicators |
After reviewing the content of palliative care in the selected countries, the data were extracted. First, the same data were removed and, then, the themes were identified and grouped according to the WHO framework. To ensure the validity and reliability of the data, 5 people were approved for their palliative care. Two authors (MA and SV) independently searched and selected the relevant documents. Policy document content was reviewed by 3 authors (SV, HR, and MA). Disagreement concerning the content of documents was resolved through discussion. Additionally, the key health indicators were investigated in the field related to the study as shown in Table 2. We used a strategy search according to Medical Subject Headings terms. In this study, the following keywords were used: (“cancer” OR “cancer patients:) AND (“palliative care” OR “supportive care”) AND (“policies” OR “programs” OR “strategies”) AND (“UK” OR “Malaysia” OR “South Africa”). The data were analyzed by content analysis approach, using MAXQDA software version 11. After reviewing the content of palliative care in the selected countries, the data were extracted. First, the same data were removed and, then, the themes were identified and grouped according to the WHO framework. To ensure the validity and reliability of the data, 5 experts were approved for their palliative care.
| Indicator | UK | Malaysia | South Africa | Source |
|---|---|---|---|---|
| Population, 2018 | 66,573,504 | 32,042,458 | 57,398,421 | WB |
| Urban population, % | 80.6 | 75.37 | 65.295 | WB |
| Population growth rate | 0.59 | 1.5 | 1.6 | WB |
| Population 0 to 15 years, % | 17.619 | 24.621 | 29.178 | WB |
| HDI, 2018 | Rank 14; 0,922 | Rank 57; 0,802 | Rank 113; 0,699 | UNDP |
| GDP | 2,650,850.18 | 296,535.93 | 295,456.19 | WB |
| GNI | 42370 | 9860 | 5480 | WB |
| Per capita expenditure on health | 4355.86 | 385.62 | 470.80 | WB |
| Life expectancy | 80.956 | 75.3 | 62.774 | WB |
| Cancer mortality | 166135 | 21500 | 41300 | WHO |
| The mortality rate for children under 5 years in 1000 births | 4.3 | 8.3 | 43.3 | WB |
| Maternal mortality in 1000 live births | 9 | 40 | 138 | WB |
| WHO region | Europe | Western Pacific | Africa | WHO |
| Income level classification of WB | High | Upper-middle income | Upper-middle income | WB |
| Health Expenditure, % GDP, 2015 | 9.88 | 4.00 | 8.20 | WHO |
3. Results
3.1. The Ranking of Countries in Palliative Care Services
In 2011, a report was issued by the International Observatory on End-of-Life Care and 234 countries were assessed and categorized into 4 groups regarding the development of palliative care services and based on indicators such as HDI, GDP, population size and raw mortality rate, the level of palliative care coverage, the type of the existing structure and the number of the levels of supportive and palliative care services, the level of the community’s awareness of palliative care, and the amount of informing the public. According to this categorization, the studied countries belong to the fourth group, which includes the two subgroups of a and b (35). Table 3 shows the categories of the selected countries based on the development of palliative care.
| Group | Countries |
|---|---|
| Group 4: Approaching integration | |
| 4a-Preliminary integration | Malaysia; South Africa |
| 4b-Advanced integration | UK |
The status of the selected countries mentioned in palliative care service of these countries is among the leading countries regarding the development of palliative care services; their support and palliative care systems possess some qualifications, such as palliative care integration approach, sufficient capacity to provide services in some parts of the country, the existence of a wide range of the types of palliative services and service providers, wide public awareness regarding care services, the existence of assessable integration and merging with health care systems’ services, the establishment of special training centers, large-scale academic communication, performance of applied studies, and the formation of national associations (35, 36).
