1. Background
The globalization of food markets and urbanization are leading to massive changes in diets worldwide, including the Middle East (1-3), which is a major contributor to the global burden of obesity and type 2 diabetes (T2D) (4, 5). Iran is no exception, with a sharp increase in the incidence of both diabetes and obesity having been observed over the past decade (5, 6).
The glycemic index (GI) is one of the indicators of carbohydrate-containing foods, which categorizes carbohydrates according to their postprandial glycemic response relative to a reference carbohydrate source, usually glucose or white bread (7, 8). The scale ranges from 1 - 100 (8). Evidence from meta-analyses of observational studies clearly shows a correlation between the consumption of high-GI foods and T2D (9, 10), cancer (11, 12), and cardiovascular diseases (13, 14).
Refined grains such as bread and white rice are the major sources of total calories in the Iranian diet, comprising 55% - 60% of consumed calories (15, 16), which generally have a high GI (8, 17). The International Table of Glycemic Index provides a comprehensive reference for GI values (8, 17). According to the table, white wheat-based bread and white rice GI values can vary widely depending on variety, the amylose content of rice, cooking, processing, physical size, and the forms and texture of bread (8, 17). Therefore, locally estimated GI values of traditional staple food in Iran are urgently needed for a better understanding of their relationship with cardiometabolic health outcomes in future research projects. However, specific GI values for Iranian rice and bread are not included in this table (8, 17). In addition, in 1997, the GI of traditional types of bread and rice measured in people with T2D were incompatible with the standard method for GI Determination (18, 19).
2. Objectives
Furthermore, varieties of brown rice have recently become partially available in Iran, but no data on GI values are available. This study can help gather reliable data for the comprehensive International Table of GI Values, which can be used for ongoing research regarding GI, as well as in clinical practice. Hence, the study objective was to measure the GI values of several types of flatbread, including Barbari, Taftoon, Sangak, Lavash, white rice, brown rice, and a mixture of lentil white and lentil brown rice known as Adaspolo, industrial barley, and rye bread (Sahar Bread. Co).
3. Methods
3.1. Subjects
Sixteen healthy, non-smoking volunteers (4 men and 12 women) were recruited from staff and students from November 21st, 2016 to March 12th, 2017, at Tehran University of Medical Sciences in Tehran, Iran. The baseline characteristics of the participants were obtained. The inclusion criteria were healthy adults aged 18 - 45 with Body Mass Index (BMI) between ≥ 18.5 and ≤ 30 kg/m2. The exclusion criteria were fasting blood glucose (FBG) ≥ 5.5 mmol/L; those with chronic diseases (cardiovascular diseases, diabetes type 1 and 2, hypertension, metabolic syndrome, cancer, renal disorders, digestive tract diseases, celiac); those following a special diet such as the Atkins diet; and taking any medication concerning glucose metabolism (metformin, etc.), thyroid function, pre/probiotic, any supplements. Athletes, as well as pregnant or breast-feeding women, were also excluded from the study.
After a comprehensive explanation of the study procedures, written informed consent was obtained from all participants. The study was conducted according to guidelines laid down in the Declaration of Helsinki, and all procedures were approved by the Ethics Committee of Tehran University of Medical Sciences (IR.TUMS.EMRI.REC.1394.023). This study was registered at www.irct.ir, identifier: IRCT2016011125947N1.
3.2. Study Design
This study was designed based on the standard method for determining GI, published by International Standard-ISO 26642 (19).
The participants were asked to attend the School of Nutrition Sciences and Dietetics at 7:30 AM for 13 days; 10 days for food tests, and 3 days for reference foods with a 2-day washout period (19). Prior to being tested, the participants were instructed to fast for 12 hours the day before and avoid any vigorous activities, smoking, alcohol consumption, high-fiber foods, indigestible high-carbohydrates (e.g., unripe fruits), and high-fat/high carbohydrates (20). Continuation with daily routines such as physical activity and dietary routine was encouraged.
