1. Background
Addiction is a reversible disorder that could cause social problems and is characterized by an array of physical, social, and psychological impacts (1, 2). Over 256 million people aged 15 - 64 across the word suffer from substance use disorder (3). According to the United Nations Office on Drugs and Crime (UNODC) in 2019, more than 35 million people across the world have substance use disorders, of which only one-seventh receive treatment (4).
In recent years, with increasing the drug production around the world, a variety of substances have been produced most notably cannabis, marijuana, and caffeine from the soft drugs category, as well as heroin, cocaine, and methamphetamine from the hard drugs category. In recent years, methamphetamine has been widely used as an addictive substance and it was used only in the US by 1600000 people in 2017 (5, 6). Although reviewing the relevant studies resulted in finding no accurate and exact statistics about methamphetamine use and users in Iran (7, 8), methamphetamine has become one of the most commonly used industrial addictive substances in Iran and the number of users has increased over the last years (8-10).
Methamphetamine is a potent nerve stimulant and is mainly a laboratory-manufactured product and large amounts of this substance can be domestically produced (11). In combination with ketamine, methamphetamine is produced in the form of a tablet known as ecstasy. Methamphetamine has neurotoxic effects and long term use of this substance is associated with harmful effects on neurotransmitters. In addition, methamphetamine dependence is associated with neuropsychiatric disorder (12).
Different approaches have been proposed for the treatment of substance use disorders, in particular for methamphetamine use (13, 14). These treatments, depending on the type of addictive substance, include psychological interventions and medication therapies. However, studies reported that medication therapies could fail without considering psychological and social interventions (15).
The psychological therapies mainly aim to change the behavior related to the substance use disorder (16). Examples of psychological therapies include motivational enhancement therapy (MET) (17), cognitive-behavioral therapies (18), and relapse prevention therapy (18, 19).
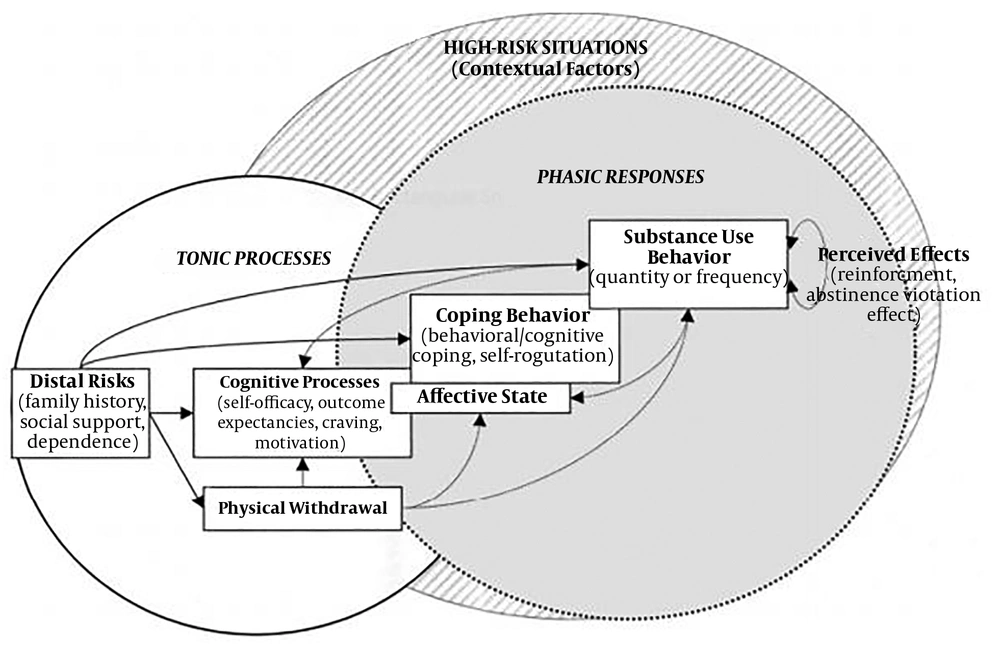
In psychological therapy, studies referred to Marlatt’s cognitive-behavioral model of relapse composed of a number of determinants (20-22). These determinants are regarded as an indicator for indicating the likelihood of relapse to substance use (18). The determinants are divided into intrapersonal and interpersonal categories. The first category includes determinants, such as a sense of self-efficacy, outcome expectancies, craving, motivation, coping with stress and temptation, and emotional states (23). The second category emphasizes social support and environmental stimuli (24).
