1. Background
The prevalence of alcohol and illicit drug use in adolescents between the ages of 12 and 17 years remains a growing concern in the United States. The use and misuse of substances in adolescence are critical to address, as this period of growth and development is crucial for emotional, behavioral, and psychosocial adjustment (1). In 2018, the Substance Abuse and Mental Health Services Administration (SAMHSA) published the national survey results depicting the increasing use of substances among adolescents (2). Specifically, the report showed a 23.9% prevalence of lifetime use of alcohol and/or illicit drugs, with 16.7% reporting the use within the past year. This continual rise of use within this age group, coupled with the low rates of treatment-seeking and treatment completion (3), highlights a need for innovative adolescent addiction treatment interventions. Such innovative interventions should aid in treatment engagement and completion, as well as the reduction of substance use and associated psychosocial concerns.
Researchers have denoted the need to refine adolescent addiction treatment to enhance engagement and treatment completion, as well as recovery-related outcomes (4, 5). In 2018, approximately one in 26 adolescents in the United States needed treatment for a substance use disorder and related symptoms; however, the data showed that only approximately 16.8% received services (2). For those adolescents that use treatment, programs are often building on singular treatment modalities. Despite these treatment modalities with moderate efficacy, adolescents with addiction continue to disengage early from treatment, and overall outcomes can still improve (4). To this end, previous literature has suggested combining treatment strategies, often considered as complementary interventions, to increase the overall impact on the clients served (3, 6). Complementary counseling strategies, when integrated into standard treatment, have the potential to enhance treatment outcomes. This integration should seek to build on the theoretical underpinnings of standard treatment to enhance the counseling outcomes (3).
One such treatment strategy is the integration of equine facilitated psychotherapy (EFP) into a choice theory-driven treatment intervention for adolescents with substance use disorders. While the choice theory as a stand-alone treatment has shown efficacy (7), resistance and disengagement are often quite high in adolescence, which can negatively impact the quality of treatment. Integrating EFP as a complement to standard treatment, such as the choice theory, offers a buffer for the client-counselor dynamic, often where resistance stems (8). Further, the bond development between client and equine often transfers to the client-counselor relationship, providing an additional reduction in resistance and disengagement (9, 10). The use of EFP within the treatment of adolescent addiction has also been previously examined. Individuals with substance use disorders often demonstrate feelings of fear or reluctance to engage in treatment due to stigmatizing experiences in their environment (11). The integration of horses as part of the addiction treatment programs is particularly powerful as horses do not judge based on past behaviors; rather horses will evaluate and respond to the here-and-now experiences or interactions.
The integration of EFP in adolescent addiction treatment has also demonstrated an increase in treatment completion rates. Kern-Godal et al. (12) examined the impact of an equine assisted therapy (EAT) program within standard day treatment services for adolescents over an 18-month treatment period. The results demonstrated a significant association between participation in the EAT group and successful treatment completion. Participants in the EAT group were significantly more likely to remain on treatment for over 90 days than the group receiving usual treatment. Extending time-in-treatment is important for adolescents with addiction as research demonstrates that early treatment drop-out is highly correlated with relapse and other negative outcomes (5), including increased psychosocial symptomology (e.g., depression, anxiety) and behavioral problems (7). This further demonstrates the need for innovative approaches to adolescent substance use disorder treatment to enhance the multifaceted outcomes associated with successful treatment.
2. Objectives
The purpose of this study was to examine the influence of an innovative EFP intervention integrated into choice theory treatment on psychosocial and behavioral outcomes of adolescents with substance use disorders. The intervention in this study was founded in the seven connecting habits posited by Glasser (13) to affect adolescents’ behaviors, enhance the positive behavioral traits associated with improved psychosocial well-being, and increase treatment engagement and completion.
3. Patients and Methods
3.1. Participants
Participants were 10 adolescents referring to the study by a local residential provider in a medium-size rural city in the southeast US. The eligibility criteria for study participation included being eight to 17-years-old, being medically and psychiatrically stable, and having an active diagnosis of a substance use disorder. The participants’ age ranged from 14 to 17 years. There were six males (60%) and four females (40%). The participants reported ethnicities as African Americans (n = 5; 50%), Caucasian (n = 4; 40%), and Biracial (n = 2; 10%). A total of 10 participants (100%) completed the study in its entirety, from intake to posttest measure completion.