Anthropometric measurements were made prior to the test day. The body weight was measured using a Seca digital scale (nearest 0.1 kg) with subjects wearing light clothing, and height was measured using a metric standard (nearest 0.1 cm) with subjects being barefoot. In addition, their BMI was calculated using the standard formula: weight (kg)/height (m)2.
Anhydrous glucose (Merck Co.) (50 g glucose dissolved in 250 mL water at room temperature) was used as a reference carbohydrate. Based on the fact that response fluctuations to reference foods typically impact resulting GI values, the glucose solution was given three times, once on the first, middle, and last days, respectively. Other test foods were measured once.
The order of food items tested was the same for all participants. On the first day, they were instructed to consume the prepared reference carbohydrate solution (the glucose solution) over a 12 - 15-minute period. On the following test days, other test foods (portions based on 50-gram available carbohydrate, calculated as the sum of starch and sugars) were evaluated, to be consumed over a 12 - 15-minute period, served with 250 mL room-temperature water. The compositional information of the test food has been adapted from the Iranian Food Compositions Table is provided in Table 1 (21).
| Food (100 g) | Water (%) | Kcal | Fat (g) | Protein (g) | Total CHO (g) | Dietary Fiber (g) | Total Sugar (g) | Starch (g) | Available Carbohydrate (g)* | portion Size (g) |
|---|---|---|---|---|---|---|---|---|---|---|
| Sangak bread | 33 | 258 | 0.7 | 7.7 | 57.4 | 4.1 | 1.5 | 51.9 | 53.3 | 94 |
| Lavash bread | 24 | 291 | 0.8 | 8.8 | 63.4 | 2.4 | 0.8 | 60.2 | 61 | 82 |
| Taftoon bread | 28 | 279 | 0.7 | 8.1 | 61.1 | 2.2 | 0.8 | 58.1 | 58.9 | 85 |
| Barbari bread | 29 | 272 | 0.6 | 8.4 | 59.5 | 2.2 | 0.8 | 56.5 | 57.3 | 87.5 |
| Barley bread | 34 | 254 | 2.3 | 7.3 | 54.8 | 7.7 | 6.3 | 40.9 | 47.2 | 106 |
| Rye bread | 40 | 242 | 1.9 | 7.4 | 48.1 | - | 3.2 | - | 43.2 | 116 |
| Lentils | 11 | 290 | 19.6 | 1 | 66 | 30.3 | 1.5 | 34 | 35.7 | 27a - 30b |
| Uncooked brown rice | 12 | 363 | 2.7 | 7.9 | 76.1 | - | 0.5 | - | 72.7 | 69c - 54d |
| Uncooked white rice | 8 | 368 | 1.1 | 9 | 81.3 | 1.4 | - | 79.9 | 79.9 | 62c - 51d |
Composition of Selected Sources of Carbohydrate Per 100 Gram Serving
For the blood glucose response test, capillary blood samples were taken by lancet from the middle and ring fingers (19, 22). Initially, the participants were asked to wash their hands, then two finger-prick blood samples were taken at -5 and 0 minutes while fasted. Postprandial blood glucose was measured 15 minutes after the first bite and at 30, 45, 60, 90, and 120 minutes. Blood glucose was measured in the whole blood using a reliable standard glucometer (ACCU-CHEK Performa-Roche Diagnostics GmbH, Germany) (23). The glucometer was calibrated using the manufacturer’s control solutions 15 minutes before the start of the test. The inter-assay CV on the standard solution was less than 3, and the laboratory’s CV for 24 duplication measurements of fasting glucose was less than 3.03%. Both meet usual standards, whereby CV should be lower than 3.6% and 5%, respectively (19).
3.3. Test Foods
The foods tested were Lavash and Taftoon (100% wheat flour (WF), 86% - 87% extraction rate (ER)), Barbari (100% WF, 82% ER), and Sangak (100% WF, 88% ER) which are wheat flatbread (24), barley “100% simple barley bread, Sahar Bread Co.”, rye “toast rye bread, Sahar Bread Co.”, as well as brown rice, white rice, and a mixture of white rice with lentils known as “Adaspolo” with a ratio of 2:1, respectively (Adaspolo A), and a mixture of brown rice with lentils with the same ratio (Adaspolo B).
