1. Introduction
Confrontation with COVID-19 threatens all people of the world. It has caused countless human and economic losses worldwide, even in the most powerful and advanced countries in the world. Researchers around the world are looking to find ways to prevent the disease, reduce the duration of infection and its damage, and treat the virus (1). Although favorable results have not been obtained for prevention or treatment so far, research is ongoing, especially in high-risk groups.
Pregnant women usually experience several anatomical and physiological changes due to adaptation to the specific conditions of pregnancy. Sometimes, the diagnosis of abnormalities in pregnant women is delayed due to physiological changes in the immune system, cardiovascular system, and respiratory system. In some other cases, the symptoms of a pregnant woman are considered as abnormal complications specific to pregnancy (2). Preterm Rupture of Membranes (PROM) and prolonged Rupture of Membranes (ROM) are the problems during pregnancy that lead to consequences such as maternal fever and maternal chorioamnionitis (3). In these cases, the diagnosis of the underlying cause of the fever may be delayed. The present study reports a woman who was hospitalized with PROM and maternal fever. The initial treatment was performed based on the diagnosis and clinical presentation of chorioamnionitis.
2. Case Presentation
The patient was a 29-year-old female G1P0 at 33 weeks’ gestation, with no previous history of underlying diseases or problems in the current pregnancy. The patient had received normal prenatal care based on the instructions of the Ministry of Health of the Republic of Iran. The client’s first and second-trimester screening reported her normal condition. The patient was transferred from a local hospital to a women’s specialized hospital in the provincial capital of Ilam, Iran. The patient’s initial complaint was PROM. The patient’s vital signs showed an abnormal pulse rate (90/min) and temperature (38ºC), although blood pressure and respiratory rate were within normal ranges. She was in the latent phase of labor, with two-finger dilatation, 30% effacement, -3 station, 138-146/min Fetal Heart Rate (FHR), and the leakage of the amniotic sack. Thus, the condition was immediately accepted as a high-risk pregnancy. Initial assessments began for the mother, including regular monitoring and recording of vital signs. Then, all vital signs were checked and recorded every four hours. The mother’s blood ABG was done, as well. Uterine contractions were measured by electrohysterography (EMG) as a non-invasive monitoring device. It utilized surface electrodes applied to the maternal abdomen with high frequency and low noise amplifier. Laboratory tests were requested, including Complete Blood Count (CBC), Blood Groups/Rhesus (BG/Rh), Erythrocyte Sedimentation Rate (ESR), Urea, Creatinine, C-Reactive Protein (CRP), Urine Analysis (UA), and Urine Culture (UC). Abdominal ultrasound was requested to assess the fetal status and amniotic fluid volume. The fetal evaluation was performed by checking and regularly recording the FHR. Treatment for chorioamnionitis began with appropriate intravenous administration of ampicillin, gentamicin, and oral erythromycin. Also, the mother received betamethasone injections to stimulate the fetal lungs and reduce the risk of an infant’s RDS. Due to the fever and confirmed PROM in the mother, the termination of pregnancy was considered for the patient. The patient had a fever, without other symptoms of COVID-19, including sore throat, cough, shortness of breath, lethargy, muscle aches, and diarrhea. Because of the epidemic of COVID-19 in Iran and Ilam, and since the patient’s husband had a dry cough for a few days, a throat swab specimen was obtained from the upper respiratory tract of the patient.
