1. Background
Psychoactive substances can either stimulate or inhibit the normal function of the central nervous system (1). Globally, the harmful use of psychoactive substances remains a significant threat with considerable negative effects on the financial and relationship aspects of households, communities, and nations. According to the World Drug report (2019), in 2018, 271 million people, or 5.5% of those aged 15 to 64 years, had used drugs in the previous year, which is 30% higher than the 2009 report, as the last report. In 2017, a total of 585,000 people lost their lives due to illicit drug use (2).
The recent report of the Dangerous Drugs Board (DDB) showed that the Philippines has 1.8 million current drug users aged 10 to 69 years old, with 4.8 million having used illicit substances at least once in their lives (3). Moreover, the 2018 statistics on the admission of person who used drugs (PWUDs) in the treatment rehabilitation centers (TRCs) in the country has significantly increased by 34.66% compared to the previous year (3).
Substance abuse has a broad range of short- and long-term, direct and indirect effects to an individual depending on the type of drugs, frequency and amount taken in, and their health status. Short-term effects may lead to significant changes in appetite, daily productivity, elevated blood pressure, sudden change of mood, psychosis, overdose, and death. Long-term addiction may cause macro-and micronutrient deficiencies that can lead to depression, anxiety, and low energy, all of which may result in relapse (4). One of the keys to the holistic recovery of PWUDs is proper nutrition and hydration, as they help regain balance, increasing the chances of recovery.
2. Objectives
Given the importance of nutrition management in drug rehabilitation, this study aimed to evaluate the effects of implementing the nutrition care process on PWUDs management 120 days after its implementation.
3. Patients and Methods
3.1. Study Sites and Sample Size
This study employed a quasi-experimental one-group pretest-posttest design in which a dependent variable was measured for one group of participants following a treatment. Participants were recruited from eight (n = 8) residential TRCs in the Philippines last 2018.
Equating the total population of each study site, the sample size was estimated as 268 PWUDs, based on the 95% confidence level and 5% margin of error, using Slovin’s formula. To determine the number of participants within the 8 TRCs, the proportional allocation was done. Using the provided lists of admitted PWUDs, simple random sampling was done to select the respondents.
3.1.1. Inclusion Criteria
The participants aged 20 to 45 years old of both genders, willing to participate, with signed consent, no food allergies, no severe mental disorder, and no underlying conditions like diabetes, cardiovascular diseases, and kidney disorders.
3.1.2. Exclusion Criteria
Individuals below 20 to 45 years, no signed consent, with a severe mental disorder, food allergies, and suffering from other diseases were excluded from the study.
3.2. The Intervention
One of the interventions was the developed nutrition management guidelines (NMG), which includes the nutrition care process (NCP) and an 8-week standardized cycle menu.
The NCP is comprised of nutritional assessment, diagnosis, intervention, and monitoring and evaluation (ADIME), which is developed to ensure high-quality nutrition care for patients. During the assessment phase, data such as nutrition-related history, anthropometric measurements, nutrition-focused physical observations, client history, and comparative standards were collected. The body mass index (BMI) was used to assess the nutritional status, and all participants were interviewed using standardized questionnaires on socio-economic status, quality of life (QoL), stress levels, psychological distress, and dietary diversity score.
In the diagnosis phase, BMI, dietary diversity, QoL, stress levels, and psychological distress were determined using standard scoring systems.
For the intervention, problems were addressed to help in the improvement of the diagnoses through the manifestations of signs and symptoms. At this stage, activities were created to help patients' progress towards the developed goals. The implementation of the whole process of the NCP and the developed 8–week cycle menu were the interventions given. Along with the provision of the calculated meals as an intervention, registered dietitian nutritionists (RNDs) provided nutrition education through individual nutrition counseling using the sample topics in the NMG (references available in Appendix 1). This is to also promote positive behavior change on health and nutrition among the participants.