White and brown rice were obtained from the same strain of rice, “Tarom, Golestan.co,” which constitutes 24% of overall Iranian rice consumption. Preparation of both types of rice was standard, including rinsing and soaking in salted water for 30 minutes, followed by boiling for 15 minutes without oil, then steaming for 20 minutes (water-rice 2:1). The soaking and cooking time required for the brown rice was 2 hours and 45 minutes, respectively. For the Adaspolo, lentils were rinsed and soaked for 4 hours, then boiled in salted water for 45 minutes until tender. The rice and lentils were then steamed together for about 40 minutes without oil. The information on distribution and supply of flours at various bakeries in Tehran were collected from both the Grain Organization and the Grain Research Institute. Owing to the vast expanse of the city (Tehran), we divided the city into five areas (north, south, east, west, and center). In these areas, a complete list of existing bakeries was obtained from the Tehran Bakers’ Union. Then, the bakeries were randomly selected from different areas of the municipality. The sampling method was performed by the statistician’s research team. For each type of bread (Lavash, Barbari, Taftoon, Sangak), three bakeries from each area were selected based on the randomization table using a random number table (Microsoft Excel 2010). As a result, each type of bread was purchased from 15 different bakeries. The industrial types of bread, including barley and rye were purchased from the Sahar CO. store. The types of bread were immediately packaged in polyethylene bags and frozen (-18°C) to preserve freshness, then defrosted at room temperature 3 hours before testing.
3.4. Calculation of Glycemic Index
Blood glucose response was expressed as the incremental area under the blood glucose response curve, and was calculated using the trapezoidal method and the IAUC method, based on a mathematical formula (disregarding the area below baseline). The IAUC for each test food ingested by each subject was expressed as the percentage of the mean IAUC glucose for three repetitions of the reference food (glucose) consumed by the same subject as GI = (IAUC test food/mean IAUC glucose) × 100. The mean values for all subjects were considered the GI of a given food. The GI values were categorized into low, medium, or high glycemic response. The cut-off for GI values was: < 55, 56 - 69, ≥ 70, respectively (8).
The glycemic load (GL) of each test food was calculated using (GI of test food × available carbohydrate in a serving of test food (g))/100, available carbohydrate was calculated as the sum of starch and sugars (21).
3.5. Statistical Analysis
International Standard-ISO 26642 asserts a minimum of ten participants is enough to determine the GI value (19); accordingly, 16 participants were considered (19, 22, 25-28). Then IAUC and GI values were calculated using Microsoft Excel® 2010, the results were expressed as means with standard error of the mean (SEM). The GI values were calculated twice, once without excluding outliers, once excluding outliers defined as individual GI values for a given food that were greater than 2 SD above the mean. The levels of intra-individual variations of the standard (glucose) tests were assessed by determining the coefficient of variation (CV) [CV% = 100 × (SD/mean)] of the IAUC of each subject’s repeated glucose load (termed ref CV), where the reference CV should be lower than 30% to be considered accurate (19). All statistical analyses were performed using STATA V.11 (STATA Corporation, College Station, TX, USA). Charts were drawn by R-program 3.1.2.
4. Results
During the study, four out of 16 participants dropped out due to schedule and work-related conflicts; procedures and measurements continued with 12 participants, which did not significantly affect the statistical potential required for data analysis (19, 22). The study included 4 men and 8 women, with a mean age of 29.1 ± 5.3, height (m) 1.66 ± 0.1, weight (kg) 67.03 ± 8.2, BMI (kg/m2) 24.4 ± 3.3, and FBS (mmol/L) 4.8 ± 0.3.
