1. Introduction
Rhabdoid Tumor is one of the rare and aggressive malignant tumors of childhood that was introduced as a subgroup of the rhabdomyosarcomatoid of the Wilm’s tumor in 1978 at first because it is similar to rhabdomyoblast in viewpoint of pathological features (1-3).
Malignant Rhabdoid tumor incidence is very low but the outbreaks of the cases out of kidney and especially of the organ involvement is relatively rare (4, 5).
The age of the incidences during infancy (from 20 days up to 50 years old has been reported), but it is more common around the age of 20 months. Generally, boys are involved 1.5 times more than girls are and in most cases, the patients would die within 6 months after the diagnosis (6).
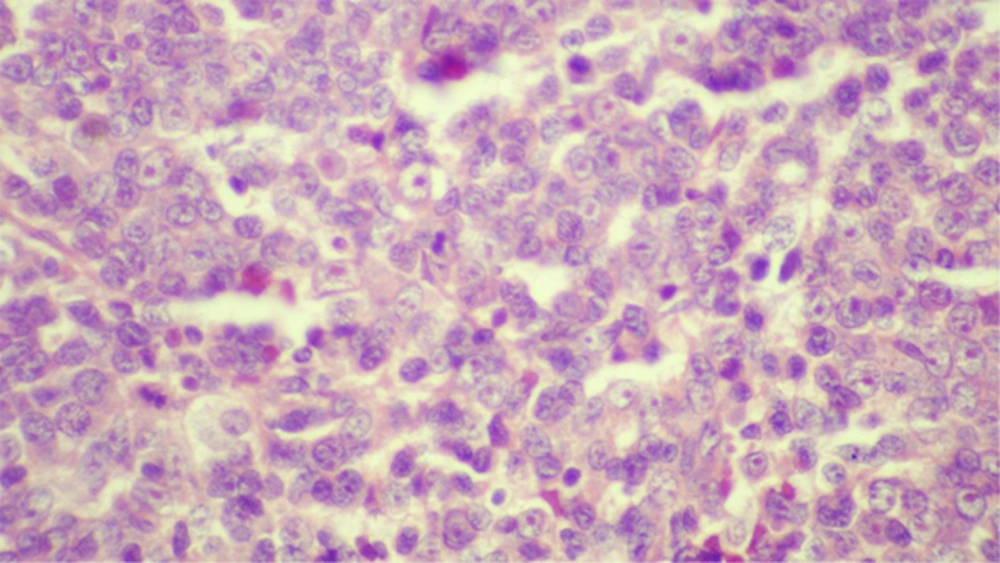
The most common site of tumor outside the kidney is cranium (7). In microscopic study, round cell or polygonal proliferation is seen with the eccentric core, prominent and clear nucleoli, eosinophilic cytoplasm by having hyaline-like inclusion bodies. This characteristic histopathologic finding is found in some of the soft tissue sarcomas or synovial sarcoma, and the extraskeletal myxoid chondrosacroma shows similar findings (8).