3.2.1. Calculated Recipes for PWUDs
Considering the recommendations for PWUDs and the nutrient requirements of Filipinos, the dietary recommendation used for the recipe development is as follows: (1) energy: 2000 kcal, (2) protein: 110 g (22%), (3) carbohydrates: 275 g (55%), and (4) fat: 50 g (23%). The recipes were collected from the Institute’s iFNRI Recipe Library and other recipe books (references available in Appendix 2) and were modified based on the macronutrient distribution range. The energy and nutrient content of the recipes were computed using food composition table (FCT) and Menu Evaluation Software, while Philippine dietary reference intakes (PDRI) was used as reference values in determining percent recommended energy and nutrient intake (RENI) distribution of the recipes. These recipes have high protein, healthy sources of fats, less sugar, caffeine, and less refined carbohydrates. The cost of each recipe was calculated to determine if the actual recipe meets the cost that was suitable for the budget of each patient in the rehabilitation centers (~ 3 USD/day). Recipe standardization and sensory evaluation were done in the kitchen laboratory of the institute.
The monitoring and evaluation components were done by the researchers with assistance from the RNDs or nurse on duty. This is to determine progress and expected outcomes to ensure that nutrition problems are being addressed.
The overall outcomes of the intervention in this study are the nutritional status, quality of life, psychological distress, and level of depression of participants.
3.3. Data Collection
3.3.1. Socio-economic Status/Demographic Data
Face-to-face interviews using pre-tested structured questionnaires were done among the participants. The general family profile and selected socio-demographic data were obtained.
3.3.2. Dietary Assessment
Individual Dietary Diversity Score (IDDS) was obtained at baseline, midline, and endpoint of the study to determine the quality of food intake. A total of 16 food groups were used in the questionnaire and compressed into nine categories, based on FANTA proposition (5), as follows: (1) starchy staples; (2) dark, green leafy vegetables; (3) other vitamin a rich fruits and vegetables; (4) other fruits and vegetables; (5) organ meat; (6) meat and fish; (7) eggs; and (8) legumes, nuts and seeds; and (9) milk and its products. Overall mean dietary diversity score (DDS) was computed, and a score of less than four (4) denotes inadequate intake, while an IDDS equal to or greater than four (4) denotes adequate intake (5). Several studies mentioned IDDs as a valid measure of nutrient adequacy irrespective of the level of food intake among several population groups (6-8).
3.3.3. Anthropometric Assessment
3.3.3.1. Weight
Weight was measured using a digital weighing scale (SECA 874, Hamburg, Germany). There were at least two measurements taken, with the average recorded to the nearest 0.1 kg (9). Participants were in light clothing.
3.3.3.2. Height
Height was obtained using a stadiometer (SECA 217, Hamburg, Germany) posted against a wall. At least two measurements were obtained, and averages were computed, and recorded to the nearest 0.1 cm (9).
3.3.3.3. Body Mass Index
The weight and height measurements were used in BMI calculations. To classify participants' nutritional status, BMI is used to measure body fat using the following cut-off points: (1) underweight ≤ 18.5; (2) normal = 18.5 to 24.99; (3) overweight = 25 to 29.99; (4) obese ≥ 30.0) (9).
3.3.3.4. Waist-Hip Ratio
The waist-to-hip ratio (WHR) is a straightforward way to describe the distribution of subcutaneous and intra-abdominal adipose tissue in the body and thus, predicts the risk of developing disease conditions associated with excess abdominal fat. The WHR was obtained by dividing the waist circumference with the hip circumference.
The waist circumference was taken by measuring the perimeter around the waist or the narrowest portion of the trunk using a tape measure. Alternatively, hip circumference was taken by measuring the distance across the largest area of the hips, which is most often the broadest part of the buttocks.
For both the waist and hip circumferences, at least two measurements were taken, with averages recorded to the nearest 0.1 cm. For males, the WHR cut-off points are < 0.90 for low, 0.90 - 0.99 for borderline, and ≥ 1.0 for high. For females, the WHR cut-off points are < 0.80 for low, 0.80 - 0.84 for borderline, and ≥ 0.85 for high (9).
3.3.4. Psychological Assessment
3.3.4.1. Quality of Life
The WHOQOL-100 questionnaire intends to measure the individual’s insights within the context of their personal goals, standards, concerns, values, and culture. Consequently, the WHOQOL-BREF instrument administered in this study is a shorter version of the original instrument that may be more convenient for use in large research studies since it only has 26 items on the QoL, categorized into physical health, psychological health, social relationships, and environmental health. A higher score indicates a better QoL in the following domains (10). Domain scores produced by the WHOQOL-BREF correlate highly (0 ± 89 or above) with WHOQOL-100 domain scores (calculated on a four-domain structure).