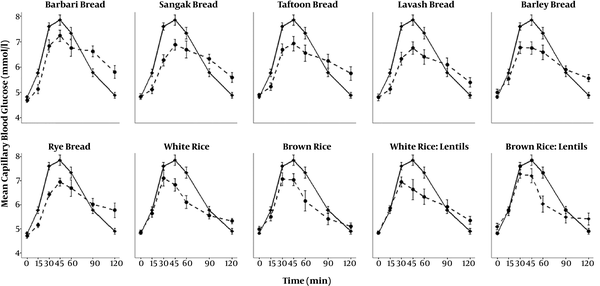
The mean GI and GL values of all the test foods are given in Table 2 and Figure 1. The GI values are presented as means with standard errors. The GI values are categorized into low, medium, or high glycemic response. The cut-off values are as follows: 55, 56 - 69, and 70, respectively (8). The mixture of brown rice with lentils with a value of 55, was placed in the low-GI category; barley bread and brown rice had GI values of 66 and 65, respectively, and therefore, were categorized as moderate-GI. Barbari bread had the highest glycemic value among the test foods. The GI value of Barbari bread was 99, which therefore categorized it as high GI. Other bread types also had high GI values: rye bread 84, Sangak 82, Taftoon 79, and Lavash 72. There was one outlier in the rye bread and barley bread groups, which were recalculated after excluding outliers. The GI values (mean (SE)) without excluding outliers were 90 (9) and 72 (8), respectively.
| Food | N | GIa, Mean ± SE | GI Classification | Serving Size (g) | Available Carbohydrateb (g/serving) | GL (per serving) |
|---|---|---|---|---|---|---|
| Bread | ||||||
| Lavash | 12 | 72 ± 7 | High GI | 30 | 18 | 13 |
| Taftoon | 12 | 79 ± 9 | High GI | 30 | 17.67 | 14 |
| Barbari | 12 | 99 ± 8 | High GI | 30 | 17.19 | 17 |
| Sangakc | 12 | 82 ± 6 | High GI | 30 | 16 | 13 |
| Rye | 11d | 84 ± 7 | High GI | 30 | 13 | 11 |
| Barley | 11d | 66 ± 6 | Moderate GI | 30 | 14.16 | 9 |
| Rice | ||||||
| White rice (Tarom) | 11e | 71 ± 10 | High GI | 30 | 24 | 17 |
| Brown rice (Tarom) | 12 | 65 ± 6 | Moderate GI | 30 | 22 | 14 |
| Lentils:White rice, 1:2 | 11e | 79 ± 7 | High GI | 30 | 19.5 | 15.4 |
| Lentils:Brown rice,1:2 | 11d | 55 ± 4 | Low GI | 30 | 18 | 10 |
Glycemic Index (GI), Glycemic Load (GL) Values, and Classification for Major Sources of Carbohydrate in the Iranian Diet
Mean blood capillary glucose concentrations, (–––) for pure glucose solution and (- - - -) for test foods. Barbari (refined wheat bread), Sangak (wheat bread), Taftoon (refined wheat bread), Lavash (refined wheat bread), barley and rye bread, white rice, brown rice, a mixture of lentils with white rice, and a mixture of lentils with brown rice.
The mean intra-individual CV of glycemic responses to the three standard tests for the 12 participants was 27%, which met the standard that the reference CV should be lower than 30% for accuracy (19, 20).
5. Discussion
The current study reported the GI values of refined carbohydrate staple foods in Iran, which are the main energy sources in Iranian diets (16). It was also the first to determine the GI of a traditional mixture of lentils with both white and brown rice. The results demonstrated that different types of traditional flatbreads tested in this study, as well as white rice, and a mixture of white rice and lentils (Adaspolo A) are classified as having a high GI. In contrast, brown rice and barley bread had moderate GIs, while brown rice and lentils (Adaspolo B) had a relatively low GI.