The high cost of treatment and the lack of cost coverage by insurances are among the issues that hinder patients’ participation in recovery plans (25, 26). However, changes to existing therapeutic systems and applying the combination of technology-based therapeutic approaches with conventional ones could be effective (27). Over the last years, there has been an increase in popularity of smartphone use due to their low cost and ease of use that have increased the use of these devices in healthcare (28). According to the studies, individuals with substance use disorder who use technology-based therapeutic approaches, such as smartphone applications are more likely to manage their recovery successfully (25, 26, 29). For this reason, several studies have been conducted in recent years that aimed at designing mobile applications for relapse prevention to substance and alcohol use disorders. Research indicates the potential of smartphone applications in providing educational information about methamphetamine use disorder (30). In a study by Birrell et al. (31), a mobile application was developed for providing evidence-based information about methamphetamine to the public. According to the results of this study, the majority of participants remarked that the application was likely to improve their awareness and understanding of methamphetamine use disorder (31).
In their study, Zhu et al. (32), developed a mobile application based on cognitive approach for improving cognitive impairment and decision-making risk in patients with methamphetamine use disorder. The findings showed that the application could help to improve cognitive impairment and impulsive control (32).
2. Objectives
As discussed above, there have been studies addressing the adoption of mobile applications in treatment of patients with substance use disorder. However, limited research addressed the use of mobile applications in relapse prevention to methamphetamine use disorder. This study aimed to develop and evaluate a mobile application for relapse prevention to methamphetamine use disorder with an approach to Marlatt’s cognitive-behavioral model.
3. Patients and Methods
This study was conducted in two main stages in 2018.
3.1. Software Production
Initially, a literature review was conducted with a focus on the Marlatt’s cognitive-behavioral model (Figure 1). In addition, there was a direct visit to an addiction recovery center to seek experts’ opinion about the subject of the study and to obtain a better understanding of relapse to substance use (methamphetamine) disorder and the associated factors. The views of clinical psychologists and exerts in addiction studies were sought in software production.
Marlatt’s cognitive-behavioral model (33)
The conceptual modeling of the software included functional, structural, and behavioral models. The programming of the application was conducted using the html, JavaScript, and CSS languages in the Apache Cordova platform to make sure that the application can be run on a variety of operating systems on smartphones.
3.2. Software Evaluation
Five experts (three clinical psychologists and two experts in addiction studies) together with five patients with methamphetamine use disorder participated in the quantitative evaluation of the application in an addiction recovery center. Patients were randomly selected to take part in this step. The data collection tool was a questionnaire developed based on relevant resources (34-37). The questionnaire was composed of three sections (content quality, learning objectives, and usability) on a-five point Likert scale ranging from very good (score 5) to very poor (score 1). The validity of the questionnaire was checked by five domain experts. The reliability of the questionnaire was also determined by calculating the internal consistency of the questions (α = 0.87). Participants were involved in the study on a voluntarily basis and the study was checked in terms of ethical considerations by the Research Ethics Committee of Shahid Beheshti University of Medical Sciences (ref: IR.SBMU.RETECH.REC.1395.886).