3.3.4.2. Level of Depression
In assessing the level of depression, Beck’s Depression Inventory (BDI) questionnaire was used. It is a 21-item multiple-choice self-report questionnaire which is one of the most commonly used psychometric measures for determining severity of depression. Interpretation of scores were classified as normal if the participant obtained a total score of 1-10; mild mood disturbance (total score: 11 - 16), borderline clinical depression (total score: 17 - 20), moderate depression (total score: 21 - 30), severe depression (total score: 31 - 40), and extreme depression (total score: > 40) (11). Reliability of the BDI questionnaire, based on Cronbach alpha, ranged from 0.75 to 0.92, whereas inter-item correlations ranged from 0.53 to 0.78. The validity analysis showed that factor loadings for all items of this questionnaire ranged from 0.77 to 0.93. (12).
3.3.4.3. Psychological Distress
Psychological distress was measured using the Kessler-10 Psychological Distress Scale (K-10), which is a brief assessment of non-specific psychological distress focused on items regarding nervousness, anxiety, exhaustion, and depression. Interpretation of scores was classified as no or low psychological distress if the participant obtained a total score of 10 - 19; mild psychological distress (total score: 20 - 24); moderate psychological distress (total score: 25 - 29); and severe psychological distress (total score: 30 - 50) (13). The 2000 Collaborative Health and Well-Being Survey were used to test the reliability of the K10, and the results indicated a moderately reliable instrument. Although supplementary research on the clinical cut-off times and the scoring are needed to determine psychological distress, the K10 was identified as a simple and reliable instrument to detect mental health conditions in the population (14).
3.4. Statistical Analysis
All descriptive analyses for the socioeconomic and demographic profile, anthropometric assessment, dietary intake, level of depression, psychological distress, and QoL assessment were performed using STATA version 13.
Repeated measures analysis of variance (ANOVA) was used to determine the difference between means of anthropometric measurements, BDI, Kessler psychological distress scale, and QoL results of the participants from baseline, midline, and endpoint. However, the Mauchly test of sphericity assumption was violated, which makes the test inaccurate. To correct this, the significance level of Huynh-Feldt correction was then used if estimates of sphericity (ɛ) are > 0.75 or Greenhouse-Geisser correction if estimates of sphericity (ɛ) are < 0.75. Multiple comparisons were computed using Bonferroni.
In the assessment of the nutritional status, standard Cochran’s Q test was used for sample size > 30 and the exact version of this for small sample size < 30, after creating a dummy variable in each nutritional status. Mcnemar test was done for pairwise comparison using Bonferronnized P-value of 0.0167 to maintain a 5% probability of a type I error across the pairwise comparisons by dividing alpha (α = 0.05) to the number of comparisons (0.05/3 = 0.0167). Kendall’s Tau was also used to test the correlation between nutritional status and dietary diversity score of the participants. Repeated measures ANOVA, Cochran’s Q test, and Kendall’s tau coefficient were performed using Statistical Package for Social Sciences (SPSS) version 20.
Somer’s Delta was used to determine if there were association between DDS and the psychological parameters such as WHOQOL-BREF, BDI score, and Kessler Psychological Distress Scale. Somer’s delta, which is a measure of ordinal association between two variables, was performed using STATA version 15.
3.5. Ethical Approval
The study was conducted in compliance with the declaration of Helsinki, ethical guidelines for biomedical research involving human subjects, and the national guidelines for biomedical/behavioral research. The ethical approval was first obtained from the Department of Science and Technology Food and Nutrition Institutional Ethics Review Board (IRB) prior to study commencement (protocol code: FIERC-2018-005). In addition, signed informed consent forms were secured from the participants, and their records were kept confidential at all times.