3.2. Procedure
The participants referred for enrollment in the study were screened by study personnel to ensure that they met the eligibility criteria. Eligible participants were adolescents aged 11 - 17 years with an active substance use disorder diagnosis, medical and psychiatric stability, and parental consent to participate. For those meeting the criteria, study personnel reviewed the Institutional Review Committee informed consent with the participants’ parents and obtained informed consent from the participants. As the participants were minors, they required parental consent beyond providing their assent to participate. The participants then completed the pretest of each of the three measures in the study. Upon completion of the baseline measures, the participants engaged in a six-session EFP group intervention. After the final EFP group session, each participant completed the posttest of the same three measures.
3.2.1. Intervention Protocol
A six-week protocol, consisting of six 1.5-h sessions, was developed with a choice theory/reality therapy foundation. The participants engaged with program equine(s) for one hour and then engage in a half-hour group therapy session about their experience. Each session’s theme was developed based on Glasser’s (13) connecting behaviors. These behaviors included listening, trusting, supporting, encouraging, respecting and accepting, and negotiating differences. The staff involved in each session included an addiction counselor, an equine specialist, and a horse trainer. The addiction counselor observed the participants’ interactions with the horses and processed with the participants for a half-hour after the equine interaction. The equine specialist observed the horses’ behaviors in response to the participants, helped translate the nonverbal feedback, and participated in the group processing after the equine intervention. The horse trainer explained the horsemanship skill the participants were learning and demonstrated the skill for the participants.
The six sessions were designed around a therapeutic goal and a horsemanship goal. The following is a breakdown of each session’s therapeutic goal, horsemanship goal, and equine activities. A description of the activities included in each section is detailed in Appendix 1 in Supplementary File.
Session 1: Listening. The therapeutic goals for session one were (A) to experience a connection with the horse and build confidence in the participants’ understanding of nonverbal cues, spatial cues, boundaries, and self-awareness; (B) to experience how listening to one’s environment can influence connection with the horse and others; and (C) to experience how paying attention to nonverbal cues (self-awareness and awareness of others) can change one’s connection to others. The horsemanship goals were (A) to learn and pay attention to the horses’ non-verbal communication facilitated through one-one interaction with the horse and grooming and (B) to recognize the impact of the one’s nonverbal language on the horse and the connection between the horse and the human. The following activities were structured to help facilitate the participants’ awareness of their ability to listen and the effect it has on connection with the horse and others.
Session 2: Trusting. This session of the program focused on trust. The therapeutic goal was to experience the feeling of being trusted and trusting with the horse, other group members, and facilitators. The horsemanship goal was to identify how horses communicate in a herd. The activities consisted of herd observation, catching the horse in the field, and leading the horse into the barn. Grooming for connection was repeated to continue to establish trust.
Session 3: Supporting. This session focused on supporting. The therapeutic goals were (A) to practice staying connected to others and understand the importance of mindfulness in connecting and supporting and (B) to experience how supporting one another in an activity contributes to achievement as a whole group. The horsemanship goals were (A) to demonstrate a supportive role in partnership with the horse to earn horse’s confidence enough to follow directions and (B) to perform a drill team as a group partnering with horses. The activity during this session was mindful leading.
Session 4: Encouraging. This session focused on encouraging. The therapeutic goal was to demonstrate empathy and encouragement as others attempted tasks with their horse partner. The horsemanship goal was to lead their horse through an obstacle course, focusing on staying connected and helping the horse feel confident and safe. The activity for this session was for participants to set up obstacle course 1 as a group.
Session 5: Respecting and accepting. This session focused on respecting. The therapeutic goal was to learn effective coping skills for overcoming adversity within a group while respecting the decisions and views of others. The horsemanship goal was to safely rope halter the horse and teach the horse to circle the individual when attached to a long rope in both directions. The activity for this session was the circle game.
Session 6: Negotiating differences. The last week focused on negotiating differences. The therapeutic goals were (A) to learn problem-solving in difficult situations and (B) to find a common resolution as the desired outcome. The horsemanship goal was to learn how to influence a horse’s movement using just body language and teamwork, without a halter or a lead rope. The activity for this session was for the group of the participants to guide a horse through obstacle course 2.