These results regarding the types of bread (except for rye bread) are consistent with the International Table of the Glycemic Index, which reports the GI value of whole-meal barley flour (80%) bread (20% white-wheat flour) (Sweden) as 67, and white-wheat-flour bread ranging from 69 to 87. These include the GI of white-wheat-flour flatbread (Sweden) at 79, Turkish bread (white-wheat flour) at 87, and Middle Eastern flatbreads (Lebanese) at 97 (8). The GI value of rye bread (84) is similar to a study that reported the GI of short rye bread as 82 (29), both higher than rye bread in the International Table of the GI (ranging from 41 - 66). Different rye used in the bread might produce this difference (rye-kernel versus milled rye). The milling of the grain and the size of fiber in the bread could explain the lower GI (30, 31). It has been shown that adding rye kernel reduces the GI of bread in comparison with adding whole-meal flour (32). Another reason for the rye bread being high GI may be due to using malt, which results in breaking the interaction between proteins and starches, creating a porous structure and leading to gelatinization of most starch granules (31). Thus, despite improving appearance and taste, the added malt has an unfavorable effect on GI values.
Kneading dough mechanically and allowing it to rise in the baking process generates a porous internal structure that, along with high gelatinization and high starch-protein interactions, grants access to salivary and pancreatic α-amylases (31, 33). Therefore, GI values for the traditional flatbreads Barbari and Sangak are quite high. Based on studies, the bread structure is more effective than the amount of fiber, in terms of glycemic response (31, 34, 35). Therefore, Barbari, Sangak, and porous rye bread have higher GI levels than Lavash and Taftoon, which are thin one-layer flatbreads (36) with a short baking time (starch granules do not gelatinize), and dense barley bread. In line with this study, the results of Musa-Veloso et al.’s meta-analysis (35) indicated that consuming bread and pasta made with whole-wheat flour (compared with refined-wheat bread and pasta) would not reduce postprandial blood glucose (35). Another reason suggested by the studies is that fact that larger particle size of whole grains comparing fine flour might be important in preserving the glycemic benefits of wholegrain wheat, due to the effect of cell-wall protection against amylase having a beneficial effect on blood glucose response (33, 34, 37).
The GI values of plain white rice and plain brown rice are consistent with the International Table of the Glycemic Index, which reports a wide range of GI values from 41 to 100 for white rice, and from 50 to 66 for brown rice (8). These wide ranges of the GI values of rice can be justified due to the fact that rice GI depends on several factors, including cultivation location (which affects starch and the ratio of amylose to amylopectin), treatment after harvest (milling), and the process and duration of cooking (which affects the digestion of starch due to gelatinization during the heating process by breaking the molecular arrangement among the starch granules) (38). A similarly high GI value was observed for the common, traditional dish of white rice and lentils. In contrast, the same dish made with brown rice had a low mean GI of 55, which might be due to the higher ratio of rice to lentils (2 to 1); this is maybe an important factor to predict GI.
Furthermore, one benefit of brown rice is decreasing blood glucose response, possibly due to bran layers, limiting the gelatinization of starch granules and serving as a barrier to digestive enzymes, thereby decreasing GI (38) but to address this aspect, it is recommended conducting a study regarding molecular and botanical structures.
The strengths of this study include calculating the GI values of the two main staple food in Iran using a standardized GI protocol, with 3 reference foods tested for each test food, and using the same strain of rice for the comparison of white and brown rice such that the impact of bran in lowering GI values could be demonstrated. In addition, this study excluded outliers from the collected data and observed a 2-day washout to avoid carry-over effects. A potential limitation was that only one popular variety of Iranian rice was studied. In future studies, other varieties should be investigated. Also, the authors acknowledge that the number of participants was limited, and it was not possible to completely control their diets and other activities, which could impact GI measurements. Therefore, further large-scale, more controlled studies could improve the reliability of the findings.
5.1. Conclusions
The results of this study indicate that the most common sources of carbohydrates in Iranian diets have relatively high GI values, which could be a contributing factor in the increasing rates of obesity and T2D. The results also show a great potential to reduce overall GI values in Iranian diets by encouraging barley bread consumption, and by replacing white rice with brown rice or a mixture of brown rice and lentils.