4. Results
4.1. Socio-economic -demographic Profile of PWUDs
A total of 268 participants completed the study, mostly male (85.82%), single (34.33%), employed (88.06%), and undergraduate high school (38.81%), and belong to a nuclear type of family (61.94%) (Table 1). The mean age of the participants for both sexes is 32, and the mean household size was six. In terms of income, the participants had a mean individual income of 278.28 USD before admission in the TRC, while the mean household income is 524.24 USD (Table 2).
| Variables | No. (%) |
|---|---|
| Gender | |
| Male | 230 (85.82) |
| Female | 38 (14.18) |
| Civil status | |
| Single | 92 (34.33) |
| Married | 63 (23.51) |
| Live-in | 84 (31.34) |
| Separated/divorced/annulled/widow | 29 (10.82) |
| Education | |
| No education/some elementary | 35 (13.06) |
| Some high school | 104 (38.81) |
| Some vocational/college | 96 (35.82) |
| Vocational/college graduate | 33 (12.31) |
| Employment status (before rehabilitation) | |
| Yes | 236 (88.06) |
| No | 32 (11.94) |
| Household type | |
| Single/nuclear | 166 (61.94) |
| Extended with non-related families | 102 (38.06) |
Socio-demographic Profile of PWUDs
| Variables | Mean (SD) |
|---|---|
| Age (n = 268) | 32 (6.9) |
| Male (n = 230) | 32 (7.1) |
| Female (n = 38) | 32 (6.7) |
| Household size | 6 (3) |
| Individual income (USD) | 278.28 (377.18) |
| Household income (USD) | 524.24 (713.61) |
Mean Age, Household Size, and Income of PWUDs
4.2. Nutritional Status of PWUDs
Generally, the results showed a significant increase in the weight and BMI of the participants across the time (P = 0.000). Applying a post-hoc analysis, the results revealed that both male and female participants experienced significant increases in weight and BMI from the baseline to endpoint. On the other hand, the mean WHR of the participants did not change significantly (Table 3).
| Variables | Baseline | Midline | Endpoint | P-Value |
|---|---|---|---|---|
| Weight (kg) | ||||
| 61.11 (10.93)ME | 62.68 (10.25)BE | 63.82 (9.90)BM | 0.000* | |
| 62.13 (10.89)ME | 63.81 (10.18)BE | 65.03 (9.72)BM | 0.000* | |
| 54.92 (9.06)E | 55.83 (7.84) | 56.52 (7.66)B | 0.006* | |
| Height (cm) | ||||
| 162.83 (7.82)ME | 162.89 (7.85)BE | 162.94 (7.85)BM | 0.000* | |
| 164.34 (6.88)ME | 164.44 (6.85)BE | 164.49 (6.86)BM | 0.000* | |
| 153.70 (7.00) | 153.51 (7.02) | 153.57 (7.01) | 0.104 | |
| BMI (kg/m2) | ||||
| 22.98 (9.31)ME | 23.56 (3.01)BE | 23.98 (2.82)BM | 0.000* | |
| 22.95 (3.36)ME | 23.55 (3.07)BE | 23.99 (2.87)BM | 0.000* | |
| 23.19 (3.03)E | 23.67 (2.64) | 23.94 (2.55)B | 0.003* | |
| Waist-Hip-Ratio | ||||
| 0.9147 (0.05) | 0.9146 (0.05) | 0.9110 (0.05) | 0.160 | |
| 0.92 (0.05) | 0.92 (0.05) | 0.91 (0.05) | 0.172 | |
| 0.9032 (0.04) | 0.9079 (0.04) | 0.9005 (0.05) | 0.606 |
The majority of participants were with normal nutritional status at the baseline (76%), 4% were underweight, while 16% were overweight and obese (3%). At the end of the 120 days intervention, underweight and pre-obese classes were significantly decreased from 4.48 to 0.37%, and 23.13 to 19.78%, respectively. Using waist-hip ratio, those classified at-risk for developing serious health conditions were significantly decreased during the study period (61.6 to 58.6%), resulting in a pull of positive increase in the number of normal waist-hip ratio at endpoint (Table 4).