3.2.2. Ethics
The study was reviewed and approved by the University and Medical Center Institutional Review Committee. Additionally, as equines were included as part of the intervention, the study was reviewed and approved by the Institutional Animal Care and Use Committee. To ensure the quality of care and oversight of the equines taking part in the intervention, each session required an equine specialist for their well-being and safe handling.
3.3. Measures
3.3.1. Adolescent Behavior Survey
The Adolescent Behavior survey (ABS) is a five-item, self-report questionnaire measuring the frequency of behaviors demonstrated by an adolescent. The ABS is an adapted version of the Right Stuff Scale developed by Parish (14). The behaviors are based on Glasser’s seven connecting habits, including supporting, encouraging, listening, accepting, trusting, respecting, and working cooperatively. The participants were asked to rate the frequency to which they engaged in the behavior within the last 30-days on a five-point Likert scale (1 = “never” to 5 = “always”).
3.3.2. Patient Health Questionnaire 9
The Patient Health questionnaire 9 (PHQ-9) is a nine-item, self-report questionnaire measuring constructs consistent with depressive symptomology (15). Specifically, the constructs include the lack of interest, depressed mood, sleeping difficulties, tiredness, appetite problems, negative feelings about self, tiredness, psychomotor agitation/retardation, and suicidal ideation. The participants were asked to rate the frequency of concerns connected to these constructs within the past two weeks on a four-point Likert scale (0 = “not at all” to 4 = “nearly every day”). The psychometric properties of the PHQ-9 have been validated in primary care mental health and addicted populations (15).
3.3.3. Generalized Anxiety Disorder 7
The generalized anxiety disorder 7 (GAD-7) scale is a seven-item, self-report questionnaire measuring constructs consistent with anxiety (16). Specifically, the constructs include panic, social anxiety, and post-traumatic stress symptomology. The participants were asked to rate the frequency of concerns connected to these constructs within the past two weeks on a four-point Likert scale (0 = “not at all” to 4 = “nearly every day”). The psychometric properties of the GAD-7 have been validated in mental health and addicted populations (16).
4. Results
4.1. Adolescent Behavior
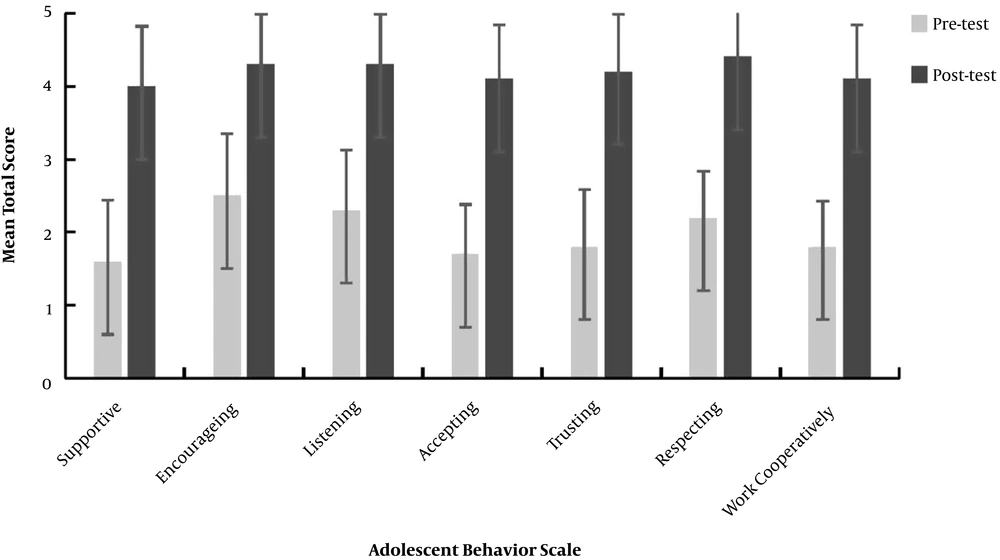
Figure 1 depicts the results of the paired-samples t-tests to compare the pretest and posttest measures of the seven categories of the Adolescent Behavior Survey. For the “supportive of others” category, there was a significant difference between the pretest (M = 1.60, SD = 0.84) and posttest (M = 4.00, SD = 0.82) results [t(9) = 14.70, P < 0.001]. For the “encouraging of others” category, there was a significant difference between the pretest (M = 2.50, SD = 0.85) and posttest (M = 4.30, SD = 0.68) results [t(9) = 13.50, P < 0.001]. For the “listen to others” category, there was a significant difference between the pretest (M = 2.30, SD = 0.82) and post-test (M = 4.30, SD = 0.68) results [t(9) = 13.42, P < 0.001]. For the “accepting of others” category, there was a significant difference between the pretest (M = 1.70, SD = 0.68) and posttest (M = 4.10, SD = 0.74) results [t(9) = 14.70, P < 0.001]. For the “trusting of others” category, there was a significant difference between the pretest (M = 1.80, SD = 0.79) and posttest (M = 4.20, SD = 0.79) results [t(9) = 10.85, P < 0.001]. For the “respectful of others” category, there was a significant difference between the pretest (M = 2.20, SD = 0.63) and posttest (M = 4.40, SD = 0.70) results [t(9) = 5.07, P < 0.001]. For the “work cooperatively with others” category, there was a significant difference between the pretest (M = 1.80, SD = 0.63) and posttest (M = 4.10, SD = 0.74) results [t(9) = 8.84, P < 0.001]. These results suggest that the six-session EFP program could affect the seven categories of adolescent behavior. Specifically, the results suggest that adolescents with substance use disorders who completed the EFP intervention showed promotions in behaviors associated with the Glasser’s (13) seven connecting habits.