4. Results
4.1. Findings Related to the Design and Production of the Application
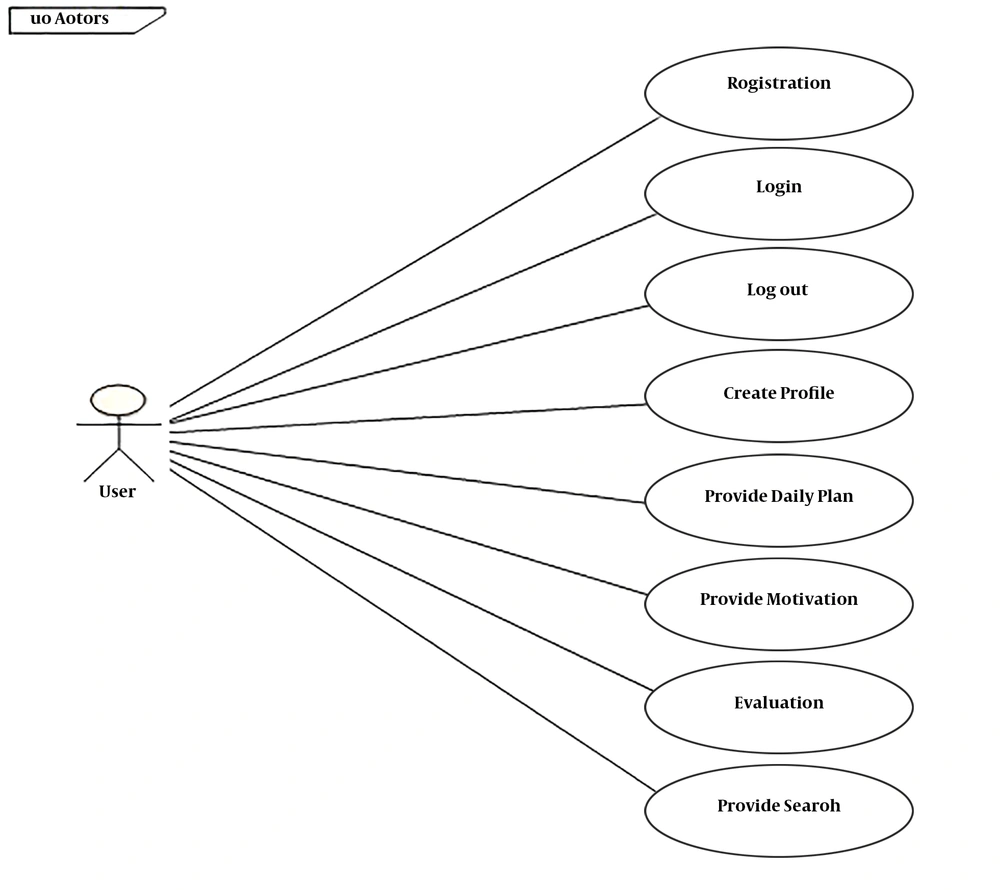
Based on Marlatt’s model and experts’ opinion, the functional requirements of the application shown in Table 1 were determined, and the related scenarios and use-cases were designed accordingly. Figure 2 illustrates the overall use-case diagram of the application.
| Functional Requirements | Description |
|---|---|
| Registration | To enable the user to be registered |
| Log-in | Allowing the user to enter in the application using ID and password |
| Log-out | To enable the user to end a session and get out of the application |
| Creating user profile | To enable the user to create his/her profile |