| Variables | Baseline | Midline | Endpoint | P-Value d |
|---|---|---|---|---|
| Nutritional status c | ||||
| Underweight | 12E (4.48) | 6 (2.24) | 1B (0.37) | 0.000 |
| Normal | 203 (75.75) | 194 (72.39) | 208 (77.61) | 0.053 |
| Pre-obese (overweight) | 44M (16.42) | 62BE (23.13) | 53M (19.78) | 0.003 |
| Obesity class I/III | 9 (3.36) | 6 (2.24) | 6 (2.24) | 0.083 |
| Waist-hip-ratio e | ||||
| Normal | 103 (38.43) | 88E (32.84) | 111M (41.42) | 0.004* |
| At risk | 165 (61.57) | 180E (67.16) | 157M (58.58) | 0.004* |
4.3. Individual Dietary Diversity of PWUDs
Analyzing the IDDS of the participants showed that more than half (61.57%) had low to medium DD (consumed ≤ 5 food groups) while about 39% had high DD (consumed ≥ 6 food groups) at the baseline. The post-intervention analysis showed a decreasing trend in the percentage of participants with low to medium DD during the study period. About 91.04% of the participants had high DD after receiving the intervention (Table 5).
| Dietary Diversity Score (total number of food groups consumed) | Baseline | Midline | Endpoint |
|---|---|---|---|
| low-medium dietary diversity (consumed ≤ 5 food groups) | 165 (61.57) | 71 (26.49) | 24 (8.96) |
| high dietary diversity (consumed ≥ 6 food groups) | 103 (38.43) | 197 (73.51) | 244 (91.04) |
Individual Dietary Diversity Score of the PWUDs a
Based on Kendall’s tau-b coefficient, there was a highly weak correlation between the nutritional status and dietary diversity score of the participants, which was not significant at the baseline (τb = 0.0672, P = 0.056) and endpoint (τb = 0.0378, P = 0.055).
4.4. Quality of Life Assessment
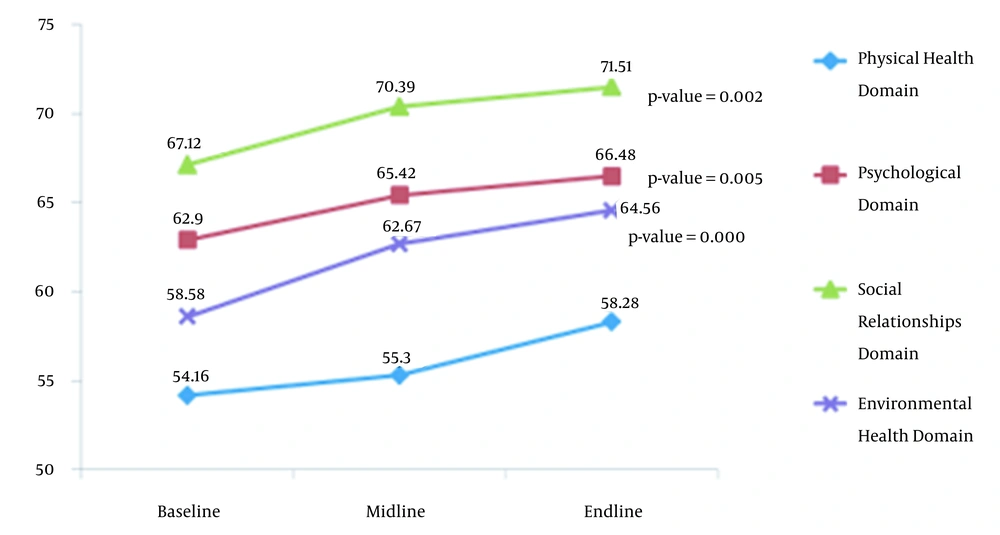
Overall, there were significant increases in the mean scores on the QoL of the participants in all domains from the baseline to endpoint: physical health from 54.16 to 58.28 (P = 0.000); psychological was 62.90 to 66.48 (P = 0.005); the social relationship was 67.12 to 71.51 (P = 0.002), and environmental health was 58.58 to 64.56 (P = 0.000). (Figure 1)
The association between WHOQOL scoring and DDS, Somers’ delta showed a highly weak to weak association between WHOQOL score in quartile and DDS categories, but non-significance was found for each domain and time points.
