1. Introduction
Infective endocarditis (IE) is a life-threatening infection of the heart valve endothelium with symptoms such as fever, fatigue, night sweats, aching joints, anemia, and weight loss (1, 2).
Prosthetic valve endocarditis (PVE) is a serious infectious disease. The most common bacteria are streptococci and staphylococci. Diagnosis is based on symptoms and a new or changed heart murmur supported by blood cultures and heart ultrasound (echocardiography) (1-3). The risk of death among those infected is about 25% (4). Without treatment, it is almost universally fatal (3, 5)
Here, we reported a case of prosthetic aortic valve presented to the hospital with fatigue, anemia, and illness.
2. Case Presentation
A 68-year-old male patient with a history of chronic kidney disease presented to our emergency department with severe anemia, illness, and about 10 kg weight loss. The patient underwent metallic aortic valve surgery two years ago due to severe aortic stenosis.
The patient was ill, pale, and afebrile with no icterus. His vital signs were stable. On examination, the patient did not have any lymphadenopathy. Cardiac examination revealed a metallic sound with diastolic murmur III/VI in LSB. Blood tests showed raised creatinine level (6 mg/dL), sedimentation rate (86 mm/h), and CRP (29 mg/L). His blood cell count and Autoimmune screen tests were as follows: WBC = 7900 cells/ microliter, Neutrophils = 70%, Hb = 6.1 mg/dL, Platelet count = 176000, RETIC count: 4.3%, Negative ANA, direct and indirect Coombs test and normal C3, C4, CH50.
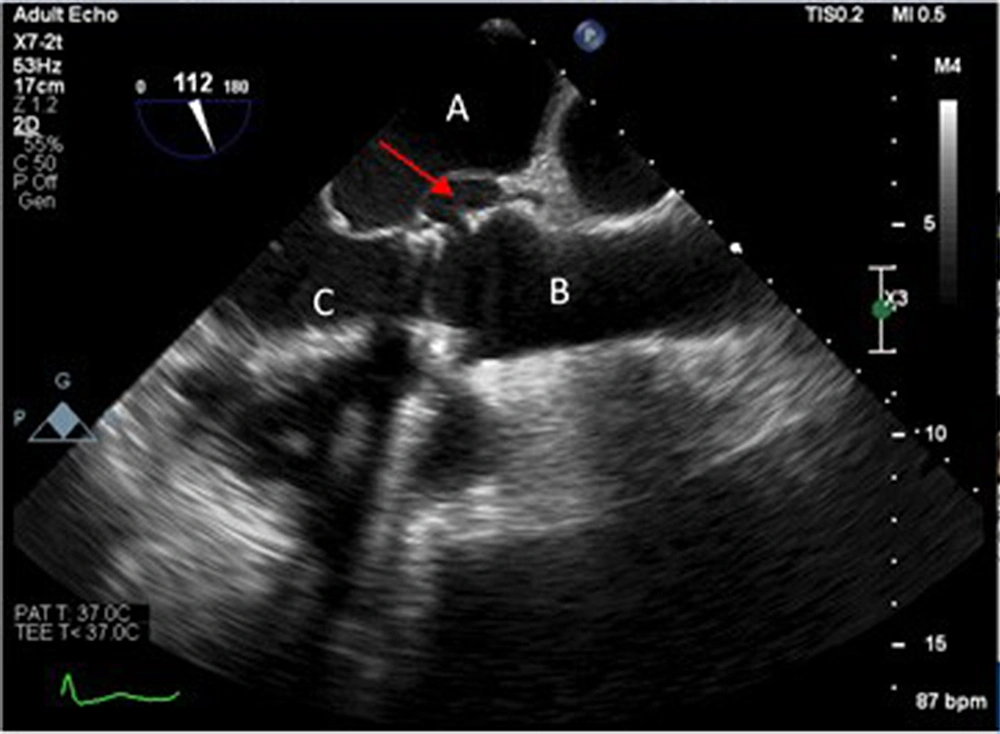
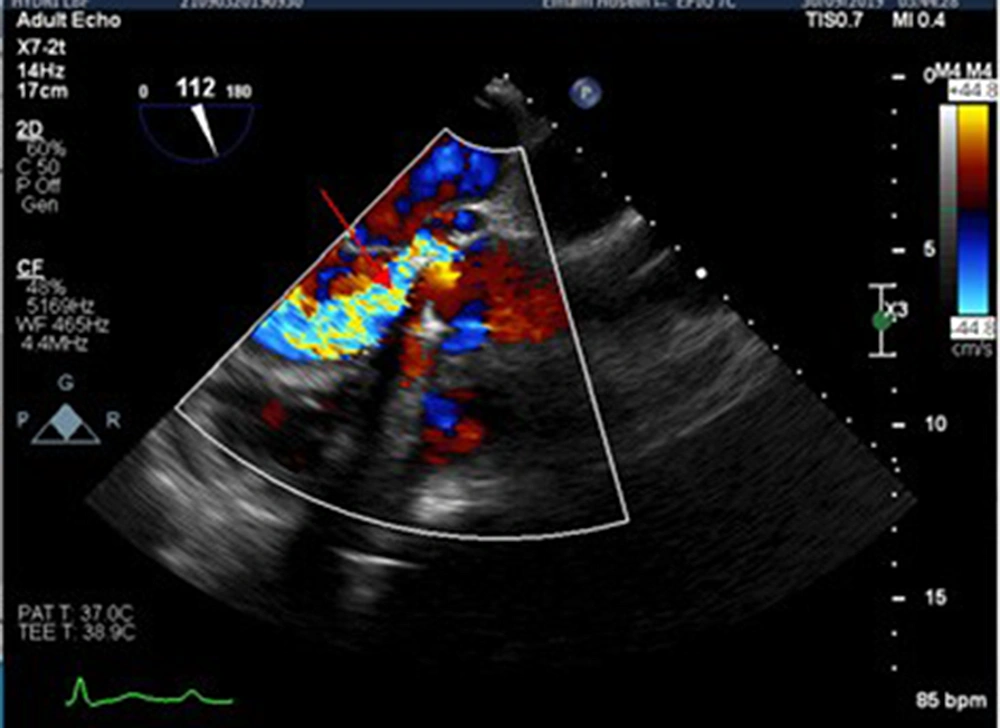
On the third day of hospitalization, he developed a fever. The antibiotic was started in the form of empirical meropenem. Transthoracic echocardiography revealed significant valvular leakage from the prosthetic valve. Due to strong clinical suspicion of infective endocarditis, the patient was scheduled for transesophageal echocardiography that revealed significant transvalvular and paravalvular leakage with pseudoaneurysm of mitral-aortic intervalvular fibrosa that made a fistula to left ventricular outflow tract and sinus Valsalva of aorta (Figures 1 and 2). prosthetic aortic valve showed partially dehiscence. All the above findings were highly suggestive of complicated infective endocarditis.