| Setting daily plan | The application should have a daily recovery plan including: educational content in different formats (the videos, audio, and texts) to create a good understanding of the disorder, its recovery, and risky situations; relaxation through music and videos files |
| Motivational aspects | The application should motivate user with messages, pictures, movies of user’s preference |
| Assessment of the recovery progress | To allow users to go through daily, weekly, and periodical assessment of the recovery process |
| Settings | To provide users to set motivational messages, reminders, and alerts based on their defined times |
| Presentation of assessment reports | The application should display user-completed Assessments to the therapist. |
| Navigation | To allow user to search within educational materials (textual, audio, and video files) |
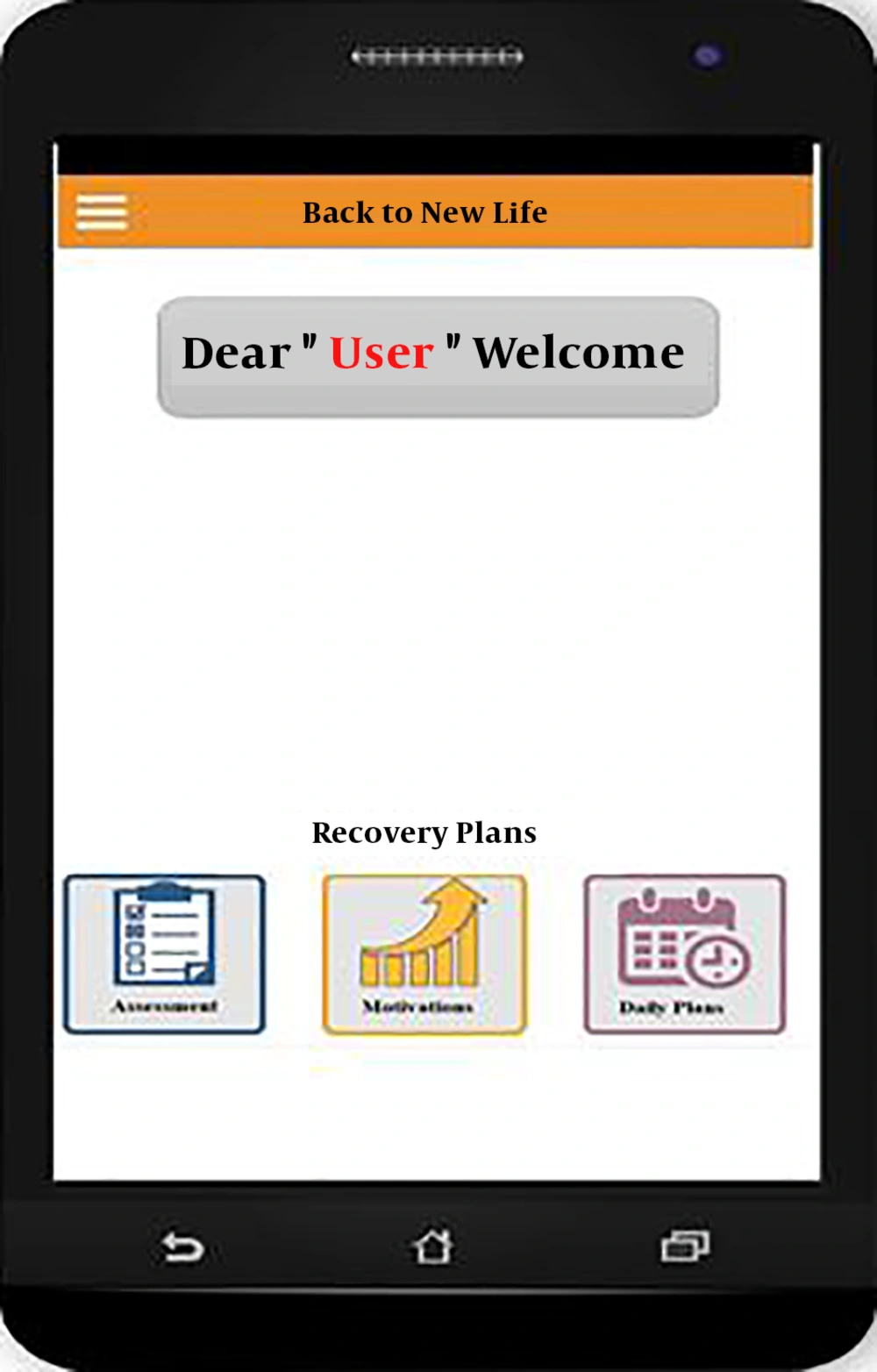
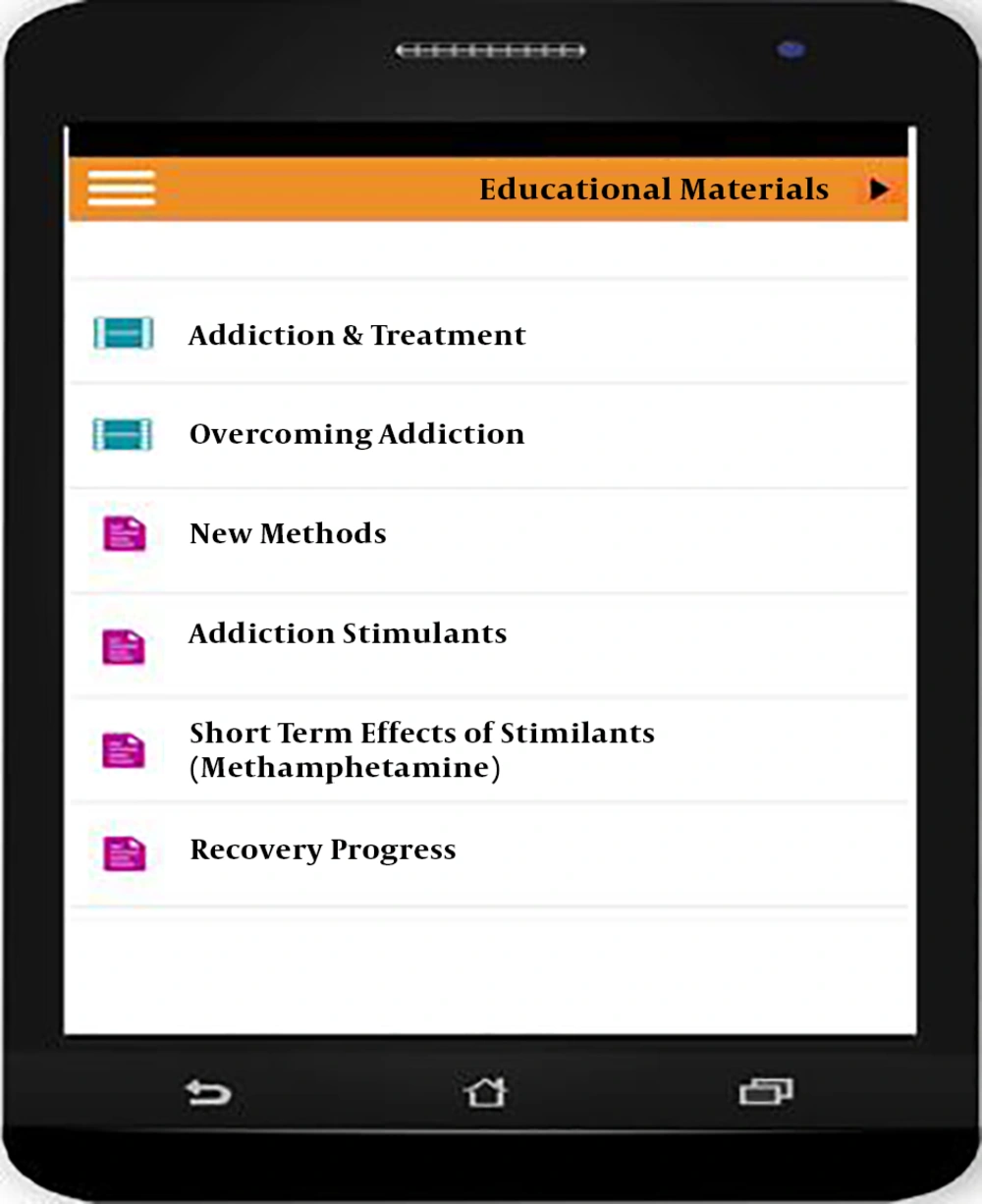
As shown in Figure 2, there were eight use-cases for the application. The application was developed based on its conceptual modeling. Figures 3 - 5 illustrates the screens for recovery plans, daily plan, and educational materials, respectively.
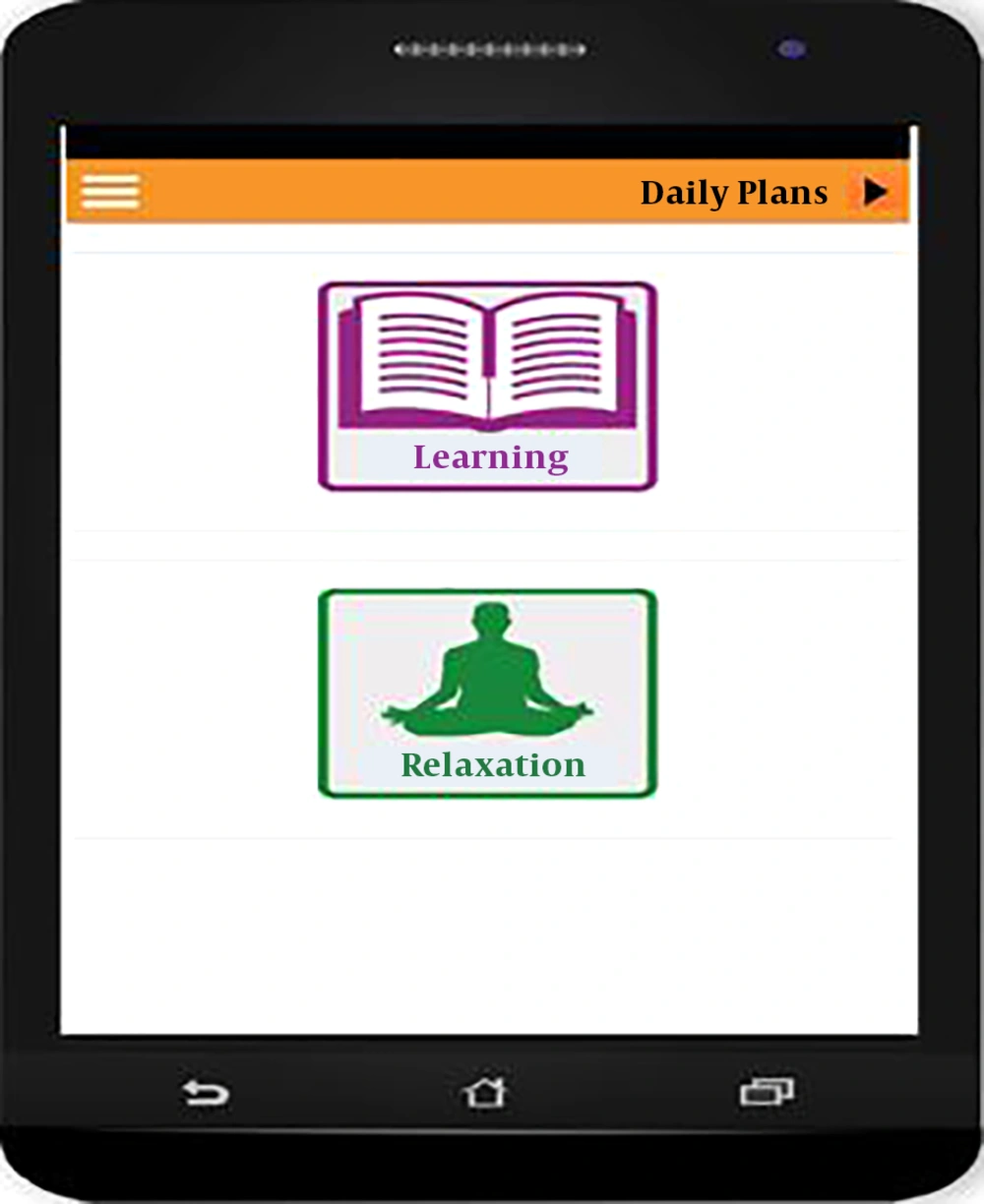
According to Figure 3, the recovery plans are composed of three parts: daily plan, motivation, and assessment. By clicking on the daily plan, the user is transferred to this section composed of education and relaxation (Figure 4).
In the screen for daily plan, by clicking on education icon, the user is transferred to educational material screen (Figure 5).
4.2. Findings Related to Evaluation of the Application
The results of evaluation of the application by experts and by patients are shown in Tables 2 and 3, respectively. According to Table 2, the highest mean score was assigned to usability of the application (4.6 ± 0.39). Content quality (4.5 ± 0.46) and learning objective (4.4 ± 0.37) of the application were in the second and third order, respectively. The results of the evaluation for patients indicated that usability (4.6 ± 0.39) and content quality (4.5 ± 0.33) had the highest mean scores, while the mean score for learning objectives was lower than two other dimensions (4.1 ± 0.37).