4.5. Level of Depression
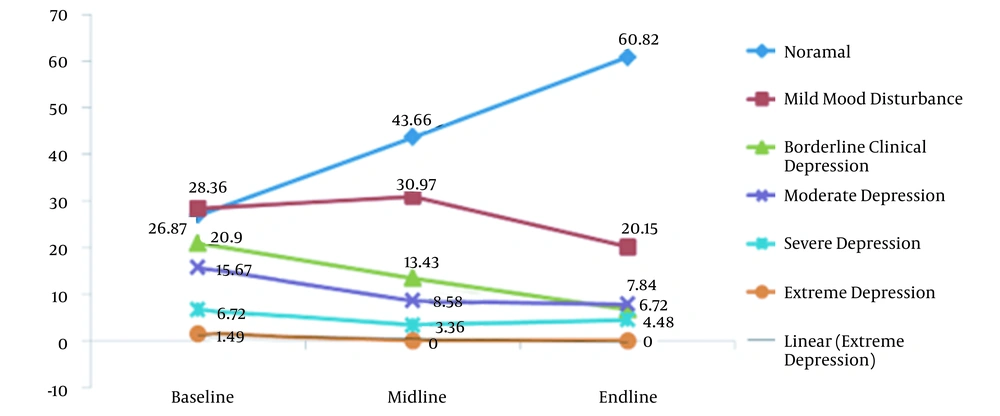
Figure 2 shows a significant decreasing trend in the mean scores of BDI scale over time. Comparing basal and endpoint values, there were increasing trends on the mean scores of normal participants (26.87 to 60.82) while a decreasing trend in the mean scores of participants who experienced mild mood disturbance (28.36 to 20.15), borderline clinical depression (20.9 to 6.72), moderate depression (15.67 to 7.84), severe depression (6.72 to 4.48), and extreme depression (1.48 to 0).
There was a very weak negative correlation between DDS and BDI categories at the baseline, and a midline and very weak positive correlation at the end line. Somers’ delta showed no statistically significant difference between periods.
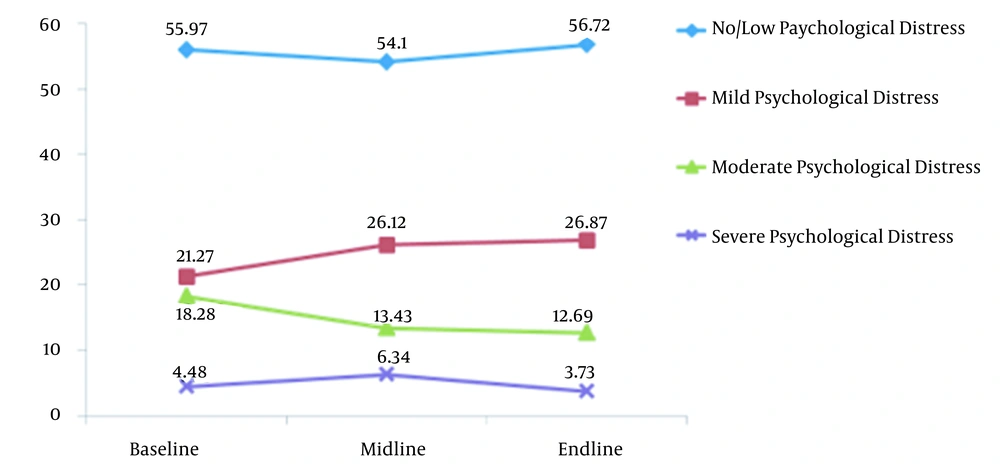
4.6. Psychological Distress
The results showed no significant changes in the mean score of the Kessler Psychological Distress Scale from the baseline to endpoint (P = 0.253). However, there was a decrease in the proportion of participants experiencing moderate (18.3 to 12.7%) to severe psychological distress (4.48 to 3.73%) (Figure 3).
The association between psychological distress and DDS showed a very weak negative correlation at the baseline to endpoint.
5. Discussion
Drug rehabilitation and treatment programs coupled with good nutrition offer an opportunity to decrease the health care burden.
The nutrition care process (NCP) is an integral part of the holistic care of PWUDs as it promotes positive patient outcomes through providing continuous and efficient individualized care for patients. This study evaluated the effects of implementing the nutrition care process as contained in the developed nutrition management guidelines for PWUDs after a 120-day implementation period.