3. Discussion
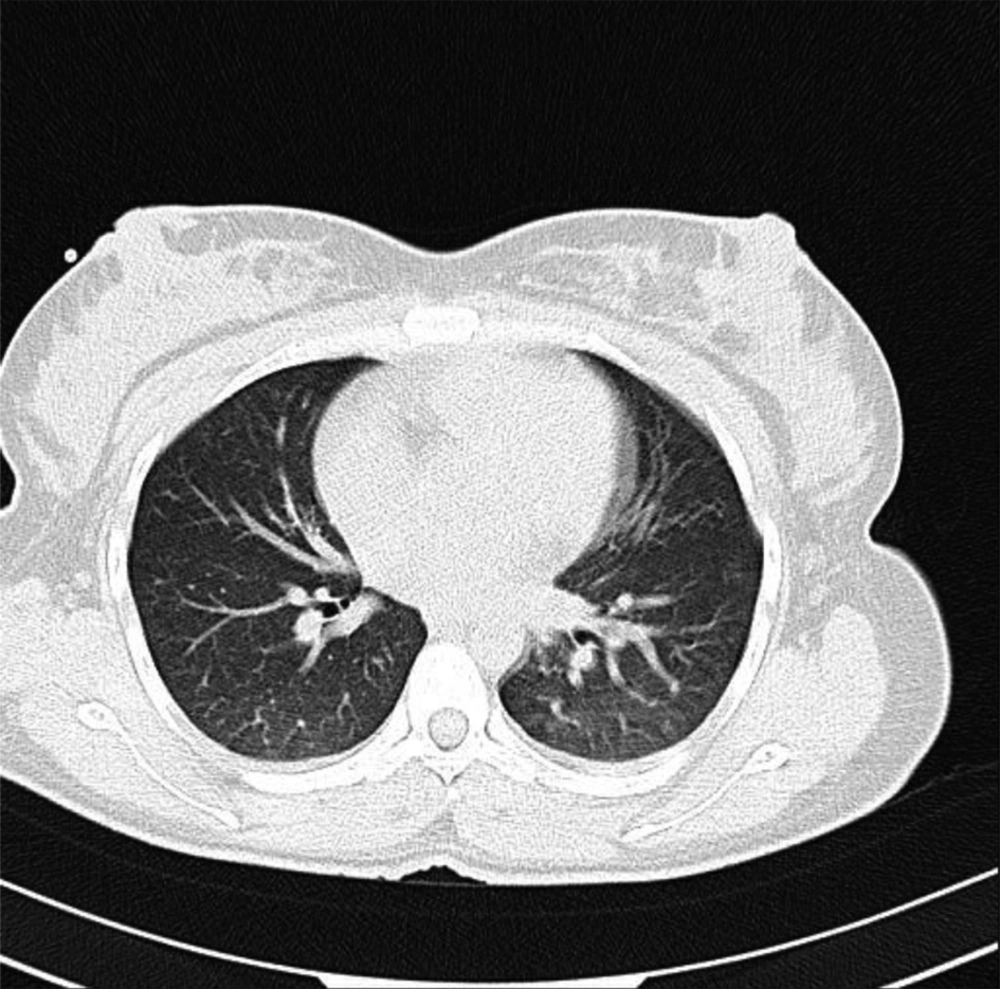
Both ESR and CRP were above the normal range (83 and 2+, respectively). The mother’s blood ABG result showed a pH of 7.41 and PCO2 of 36%. The patients’ O2 saturation was 96%. During the NVD plus Episiatomy, a live female baby with a healthy appearance was born with normal Apgar scores in the first and fifth minutes of delivery (8 and 10, respectively). The RT-PCR assay confirmed that the throat swab of the patient was positive for COVID-19. The test results were announced when the patient had a normal delivery. Because the patient was suspected of COVID-19, all protective processes were done. The newborn was separated from the mother immediately after NVD and transferred to the NICU because of both premature birth and chorioamnionitis. Due to the mother’s positive RT-PCR test, a throat swab specimen was taken from the newborn for RT-PCR. Also, a chest CT scan was done for the mother (Figure 1).
Based on the results, abnormalities in chest CT images and bilateral involvement were detected in the patient; however, the RT-PCR throat swab specimen was negative for the newborn. The patient was transferred to the COVID-19 care unit. She was healthily discharged from the hospital with two negative RT-PCR tests. Her newborn was followed for two weeks, and no symptoms of COVID-19 were reported.
COVID-19 is a dangerous pandemic that has emerged since December 2019 in Wuhan, China (4). Pregnant women are at high risk for the virus, along with the elderly and those with underlying diseases (5). Although some symptoms have been reported as the main symptoms of COVID-19 (6), in the present case, there was only fever without signs of difficulty breathing, cough, weakness, or lethargy, with a normal level of pH and PCO2. There is a contradiction about the probability of vertical transmission from the mother to the fetus during pregnancy (6-10). The RT-PCR throat swab specimen was done for the newborn that showed a negative result. In the present case, the newborn was immediately separated from the mother and fed with formula, like in other studies (7, 8).