4.2. Psychosocial Symptoms
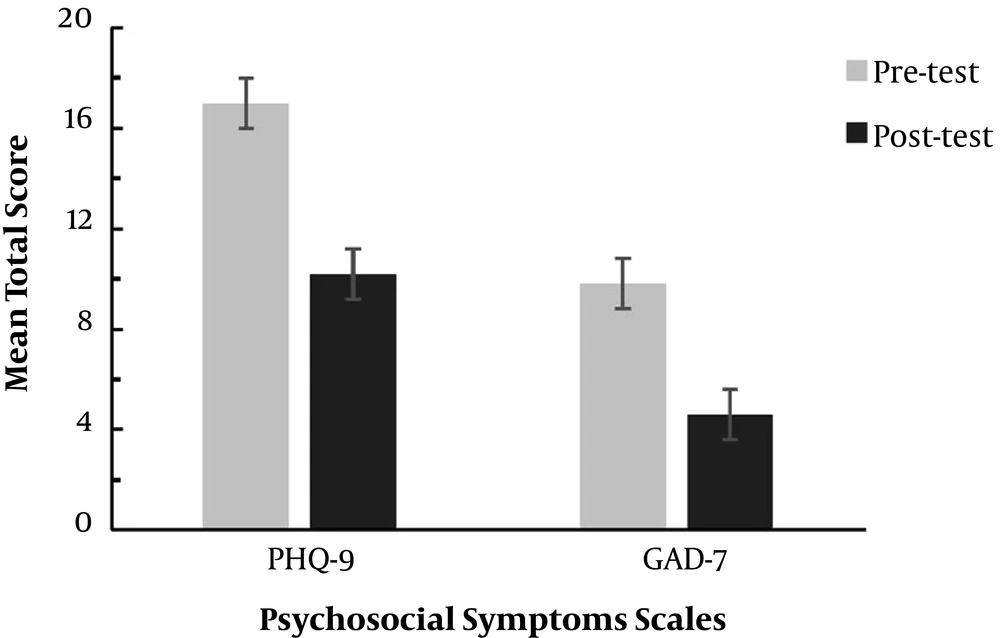
Figure 2 depicts the results of the paired-samples t-tests to compare the pretest and posttest measures of the total score on the PHQ-9, representing depressive symptoms, and the total score on the GAD-7, representing anxiety symptoms. For the PHQ-9, there was a significant difference between the pretest (M = 17.00, SD = 2.16) and posttest (M = 10.20, SD = 1.55) results [t(9) = 18.94, P < 0.001]. For the GAD-7, there was a significant difference between the pretest (M = 9.80, SD = 1.23) and posttest (M = 4.60, SD = 1.90) results [t(9) = 13.38, P < 0.001]. These results suggest that the six-session EFP program could affect psychosocial symptomology. Specifically, the results suggest that adolescents with substance use disorders who completed the EFP intervention showed decreases in depressive and anxious symptomology.