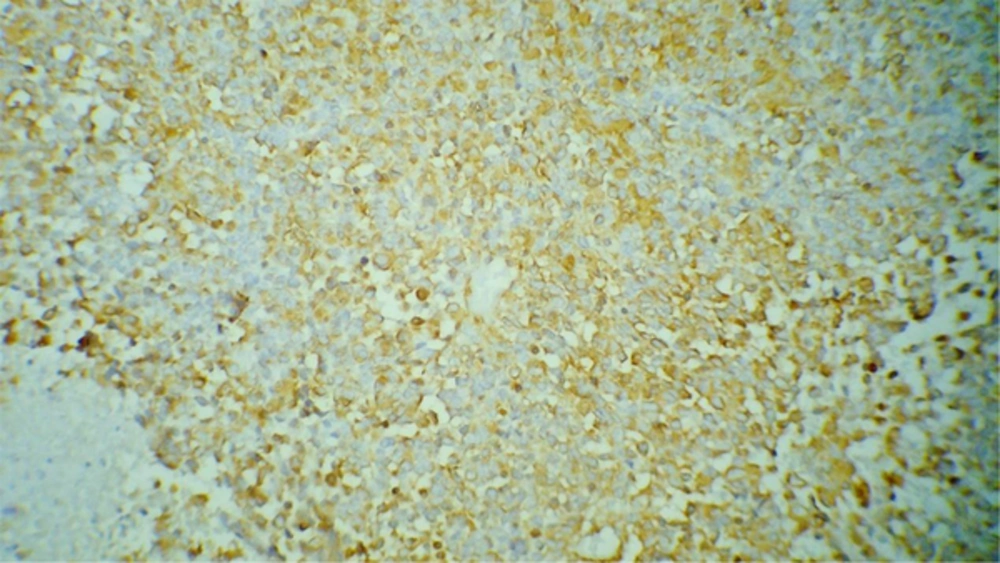
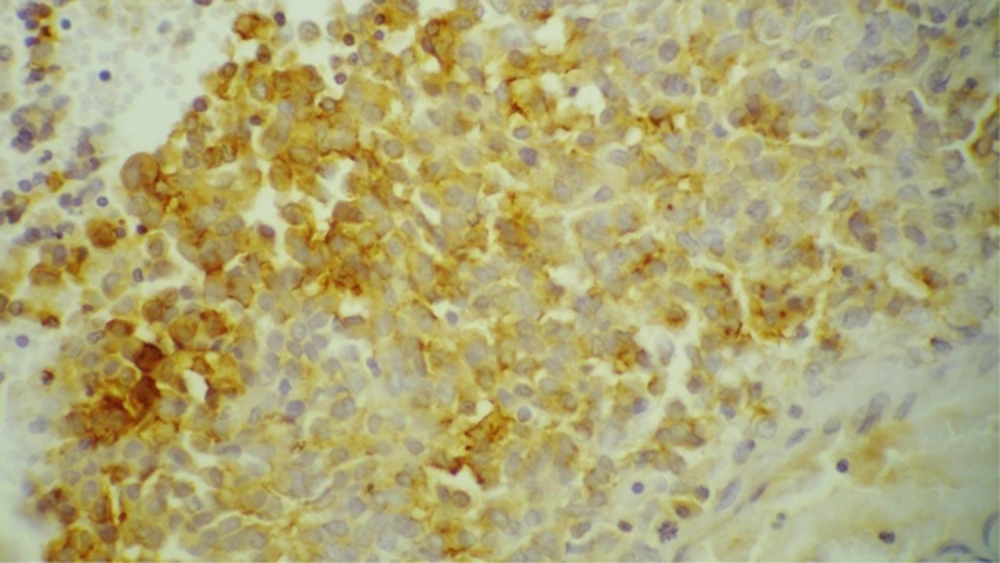
In immunohistochemical studies, neural markers such as synaptophysin, CD57, neuron specific enolase (NSE), smooth muscleactin, S-100 protein, vimentin, EMA, cytokeratin, CD99 and desmin might be seen, and desmin is expressed sporadically (9, 10).
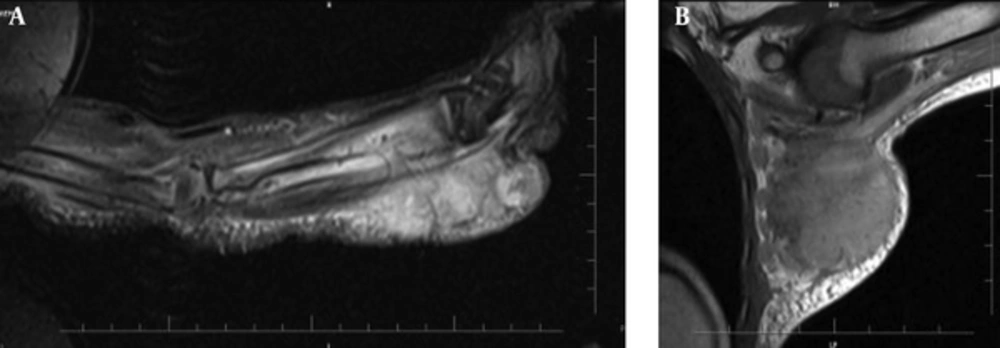
Radiological characteristic or specific findings were not recognized for this group of rare infantile tumors but tumoral lesions have heterogeneous hyperintensityin CT scan/T2-MRI studies.