| Evaluation Dimensions | Option (Score) | Values | |||||
|---|---|---|---|---|---|---|---|
| Very Good (5) | Good (4) | Fair (3) | Poor (2) | Very Poor (1) | Total | ||
| Content quality | |||||||
| Accuracy | 5 | 0 | 0 | 0 | 0 | 25 (100) | 5.0 ± 0 |
| Reliability of resources | 4 | 1 | 0 | 0 | 0 | 24 (96) | 4.8 ± 0.44 |
| Conciseness and comprehensiveness | 0 | 4 | 1 | 0 | 0 | 19 (76) | 3.8 ± .44 |
| Educational aspects | 2 | 3 | 0 | 0 | 0 | 22 (88) | 4.4 ± 0.54 |
| Cultural aspects | 3 | 2 | 0 | 0 | 0 | 23 (92) | 4.6 ± 0.54 |
| Total | 14 | 10 | 1 | 0 | 0 | 113 (90.4) | 4.5 ± 0.46 |
| Learning objectives | |||||||
| Focusing on user needs | 1 | 4 | 0 | 0 | 0 | 21 (84) | 4.2 ± 0.44 |
| Feedback presentation | 5 | 0 | 0 | 0 | 0 | 25 (100) | 5.0 ± 0 |
| Achievability | 1 | 4 | 0 | 0 | 0 | 21 (84) | 4.4 ± 0.54 |
| Total | 7 | 8 | 0 | 0 | 0 | 67 (89) | 4.4 ± 0.37 |
| Usability | |||||||
| Fonts | 4 | 1 | 0 | 0 | 0 | 24 (96) | 4.8 ± 0.44 |
| Screen design and layout | 3 | 1 | 1 | 0 | 0 | 22 (88) | 4.4 ± 0.89 |
| Terminology | 3 | 2 | 0 | 0 | 0 | 23 (92) | 4.6 ± 0.54 |
| Ease of use | 5 | 0 | 0 | 0 | 0 | 25 (100) | 5.0 ± 0 |
| Ease of learning | 5 | 0 | 0 | 0 | 0 | 25 (100) | 5.0 ± 0 |
| Navigation (speed and structure) | 5 | 0 | 0 | 0 | 0 | 25 (100) | 5.0 ± 0 |
| Minimum technical requirements | 0 | 3 | 2 | 0 | 0 | 18 64 () | 3.6 ± 0.54 |
| Compatibility with different platforms | 4 | 1 | 0 | 0 | 0 | 24 (96) | 4.8 ± 0.44 |
| Total | 29 | 8 | 3 | 0 | 0 | 186 (93) | 4.6 ± 0.39 |
| Total | 50 | 26 | 4 | 0 | 0 | 366 (91) | 4.6 ± 0.38 |
aValues are expressed as mean ± SD or No. (%).
| Evaluation Dimensions | Option (Score) | Values | |||||
|---|---|---|---|---|---|---|---|
| Very Good (5) | Good (4) | Fair (3) | Poor (2) | Very Poor (1) | Total | ||
| Content quality | |||||||
| Accuracy | 5 | 0 | 0 | 0 | 0 | 25 (100) | 5.0 ± 0 |
| Comprehensibility | 1 | 4 | 0 | 0 | 0 | 21 (84) | 4.2 ± 0.44 |
| Conciseness and comprehensiveness | 3 | 1 | 1 | 0 | 0 | 22 (88) | 4.6 ± 0.54 |
| Educational aspects | 3 | 2 | 0 | 0 | 0 | 23 (92) | 4.6 ± 0.54 |
| Cultural aspects | 1 | 4 | 0 | 0 | 0 | 21 (84) | 4.2 ± 0.44 |
| Total | 13 | 1 1 | 1 | 0 | 0 | 112 (89) | 4.5 ± 0.33 |
| Learning objectives | |||||||
| Focusing on user needs | 0 | 3 | 2 | 0 | 0 | 18 (72) | 3.6 ± 0.54 |
| Feedback presentation | 3 | 2 | 0 | 0 | 0 | 23 (92) | 4.6 ± 0.54 |
| Total | 3 | 5 | 2 | 0 | 0 | 41 (82) | 4.1 ± 0.37 |
| Usability | |||||||
| Fonts | 4 | 1 | 0 | 0 | 0 | 24 (96) | 4.8 ± 0.44 |
| Screen design and layout | 0 | 4 | 1 | 0 | 0 | 19 (76) | 3.8 ± 0.44 |
| Terminology | 5 | 0 | 0 | 0 | 0 | 25 (100) | 5.0 ± 0 |
| Ease of use | 4 | 1 | 0 | 0 | 0 | 24 (96) | 4.8 ± 0.44 |
| Ease of learning | 4 | 1 | 24 (96) | 4.8 ± 0.44 | |||
| Navigation (speed and structure) | 5 | 0 | 0 | 0 | 0 | 25 (100) | 5.0 ± 0 |
| Minimum technical requirements | 0 | 3 | 2 | 0 | 0 | 18 (72) | 3.6 ± 0.54 |
| Compatibility with different platforms | 4 | 1 | 0 | 0 | 0 | 24 (96) | 4.8 ± 0.44 |
| Total | 26 | 11 | 3 | 0 | 0 | 183 (91) | 4.6 ± 0.39 |
| Total | 42 | 27 | 6 | 0 | 0 | 336 (84) | 4.2 ± 0.38 |
aValues are expressed as mean ± SD or No. (%).