The dietary regimen followed in the study as contained in the provided recipes was low in sugar, limited in saturated fats, low in caffeine, high in protein, and rich in antioxidants to facilitate faster healing and prevent relapse. The improved nutritional status of the participants at the end of the study might be attributed to the better quality of diet, as evidenced by the significant increase of the dietary diversity score.
Due to compromised gastrointestinal function, intravenous drugs users prefer easily ingested and digested foods. Preferences for high sugar, fatty foods, and caffeine-rich foods are common among PWUDs to perpetuate the behavioral cycle of independence. Aside from the affinity towards poor dietary quality foods, a systematic study reported that most PWUDs suffer from antioxidant vitamin deficiency. Oxidative stress is more prevalent in opium consumers since this drug causes oxidative stress and has negative effects on the lipid profile and antioxidant enzymes of PWUDs (15). Consumption of nutrient-dense foods and antioxidants was known to aid in reducing inflammation and cell oxidation and providing adequate nourishment to the body. A systematic review showed that among opium users, there was an increase in the production of free radicals and reactive oxygen species, a decrease in the concentration of vitamins A, E, C, and total antioxidant capacity, and a decrease in the activities of an enzymatic and non-enzymatic oxidant such as glutathione and glutathione peroxidase, superoxide dismutase and catalase (16). Unfortunately, there was an increase in the percentage of overweight and obesity at the end of the study. This might be attributed to the additional foods provided by family members in-between visits and their access to snacks sold in the facilities’ stores. Additional calories provided by other food items consumed by PWUDs, other than what is provided by the TRCs, can be evaluated in further studies.
At the early phase of recovery, PWUDs would often struggle to differentiate hunger from cravings for substances. Cravings are triggered by anxiety, irritability, and a low mood or energy level. Low blood sugar, dehydration, high caffeine intake, and an unbalanced diet may trigger these symptoms. Therefore, aspects that should be targeted in medical nutrition therapy and nutrition education were the healing and nourishing of the body, stabilizing mood, reducing stress, preventing cravings for substances, addressing medical conditions, and encouraging a healthful lifestyle. Based on the NMG used in the study, nutrition education is one of the interventions provided to the PWUDs other than the provision of calculated meals. It should always be taken into consideration that recovering from any substance use disorder (SUD) does not only involve changes in the diet but also gaining information and knowledge, increasing self-awareness, developing skills for sober living, and following a structured program of change. Several studies have also shown the benefits of nutrition services in the treatment outcomes when incorporated in the rehabilitation program, which includes sobriety success rate, positive behavior change, healthier food choices, decrease in BMI, and reduced waist circumference (16-19). In another study, lower levels of circulating leptin, coupled with a diet high in fat and carbohydrates, caused a metabolic imbalance among cocaine-dependent males, resulting in excessive weight gain throughout rehabilitation (20). These results only showed that incorporating positive changes in their eating environment may help facilitate dietary behavior change in rehabilitation facilities.
Concerning QoL, significant increases in the mean scores for all domains were observed at the endpoint. QoL is a significant metric and outcome in the management and treatment of chronic diseases, including SUDs (21). Given that it is a subjective assessment of a patient's life in terms of their physical health, mental health, social relationships, and environment, the patients' subjective evaluations of the effects of SUD and treatment on their lives are included. As a result, it aids physicians in recognizing issues other than the disorder's specifics, allowing them to provide more appropriate treatment. Stable mental well-being has been shown to be a powerful protective factor in the treatment of PWUDs (22). Consequently, a study among in-patients in SUD treatment showed improvement in QoL at six-month follow-up, indicating its usefulness in providing evidence of therapeutic benefit in the rehabilitation programs (23).
Psychoactive substances may lead to psychiatric problems due to the significant damage it causes to the brain’s chemistry. When the natural production of these neurotransmitters is disrupted, it compounds the PWUD’s dependence on substances due to the loss of ability to feel good naturally (24). The results indicated a significant decrease in the percentage of patients experiencing moderate to severe psychological distress from the baseline to endpoint. This indicated that along with psychological interventions, the improvements might also be attributed to proper diet and nutrient intake, providing a positive impact on mood, behavior, and proper sleep. A major basis of recovery is learning how to change negative behaviors and make healthier lifestyle changes, so making healthier food choices is a vital piece to achieve this holistic, healthy, and balanced way of life (25).
