1. Background
Pregnancy, childbirth, and motherhood are among the most important events in women’s lives (1). However, many women experience some degrees of mood disorders after delivery (2), such as baby blues and postpartum depression (PPD), as the most common mood disorders after childbirth (3, 4). Postpartum depression is a common form of depression that begins during the first four weeks after delivery, with a prevalence rate of 10 - 15%, 33%, and 45% in routine pregnancies, unwanted childbearing, and in mothers with a history of depression, respectively (4-6).
Although the exact causes of this disorder are still unclear, some studies have shown an association between PPD and the chemical, physical, and social changes associated with childbearing. Postpartum depression presents with various symptoms, such as memory and concentration impairment, fatigue, insomnia, changes in appetite, feelings of guilt, self-harm behaviors, discomfort, anhedonia, and psychomotor retardation (7). One of the main concerns of parents with a mood disorder is their inability to perform their responsibilities, including parental roles, child feeding, and communication with the child. On the other hand, it has been shown that PPD can significantly affect neonatal weight gain (8, 9).
Postpartum depression treatments are classified into two categories: Medical therapy and psychotherapy. There is a slight interest in prescribing medication to treat depression during pregnancy and lactation. On the other hand, due to fear of the side effects of medications, patients are less likely to take medication during pregnancy and lactation (10-13). Among different psychotherapy methods, cognitive-behavioral therapy (CBT) is one of the most effective therapies for PPD (14-17). Cognitive-behavioral therapy is a psycho-social intervention to improve mental health. Cognitive-behavioral therapy focuses on challenging and changing unhelpful cognitive distortions and behaviors, improving emotional regulation, and developing personal coping strategies that target solving current problems. The therapeutic effect of CBT on the management of depression is greater than that of medical therapy; indeed, it is an effective short-term intervention. However, one of its important limitations is the need for the patient’s physical presence in several consecutive sessions to complete the course, which is often difficult for recently delivered mothers (18-20).
2. Objectives
We tried to address this limitation using a new method by providing CBT as virtual content for mothers. We evaluated this new method’s effectiveness in treating PPD compared to drug therapy.
3. Materials and Methods
This open-label randomized clinical trial was performed from 2019 to 2020. Random sampling was conducted among the mothers who had just given birth and met the criteria for the study. They were randomly assigned to two groups using the method of randomized blocks with sealed envelopes. The weighing person did not know about group assignments. Postpartum depression was evaluated using the Edinburgh Postpartum Depression Questionnaire, which includes 10 questions. The total score is 30, and scores higher than 10 indicate postpartum depression. The researchers have reported the validity of the Persian version of the scale test is 0.8 and Cronbach’s alpha of 0.77, with a sensitivity of 95.3% and specificity of 87.9% (21).
Considering the significance of a 200 g difference between the mean weight changes and the standard deviation of 300 grams in each group, with the test power of 90% and the type 1 error probability of 5%, based on the following formula, 48 cases were needed in each group. Considering the 10% dropout rate, we included 55 people in each study group.
The inclusion criteria were singleton pregnancies, the Edinburgh questionnaire score of more than nine, and being able to utilize social media applications like Telegram. Also, multi-gravid women and those with complicated conditions, such as hypertensive disorder of pregnancy, diabetes, and delivery bleeding, were excluded from the study. In total, 1,034 women completed the Edinburgh questionnaire, and only 129 had a score of more than nine (10 or more) and filled out the informed consent form. Nine patients were excluded due to no access to social media applied in this study. Fourteen women were excluded due to pregnancy complications, i.e., preeclampsia and diabetes. In addition, four other cases were excluded due to multiple birth, stillbirth, neonatal death, and prior depression. Finally, 102 cases were randomly divided into two groups, including 52 in ICBT and 55 in drug therapy groups.
In this study, the Declaration of Helsinki was respected throughout the study. Also, this study was approved by the Ethics Committee of the Tehran University of Medical Sciences (IRB code: 9421744011). Baseline data, including age, pregnancy weight gain, body mass index (BMI), and infant’s birth weight, sex, and feeding data, were recorded. The subjects were randomly assigned to receive either medical treatment (sertraline 50 mg/day) or ICBT (cognitive behavioral therapy including depression symptoms, controlling anxiety and depression, coping strategies, the role of negative thoughts and their relationships with emotions, problem-solving skills, monitoring mood and improving depressed mood, relaxation training, and teaching effective behavioral styles). Virtual content was sent via text messages through Telegram.
The facilitator visited all patients in person three times during the study period. The first meeting was to explain the plan and the type of treatment. The second visit was performed when the baby was two months old, and the third was done at four months old. The purpose of the second and third visits was to find the cases of exacerbation or suicidal thoughts. So, if the patient suffered from those problems, she could no longer participate in this study; however, there were no such cases. If people had a problem with the treatment, it would be considered. During this period, telephone counseling was available to patients five days a week, and they could call in case of any problem. In the follow-up, the weight of infants in both groups was assessed by a calibrated Seca scale at the age of two and four months, and the mothers completed the Edinburgh questionnaire.