3.2. Epidemiological Overview
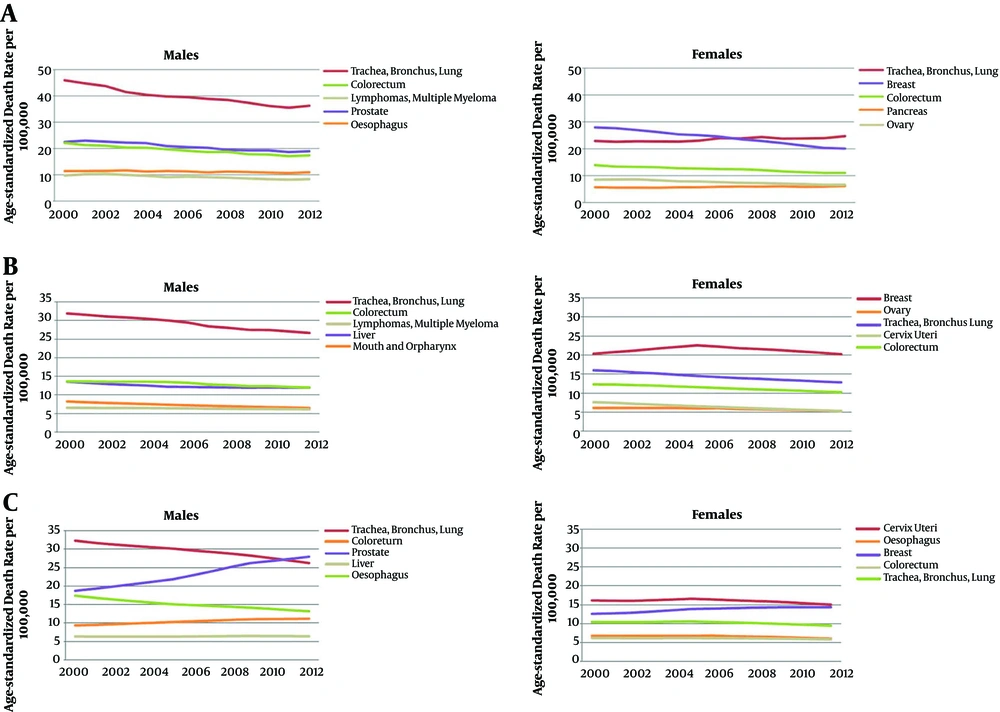
UK: The UK is a high-income country located in Europe (37). In 2016, 166 135 deaths caused by cancer were reported in this country. In 2014, 163 200 individuals died, 86 300 of whom were males and 76 900 of whom were females. Figure 2A shows the cancer mortality rate in both genders (38-40). In the UK, cancer accounted for more than 1 out of every 4 deaths (28%) in 2016. Nearly half of all cancer deaths have been reported to be associated with lung, bowel, breast, or prostate. In 2018, the UK had a cancer rate of 31902 cases per 100 000 people (41). More than 360 000 new cases of cancer are recorded annually in the UK. In 2015, the cancer rate was 183 000 new cases in men and 177000 in women per year. Every 2 minutes, 1 cancer diagnosis is recorded in this country. The incidence rate of all types of cancers in the UK will rise by 2% from 2014 to 2035, reaching a number of 742 new cases per 100 000 by 2035. Compared with the European Union, the cancer incidence rate in the UK is lower in men and higher in women. The most common type of cancer in the UK is breast cancer in females and prostate cancer in males (38-40).
Malaysia: Malaysia is a country with an above-average income located in the western pacific region (42). In 2014, 21 500 cancer deaths have been reported in this country, 11200 of which belonged to males and 10 300 of which belonged to females. Figure 2B shows the trend of age-related cancer mortality in men and women (39). In 2018, 43 837 new cancer cases and 26 395 cancer deaths were estimated in Malaysia (43). Contagious diseases are currently the leading cause of mortality and illness in this country (44). The most common type of cancer in Malaysia is breast cancer in females and lung cancer in males (39).
South Africa: South Africa is a country with above-average income located in the Africa region (45). In 2014, 41 300 cancer deaths have been reported in the country, 20 700 of which belonged to males and 20 600 of which belonged to females. Figure 2C shows age-related cancer mortality in men and women (40). The most common type of cancer is breast cancer in females and prostate cancer in men. The cancer mortality rate in these countries is about 5%, which is much lower compared with European countries (20%) (40). Cancer is not among the 10 leading causes of death in South Africa. According to the mortality rate data, the estimated need for palliative care in this country accounts for only 0.52% of the population’s need (46).
3.3. Stewardship/Policy Actions
In the UK, health management is done by the local authorities of each region, and the health system is responsible for developing protocols and palliative care guidelines (47). In Malaysia, public health services are also managed in an organized way, through central, provincial, and regional departments, under the administration of the Ministry of Health (48, 49). In South Africa, health centers are run by provincial health departments, and provincial offices are direct employers of health workers, while the Ministry of Health is responsible for policy development and coordination (11, 46).
3.4. Workforce
There are 6000 to 7000 palliative care professionals (around 5000 nurses, 750 physicians, and 70 000 social volunteers) employed in the UK. There are academic and higher education palliative care centers available in the country (50, 51). In 2016, there are 18 trained professionals in the field of palliative care working in Malaysia (52). From 2003 to 2004, 842 recruited employees had been working in the field of palliative care for around 125 780 hours per month in South Africa. On the other hand, the volunteer workforce consisted of 1978 people working a total of 25 806 hours per month within this period (46).