Two days later, according to the blood culture result (vancomycin-resistant enterococci with sensitivity to ampicillin and imipenem), the patient's antibiotic was changed to ampicillin, imipenem, and rifampin.
Because of the patient's clinical conditions' gradual deterioration (symptoms of decompensation heart failure), he was scheduled for open heart surgery. The patient underwent a new prosthetic aortic valve surgery to repair an intervalvular fibrosa pseudoaneurysm. Unfortunately, after the operation, he died because of septic shock and severe acidosis.
3. Discussion
Prosthetic valve endocarditis is a serious complication in cardiac surgery patients, constituting 20% of endocarditis cases (6). Despite advances in surgery and rapid diagnosis and treatment of endocarditis, PVE still has a high mortality rate. The indications for surgery in PVE are valve dysfunction, decompensated cardiac failure, heart block, recurrent embolism, uncontrolled infection, and special organisms (fungus, gram-negative bacteria). One of the catastrophic complications is abscess formation which is the spread of infection to adjacent tissues. Mitral aortic intervalvular fibrosa (MAIVF) is one of the most common sites of abscess. Mitral aortic intervalvular fibrosa is a thin and avascular fibrous tissue between the mitral and aortic valves prone to abscess formation, spontaneous rupture, and drainage of infectious contents into the left ventricle (Pseudoaneurysm) (6).
Even if PVE is diagnosed and treated quickly with surgery, the morbidity and mortality rate is high (4).
A rare presentation of endocarditis is anemia, that reported in some cases. The cause of anemia has been hemolytic anemia, mechanical and autoimmune hemolysis, with normochromic and normocytic cells (7-9).
Complications of infectious endocarditis include involvement of various organs; one of the most important of them is kidney involvement which can include renal cortical necrosis, acute interstitial nephritis, focal and diffuse proliferative glomerulonephritis and interstitial nephritis related to antibiotics (10-13).
This case report indicates that anemia and fever of unknown origin in patients with renal failure can be one of the diagnostic signs of endocarditis. It is important to consider infectious endocarditis in high-risk patients because late diagnosis greatly increases mortality, serious complications, and morbidity.