The prognosis of malignant rhabdoid tumors is unfavorable and most of children would die within six months after diagnosis. The invasiveness, young age of the patients, limitations of the use of radiation in this young age and the tolerance of the chemotheraputic agents in infancy have important roles in the prognosis of these patients.
2. Case Presentation
A 15-month-old girl referred due to swelling of the anterior part of the left forearm and left axilla that started one month earlier. In the examination, there was a large mass about 5cm × 14cm that involved more than distal-half of the left forearm. It was warm, relatively stiff and painless causing decreased left hand’s movements. Another soft tissue mass with a diameter of about 8 - 10cm was in the left anterior axillary space with well-defined, stiff limits, and its skin was warm and erythematous. Other physical examinations were normal. The liver span was normal and spleen was touched maximum 1cm below the left rib edge. CBC was normal and ESR = 20. In color doppler sonography of left upper limb, one solid heteroechogenic mass was seen around the distal left forearm bones and also several hyperechoic ovoid masses were found (with maximum diameter of 20mm × 14mm). In ultrasound of the abdomen and pelvis, splenomegaly was reported. Aspiration and biopsy of bone marrow showed normal results. In bone survey, periosteal reaction and distal cortical thinning of left ulnar (suggestive of tumor invasion into the bone) was obtained. There is no abnormal finding in the brain, thoracic, abdomen and pelvis CT scan, and in the whole body bone-scan. MRI of left upper limb and finally microscopic and immunohistochemical study on tissue biopsy sample of anterior mass of left forearm confirmed the diagnosis. Left forearm mass biopsy revealed tumoral sheet composed of medium sized cells with vesicular chromatin and occasionally prominent nucleoli, scant to medium amount of eosinophilic cytoplasm mostly with epitheloid features. Some areas show discohesive cells with rhabdoid features and multifocal necrosis, hemorrhage and scattered macrophages. IHC study detected CD34 (focal positive), S100 (focal positive), EMA (focal positive), Vimentin (diffuse strongly positive), Ki67 (~20%), but negative results for CD99, CD45, CD30, Myogenin, Desmin, Pan CK, Synaptophysin and Chromogranin.
3. Discussion
Malignant Rhabdoid Tumor (particularly its extrarenal subgroup) includes a group of very rare and progressive tumors that are often resistant to treatment. The outbreaks in extrarenal areas and especially in the limb is 0.1 out of one million.
Our patient had a mass with certain limits on the left anterior forearm and also the left anterior axilla where there was no metastasis to distant organs during assessment. The brain and kidneys had no tumor extention. The age range of this group of the malignant tumors is between three months up to 50 years (2). Our introduced patient showed her first symptoms at the age of 14 months (three weeks before referring and diagnosis of the disease). So the chemotherapy started after initial radiography, and tissue sampling considering the clinical features. Although in some studies, the radiation together with surgery and chemotherapy may be useful in controlling and treatment of MRT but because of the young age of the patient, radiotherapy may have longtime undesirable effects on her growth, thus we did not put it in our patient’s treatment method and we hoped we could provide long time survival for the patient by helping adjuvant chemotherapy and surgery. To our knowledge, this case is the first case of extracranial extrarenal rhabdoid tumor of extremities in our hospital.
3.1. Conclusion
Due to low incidence and prevalence of MRT especially extrarenal subtype, more clinical trials should be done to disclose the optimal treatment according to individual conditions of the patients to increase the overall survival.