Depression, ranging from mild to major depressive disorder, may be influenced by a person's diet and vice-versa. Dietary patterns that have been identified to influence the risk of depression include processed foods, saturated fat, processed meat, refined grains, and added sugars, including sugar-sweetened beverages. Studies have shown that high consumption of natural foods such as fruits, vegetables, whole grains, legumes, nuts, seeds is inversely associated with risk of depression (26, 27). The benefits of a healthy diet in relation to depression may be attributed to factors such as improvements in vascular health, lower levels of LDL cholesterol, reduced inflammation, decrease in oxidative stress, improvements in the gut microbiome, and increased levels of serotonin and norepinephrine (28). The Beck’s Depression Inventory showed a downtrend in the mean score for both genders, indicating that a decline of depression episodes was established after 120 days of intervention. The majority of the participants experienced mild to moderate depression at the beginning of the study, which was quite expected since the participants selected were all newly admitted to the TRC (< two months). Depression is a mental illness frequently co-occurring with substance abuse, and the relationship between the two disorders is bi-directional. When the effect of drugs starts to wear off, PWUDs may experience depression as they struggle to cope with how the addiction has impacted their life (29). Among the study participants, there was a decrease in the prevalence of individuals experiencing depression from the baseline to the endpoint. Many of the usual eating habits that occur during addiction are similar to those that occur in depression, which may include poor appetite, skipping meals, and a strong craving for sweets (4). A meta-analysis study showed that a dietary pattern characterized by high intakes of fruit, vegetables, whole grain, fish, olive oil, low-fat dairy, and antioxidants with low intakes of animal foods was apparently associated with a decreased risk of depression. A diet rich in red and/or processed meat, refined grains, sweets, high-fat dairy products, butter, potatoes, and saturated fats, and low in fruits and vegetables, on the other hand, is linked to an increased risk of depression (30). This only shows that eating healthy alongside the rehabilitation and treatment program may decrease the risk of depression and aid in faster recovery.
After testing for the association, however, no association was observed between dietary diversity score and the three psychological parameters (WHOQOL-BREF, K10, and BDI). Despite the significant improvements of scores from the baseline to endpoint and positive association seen in previous literature, it should be taken into account that only DDS was obtained instead of the usual nutrient intake of the PWUDs, and the intervention was only conducted for 120 days, instead of the whole rehabilitation period. With these limitations, it is strongly recommended for future studies to use a more quantitative approach of assessing dietary intake and consider a longer period of intervention to best see the results.
Aside from providing the intervention, another important component of the nutrition care process is the monitoring and evaluation of the researchers with the help of the resident health workers in the TRCs. These are important components of the NCP because they are used to assess and evaluate the nutrition intervention and if the nutrition-related targets have been reached. In general, it was observed in the nutrition monitoring and evaluation that the intervention coupled with the rehabilitation regimen, was successful in the improvement of the nutritional status of PWUDs, which was reflected with the increased proportion of PWUDs with normal BMI. Lowered mean scores in depression and psychological distress, as well as improved, QoL were also observed from the baseline to midline to endpoint. However, it is worth noting that although the NMG and recipe booklets were well-adapted, the initiative of the TRC management is still a determining factor in the successful implementation of the intervention.
5.1. Conclusion
Nutrition services employing the nutrition care process and the developed calculated diet for PWUDs could be implemented in the TRCs. The interventions resulted in improved nutritional status, quality of life, and reduced stress levels of PWUDs.
5.2. Study Limitations
The investigators have no complete control over the participant’s diet aside from the calculated meals provided by the TRCs, thus, it is possible for participants to consume other food items that could affect their nutrient intake. Also, due to limited budget, the biochemical assessment was not performed to detect the presence of nutrient deficiencies and the intervention period was only 120 days. As for the dietary assessment, only DDS was obtained instead of the usual nutrient intake of the PWUDs.