Statistical analyses were accomplished by SPSS version 24.0 (Chicago, Illinois, United States). Depression status and infants’ weight at different time points were analyzed using repeated-measures ANOVA and independent-sample t test. The p-values of less than 0.05 were considered statistically significant. All numerical data are represented as mean ± standard deviation (SD).
4. Results
There were 29 (55.8%) male children in the group of cognitive behavioral therapy with virtual content and 26 (52%) male children in the drug treatment group. The mean maternal age in the ICBT and conventional groups was 28.51 ± 4.96 and 29.12 ± 5.76 years, respectively (P > 0.05). The mean pregnancy weight gains in the ICBT and conventional treatment groups were 13.63 ± 4.24 (range: 8 to 25) and 13.48 ± 3.99 kg (range: 8 to 24), respectively (P = 0.041). In Table 1, the characteristics of the patients were mentioned.
| Group | Age | Mothers' Weight Gain in Pregnancy | ||
|---|---|---|---|---|
| Mean ± SD | n | Mean ± SD | n | |
| Cognitive behavioral therapy | 28.519 ± 4.960 | 52 | 13.634 ± 4.247 | 52 |
| Drug therapy | 29.120 ± 5.766 | 50 | 13.480 ± 3.996 | 50 |
| Total | 28.813 ± 5.352 | 102 | 13.558 ± 4.106 | 102 |
Characteristics of the Patients
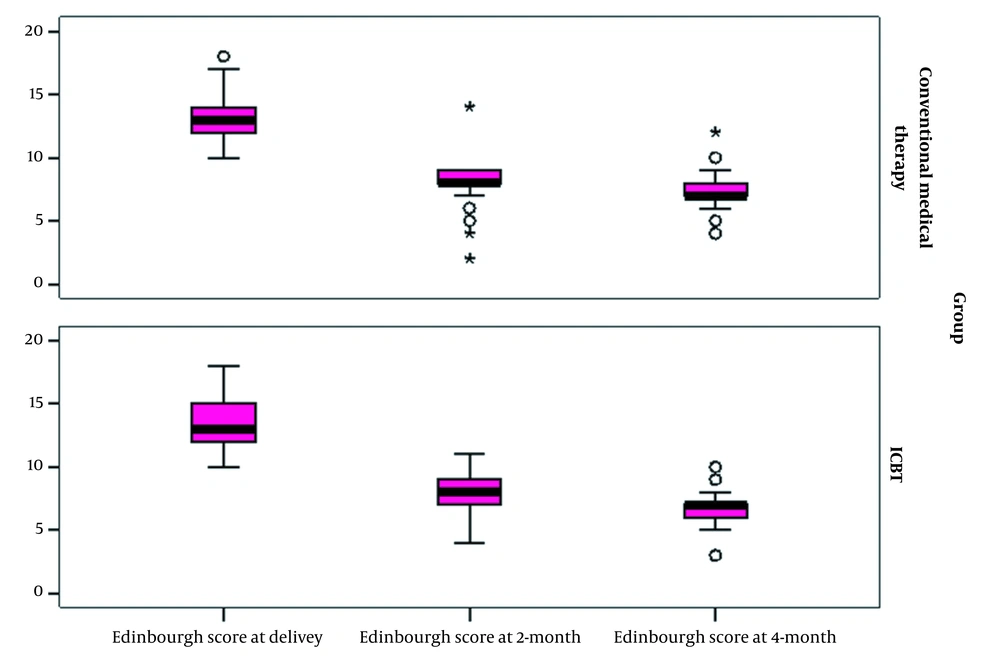
As shown in Figure 1, the mean Edinburgh’s depression scale score at birth was 13.26 ± 2.12 and 13.3 ± 2.05 in the ICBT and conventional groups, respectively (P > 0.05). The mean score two months after delivery was 7.90 ± 1.16 and 7.94 ± 2.19 in the ICBT and conventional groups, respectively (P > 0.05). Also, the mean score four months after delivery was 6.82 ± 1.28 and 6.98 ± 1.49 in the ICBT and conventional groups, respectively (P > 0.05).
Covariance analysis (ANCOVA) was used to compare the average weight changes of the two groups. The confounding effect of children’s gender and nutrition type was considered in the ANCOVA model.