5. Discussion
As adolescents’ substance use continues to rise in the United States, the need for innovative treatment strategies is at a pinnacle. Treatment strategies need to address addiction-related outcomes, as well as underlying psychosocial and behavioral issues related to adolescent addiction (3). This study aimed to examine the impact of an innovative EFP intervention on psychosocial and behavioral outcomes of adolescents with addiction. The results of this pilot study have important implications for the field of adolescent addiction treatment and the integration of EFP interventions. Specifically, the results of this study demonstrated that a six-session group EFP intervention integrated into a choice theory strategy could increase positive connecting behaviors and decrease psychosocial symptoms in adolescents with substance use disorders.
The results of the study demonstrated a significant increase in prosocial adolescent behaviors from baseline to post-intervention. Specifically, an increase was noted in behaviors related to supportiveness, encouragement, listening, acceptance, trusting, respecting, and cooperation. This is consistent with previous literature related to behavioral responses to equine interactions. In particular, Vidrine et al. (17) noted strong positive behavior modifications upon the completion of equine interactions. This finding is important to the field of adolescent addiction, as engagement in negative, non-prosocial behaviors has been linked to the continued use of substances (4) and poor treatment outcomes (5). While the seven connecting behaviors (13) have not been examined in the context of adolescent addiction treatment or EFP, previous literature has demonstrated many examples of the reduction of negative behavioral expressions (18). The current study expands the current literature based on both EFP interventions and adolescent addiction by examining these behaviors in this context. Additionally, the current study addresses concerns posited by El Mallah (18) related to the conceptual specification of prosocial behaviors through the use of Glasser’s (13) well operationally defined seven connecting behaviors.
The results of this study demonstrated a significant reduction in both depressive and anxious symptomology. The mean score reductions on the PHQ-9 (depressive symptoms) and GAD-7 (anxious symptoms) from baseline to post-intervention demonstrated the potential of the EFP intervention to reduce psychosocial symptomology. These results are consistent with those depicted in previous studies. For example, Kemp et al. (10) found that an EFP group intervention was effective in reducing psychosocial symptoms of children and adolescents with sexual abuse histories. Overall, the findings of this study offer further support that EFP interventions for adolescents with behavioral health concerns are effective in reducing psychosocial symptoms, particularly depressive and anxious symptoms (9, 19, 20).
The present study builds upon additional recommendations from previous research. McNamara (21) recommended that EFP studies have a stronger tie or connection to theory. This study integrated the EFP intervention into the choice theory lens, building upon the theoretical foundation. Additionally, previous research has denoted a need to fill the gap between research and practice, in particular related to the elaboration of intervention protocols (22, 23). This study utilized a manualized, six-session group intervention protocol. While the participant responses are unique, each interaction with the equine(s) followed the same protocol, thus improving replicability.
There were limitations associated with this study. The primary limitations were the low sample size and the lack of a control group. Including a control group would allow researchers to determine the influence of an intervention beyond uncontrolled variances (e.g., time, maturation). Additionally, the use of self-report measures can be seen as a limitation to this study. Self-report measures only provide subjective ratings of behavior and psychosocial symptoms. Future research should increase the sample size, use a randomized control group, and seek objective measures to offset the limitations of self-report measurements. Additionally, future studies should explore the use of qualitative or mixed-method designs to specifically elucidate the participant perception on the role of the equine in the intervention experience. This would allow more sophisticated examinations of how the integration of equine interventions enhances the experience and contextualize the perceived influence of the equine as part of the change process.
The present study demonstrated the potential efficacy of an innovative EFP intervention integrated into a choice theory-driven treatment strategy for improving psychosocial and behavioral concerns related to adolescent addiction. Participants reported a significant improvement in the seven connecting behaviors, namely supporting, encouraging, listening, accepting, trusting, respecting, and working cooperatively. Participants also reported a reduction in depressive and anxious symptomology. This intervention has the potential to improve adolescent addiction treatment processes and outcomes. Further, the results of this study add to the literature on EFP and adolescent addiction treatment. The connection to the choice theory, particularly the use of the seven connecting behaviors (13), helps provide a well-defined and conceptualized set of behaviors that can be examined across future studies to improve the comparability and generalizability of results. Additionally, the use of a manualized intervention protocol will improve replicability, a problem that has been noted for EFP and EAT-related studies (20). Despite some limitations with the current study, the results are promising and demonstrate the potential of innovative EFP interventions for impacting treatment outcomes in adolescents with addiction.