Dear Editor,
The suicide rate among physicians has been reported to be higher than that among the public as a whole (1). Several factors, including the knowledge of the lethal doses of medications, increased access to potentially lethal medications, and untreated or inadequately treated mental illnesses (eg, depression and anxiety), increased the rates of suicide completion among physicians (2). This increased rate is often associated with long working hours, the high-stress culture of medicine, the relative neglect of self-care, and spending less time with family and friends (3).
Medical students and physicians in residency programs appear to be at higher risk of burnout, depression, and substance abuse (4). A meta-analysis reported that there is an increase of 15.8% in depressive symptoms in the first year of residency. Over the course of training, 20.9 - 43.2% of residents showed depressive symptoms. Rotenstein et al. reported that the prevalence of suicidal ideation among medical students was 11.1% (5).
Medical literature suggests that the enhanced rate of suicide during and after a stressful environment due to pandemics is not unusual (6, 7). Jahan et al. reported about coronavirus disease 2019 (COVID‐19)‐related suicides among healthcare professionals the most common reason for which was infection with COVID‐19, followed by a stressful and heavy workload, the fear of COVID‐19 infection, anxiety related to the transmission of the virus and mortality of patients, and increased emotional stress (8). Although several publications anticipated having higher healthcare providers’ suicidality due to the COVID-19 pandemic, there is no systematic information on residents’ and physicians’ suicides due to the current pandemic (9, 10).
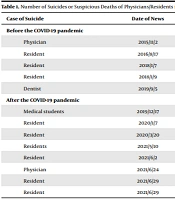
The present study was carried out in June 2021. This study reviewed Iranian news websites addressing the suicide of Iranian resident physicians observed through the use of the Google search engines by searching Persian equivalences of key terms (eg, suicide, physician, resident, and medical student). The results showed that Iranian news agencies reported that the number of suicides among physicians/residents was 15 from 2019 to June 2021. Detailed results are presented in Table 1.
| Case of Suicide | Date of News | N | City | Link of News |
|---|---|---|---|---|
| Before the COVID-19 pandemic | ||||
| Physician | 2015/11/2 | 1 | Tehran | https://www.jamaran.news/ |
| Resident | 2016/8/17 | 1 | Tehran | https://sepidonline.ir/index.php?newsid=8660 |
| Resident | 2018/1/7 | 1 | Sari | https://khabarfarsi.com/u/49979680 |
| Resident | 2018/1/9 | 1 | Sari | http://shafaonline.ir/fa/news/180895/ |
| Dentist | 2019/9/5 | 1 | Tehran | https://www.rokna.net/ |
| After the COVID-19 pandemic | ||||
| Medical students | 2019/12/17 | 5 | Ahvaz | https://www.khabaronline.ir/news/1332245/ |
| Resident | 2020/1/7 | 1 | Tehran | https://www.isna.ir/news/98101713509/ |
| Resident | 2020/3/20 | 1 | Kerman | http://www.tabnakkerman.ir/fa/news/832738/ |
| Residents | 2021/5/10 | 4 | Tehran | https://www.isna.ir/news/1400021913171 |
| Resident | 2021/6/2 | 1 | Mashhad | https://www.salamatnews.com/news/312420/ |
| Physician | 2021/6/24 | 1 | Nahavand | https://www.salameno.com/news/55264571/ |
| Resident | 2021/6/29 | 1 | Shahrekord | https://www.salamatnews.com/news/313901/ |
| Resident | 2021/6/29 | 1 | Kashan | https://www.salamatnews.com/news/313901/ |
Abbreviation: COVID-19, coronavirus disease 2019.
In numerous countries, suicide is a silent epidemic due to the culture of silence. Exposure to public suicide-related information could make others start thinking about self-harm, suicidal thoughts, and suicidal plans (11). On the other hand, suicide issues remain poorly understood in resident physicians, and their problems are mostly neglected. According to the report of the Iranian Students News Agency from Iran’s Medical Organization spokesman, work pressure, particularly in the COVID-19 pandemic, and economic pressure are the problems faced by medical students and residents (12).
In Iran, economic pressure has been increased in recent years, with negative impacts on mental and physical health, thereby threatening the life of Iranians (13). The reinforcement of protective factors for suicide, including access to health care, experience in conflict resolution, support of family and community, and religious beliefs, should be addressed. The mental health of residents and timely screening should be considered before they attempt suicide.