3.5. Health Care Financing
In the UK, 83% of hospital consultation costs, 59% of home care costs, 30% of hospitalization costs, and 23% of day clinics costs are paid by the government, and the rest is financed by a combined budget from both public and private sectors, and the government is responsible for the majority of financing (53). In Malaysia, only patients meeting the criteria set by the Ministry of Health receive care through federal funding. Mostly, this financial burden is placed on charity (54). In South Africa, along with service provision centers, there are private hospitals and clinics for those, who have health insurance coverage or can pay out of pocket for healthcare (46).
3.6. Service Delivery
In the UK, palliative care is integrated into the health system (55), while in South Africa, palliative care is provided in an isolated form in some areas. The coverage of palliative care is not centralized; in some areas, comprehensive care is provided at an appropriate level, while in other parts, even basic level care is not available (46, 56). In Malaysia, these services are provided only in some areas, but in a generalized and comprehensive form (22).
3.7. Information and Research
In 2001, the quality improvement Department for Cancer Services in the UK has regulated the standards of cancer service (57). In addition, the government commitments to the high quality of end-of-life care were developed in the Department of Health and Social Care (58). In 2016, Hopis Malaysia published a report titled Palliative Care Need Assessment (59). In 2005, South Africa formulated a standard manual for healthcare in cooperation with the Council for Health Services Accreditation of South Africa in order to evaluate the quality of services provided by the charity sector, whose third edition is currently in use (46).
Key health indicators in the field related to the study, as well as the policies and the plans for cancer supportive and palliative care in the selected countries based on the WHO guidelines in the fields of stewardship/policy actions, workforce, health care financing, service delivery, and information and research, are presented in Tables 1 and 2.
4. Discussion
This article compares the policies and the strategies for cancer supportive and palliative care in the UK, Malaysia, and South Africa. According to a report by the British Parliamentary and Health Service (2015), the causes of failure in palliative care provision in the UK were as follow: Weak symptom control, weak planning, communication, not addressing the needs of dying patients, insufficient out-of-hour services, ill-timed diagnoses, and treatment referrals (60).
National policies play an important role in spreading access to palliative care (22). One of the factors that distinguish the policies of different countries in supportive and palliative care provision is the existence and efficiency of a state strategy for national palliative care (55). In the UK, there is a comprehensive strategy for the enhancement and development of national palliative care. The vision and targets are clarified, and an action plan is defined along with powerful mechanisms in order to achieve these targets. Besides, the strategies are clearly determined by the central government and are regularly assessed and updated, and local governments should follow them. In fact, the policy implementation process has is up-down (36, 50). However, in Malaysia and South Africa, despite the fact that there is a governmental strategy and a broad vision of the development and promotion of national palliative care, the general and the specific goals are not defined and there are limited mechanisms to achieve goals (46, 56). In these countries, unlike the UK, the local states are not obliged to follow national strategies. In other words, these strategies are only prescriptive in nature (36, 61). In these countries, the Ministry of Health is responsible for the stewardship and the policy actions of palliative care, and regional departments are responsible for implementing these policies (50, 62). One of the advantages of South Africa is its major role in global issues and a palliative care statement during the African Union Summit in 2013 issued by the Minister of Health (36). In 2016, a palliative care policy framework was also approved. The UK owns the highest quality of death as a result of inclusive national policies, the broad integration of palliative care into national healthcare services, and the powerful hospice movement. It also has the highest score for care quality. Generally, income level is a good indicator of palliative care accessibility and quality: rich countries such as the UK are placed high in the ranking of palliative care (55).
One of the success factors in achieving palliative care goals is the deployment of professional and specialized personnel (36). There are adequate professional palliative care experts in the UK, which are approved by national professional boards. Volunteers must also attend a training course. The UK is the first country, in which palliative care has emerged (51). It also has the best children palliative care services (63). As in the UK, there is professional palliative care staff in Malaysia and South Africa. However, there is a shortage of doctors, nurses, and other support staff (49, 64). Unlike the UK, in this country, specialized palliative care education does not generally need to be approved by national professional boards (36). Although South Africa is not among the top countries in the human resources ranking (ranked 59th), it is, in many cases, a leading force in training and educating the workforce. The first MSc degree in the field of palliative care was presented at the University of Cape Town, South Africa (65). Another advantage of the palliative care plan in this country is the education of family physicians with the aim of integrating palliative care into the healthcare system. Among the successful programs in the UK, which other countries can adopt, lunching the National End-of-Life Care Intelligence Network in April 2013 and developing Background Electronic Palliative Care Coordination Systems within the palliative care system can be mentioned (66).