5. Discussion
According to Marlatt’s model, individuals’ cognition of their substance use disorder and the ways of coping with temptations are key determinants for relapse prevention, and patients with substance use disorder should be provided with educational material. Marsch (38), reported that technology-based therapeutic approaches could help improving the outcomes of addiction recovery. In the present study, a key service of the application develop was assigned for patient education including audio, video, and textual materials. This was in line with Gustafson et al.’s (27) study, in which a mobile application was developed to improve outcome for people undergoing alcohol dependence recovery. In their application, there was a specific section for patient education with audio and textual materials to help patients cope with temptation. The findings of the current study and those reported by Gustafson et al. (27), remark the key role of education in relapse prevention. Therefore, developing mobile applications with educational capabilities for people with methamphetamine use disorder appears to improve the recovery outcomes.
In addition to patients’ education, relaxation plays a critical role in relapse prevention and follow up of treatment after patients’ discharge from recovery centers (39). In the current study, there was a relaxation service, as part of the recovery daily plans, to help patients overcome with stress and substance use temptation. This was supported by Gustafson et al. (27), who considered a relaxation capability for their application, which provided users with audio materials. These findings suggest that the relaxation service of applications could improve the coping behavior referred to the phasic responses of the Marlatt’s model, and considering this capability of the software is therefore suggested in the development of similar applications.
In the current study, a key function of the application was the motivational capability. The application should permit patients to develop the motivation part of the application based on their own preferences with audio, video, and textual materials. This is supported by Gustafson et al. (27), who reported such a capability for their application. With respect to the tonic process highlighted in the Marlatt’s model (29), attention should be paid to the cognitive processes, part of which refers to the role of motivation in relapse prevention. Therefore, developing the motivation capability of the application by patients might help them to have a better feeling about the recovery process.
Reminding different stages of treatment and the progress of recovery, as well as generating messages for motivation were among the key functions of the application designed in the current study. This findings is in line with other studies, as the application designed in Gustafson et al.’s (27) study supported patients’ in their recovery through generating reminders for continued use of the application and motivation messages. This is also consistent with Stoner and Hendershots (40) study in which a mobile application called AGATE was designed with the capability of sending reminder messages to patients undergoing recovery for alcohol use disorder to improve their adherence to the recovery plans, such as medications that should be taken.
In their study, Bock et al. (41) indicated the positive role of motivational messages sent via short message service (SMS) in smoking cessation intervention. The continuity of treatment and adherence to recovery plans are critical in treatment of people with substance use disorder. Failure in these respects could increase the possibility of relapse to substance use and would be a waste of resources both for patients and for care providers (42). Given the high likelihood of relapse in methamphetamine use disorder and the necessity of follow up after initial recovery, the current study aimed to develop an application for improving the outcome of the recovery process. The findings of the current study and those presented above in other studies could support this notion that capabilities such as, reminder and motivation messages, as key functions of the applications used for relapse prevention, could help improving the sense of self-efficacy, outcome expectancies, and coping behavior, as well as self-regulation.
In the current study, the results of the application evaluation indicated that 88% of participants were satisfied with content quality, learning objectives, and usability of the application. Among the three dimensions of evaluation, the highest score was assigned to content quality of the application from both patients and expects’ points of view, which appeared to be associated with accuracy and different information formats of the educational content. This was in line with Walters et al.’s (43) study, which aimed at developing a web-based system for treatment of patients with substance use disorder. A satisfaction rate of 92% was reported for the audio content and data integrity of the application. The similarity of the results could be due to considering key designing principles and the context of use of the systems.
Design and deployment of mobile applications, such as the application developed in the current study could be a complementary approach to the therapeutic and psychological treatments to prevent relapse to substance use disorders. After investigating the impact of this application on relapse prevention to methamphetamine use in interventional studies and further development of the application based on evaluations with larger sample sizes, it could be used by relevant care centers for improving the outcome of addiction recovery.