In order to increase access to palliative care, government funding is essential. In some countries, despite the fact that government funding is allocated to this type of care, either it is difficult to access it or it is poorly monitored (22, 36). In many countries, including the UK, providing palliative care is possible through charity (55). In the UK, government subsidies or public programs exist for individuals to increase the accessibility to palliative care. There are clear qualification criteria and simple procedures for using funds. There are instructions for accessing these funds. The effectiveness of this plan is examined on a regular basis (36). In Malaysia and South Africa, as in the UK, there are government subsidies or appropriate plans for people, who have access to palliative care (36, 48). Qualification criteria are also clear, but unlike the UK, access to budgets and programs is difficult and the effectiveness of programs is not monitored. Subsidies are needed for palliative care services in order to make the treatments more affordable. These aids are provided in the form of national insurances, pension programs, and charity funds, the same as in the UK (55).
A large number of patients die every year in hospitals globally, but many of them spend their final days at home or in hospices (22). England is one of the countries that is making changes in order to increase the quality of care received by patients and help reduce the costs of the National Health Service in the country (67). While countries need to take efforts for increasing palliative care accessibility and make the services affordable, the quality of care should also be taken into account. It should be ensured that painkillers, such as opioids, are easily available and managed properly (22, 36). Opioid painkillers are freely available in the UK. However, in South Africa and Malaysia, these drugs are always available or can be accessed only through specific laws, bureaucratic procedures, and prejudices (36, 62). South Africa has better access to medications than many African countries do (65). One of the South African national policies for palliative care (2017 - 2022) is the correct and stable access to appropriate medicines and related supplies to provide palliative care (68).
When the end-of-life comes, community engagement becomes important. When communities, volunteers, and families accept more responsibility, emergency admissions and hospital costs will be decreased. For policymakers, the question is how to increase motivations and develop support systems for further encouraging the community. In today’s world, people find it hard to discuss topics around death. So, it is of importance that social groups increase public awareness of palliative care. Another advantage of palliative care in the UK is that it has the second place in terms of public awareness on this field, of which people have a strong perception. Information on palliative care can easily be found through public portals and communities (69). But, in Malaysia and South Africa, people have an average perception and knowledge about palliative care. Besides, the information available in this regard on public portals and communities is not broad (36, 48, 49). The palliative care resolution issued by the World Health Assembly has created a strong motive for all countries to formulate palliative care policies, and in most countries, there is a big deal of effort made to ensure that all citizens access palliative care. However, in many developing countries there is still little or even no access to palliative care (19).
In Iran, due to the high rates of cancer-related mortality and the high cost of treating this disease (70), the health system requires to design of a purposeful program that will prioritize providing palliative care services to patients with cancer. By examining and analyzing palliative care policies in countries like the UK, Malaysia, and South Africa, all of which are pioneers in developing palliative care services and selected from 3 different continents, lessons can be learned from the challenges, weak points, and strengths of their policies and plans. They can be used as models for countries like Iran, which is at the beginning of its path. Although different models and policies have been presented for the provision of palliative care services in patients with cancer, in integration with the health system in different countries, selecting and implementing them requires attention and considering the specific conditions of each society and, consequently, the policies of the health system in that country and, ultimately, informed decision-making by health-care policymakers.
The present study had limitations, some of which can be mentioned here. It was not possible to access to all the data of the target countries. Some programs may be inaccessible or confidential; nevertheless, the authors of this study tried to review all the documents. The diversity of health structures and documents in the selected countries has led to lots of differences in the implementation of various programs, posing challenges in decision making around choosing the best policies.
4.1. Conclusions
Countries should consider palliative care as one of the top priorities of the health system and a method for improving QOL in patients with cancer and their relatives due to the high prevalence of chronic and incurable diseases such as cancer, the increased aging population, limited intensive care beds, the shortage of equipment, financial and human resources in medical centers, and the importance of palliative care as a missing link in the cycle of healthcare. Although most countries in the world still have a long way to reach the desired level in providing support and palliative care, they can accomplish this goal by taking into account the conditions of each country, focusing on each area of practical guideline, examining the situation and the facilities available, and learning from the experiences of other countries.