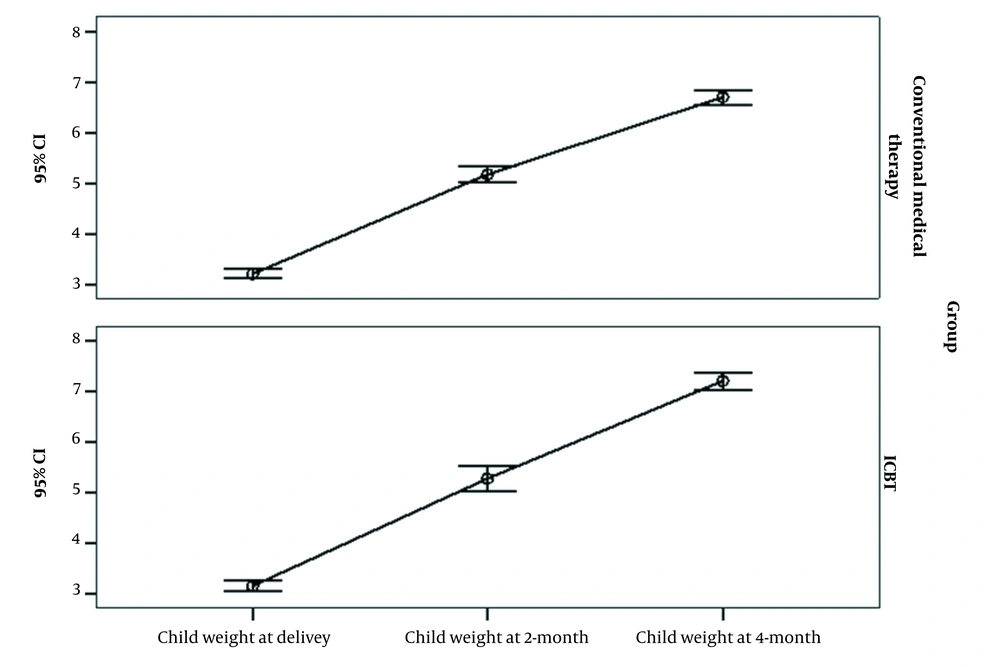
As shown in Figure 2, the mean infants’ birth weight was 3.15 ± 0.37 and 3.20 ± 0.33 kg in the ICBT and conventional groups, respectively (P > 0.05). Their weight after two months was 5.27 ± 0.89 and 5.17 ± 0.57 kg in the ICBT and conventional groups, respectively (P > 0.05). Also, the infants’ weight after four months was 7.2 ± 0.60 and 6.69 ± 0.51 kg in the ICBT and conventional groups, respectively (P < 0.001).
According to repeated-measures ANOVA, the groups showed no significant difference in Edinburgh’s depression scale score (P > 0.05). However, the infants’ weight showed a significant difference between the groups (P = 0.041), and the ICBT group showed better weight gain than the group receiving conventional medical treatment.
5. Discussion
This study assessed the effectiveness of ICBT versus conventional medical therapy for PPD. It was observed that ICBT could improve PPD and weight gain after four months of treatment compared to conventional therapy and improved weight gain in children. Numerous studies have reported that PPD could harm maternal and infant well-being. Although PPD is a prevalent disorder, less than 50% of cases seek treatment, and only less than 10% of women who suffer from PPD receive adequate treatment (22, 23). Some interventions using the Internet or phone call could significantly decrease essential barriers, such as difficulty attending a clinic with an infant for their treatment, and enable them to control their treatment schedule (24).
On the other hand, it has been shown that CBT based on virtual content could significantly improve depression in PPD. In this regard, Milgrom et al. in 2015 investigated the effect of online CBT on postnatal depression. They observed that online CBT with a follow-up could significantly improve postnatal depression (24). In addition, a study by Milgrom et al. was conducted to compare the effect of three treatments, including CBT, selective serotonin reuptake inhibitor (SSRI) therapy including sertraline, and combination therapy of both CBT and SSRI on PPD (17). The results suggested that these treatments could significantly improve PPD; however, BT was more effective, followed by combination therapy. Yazdanimehr et al. conducted a study to investigate CBT’s effectiveness in treating PPD (15). The results revealed that depression could be improved by receiving CBT in individuals with PPD compared to routine treatments (15). In line with the above-mentioned studies, we observed that CBT could significantly improve the Edinburgh postnatal depression scale score after four months from 13.269 to 6.538. Accordingly, CBT could be a novel treatment for PPD in women.
It has been shown that PPD adversely affects the mother’s quality of life and the infant’s well-being and weight gain. Postnatal depression negatively impacts mothers, manifesting in a low quality of life and the inability to care for themselves, their partners, and infants (25, 26). Zubaran et al. showed a significant relationship between PPD and well-being (27). Johansson et al. showed that internet cognitive behavior therapy had a good result in reducing depression compared to routine treatment after six and 12 months (28). Another study showed reduced symptoms of depression with internet-delivered cognitive behavioral therapy compared to people on the waiting list (29). Loughnan et al. and Mailgram et al. showed that internet CBT+ coach calls for PND (MumMoodBooster (MMB)) improved the symptoms of depression compared to usual treatment and face-to-face CBT within 21 weeks (24, 30).
However, few studies have been conducted to evaluate the effect of CBT on PPD and infants’ well-being and weight gain. In this regard, we investigated the infant’s weight gain and the mothers’ PPD status. Our results failed to show any significant difference between the cases treated conventionally and those treated with CBT two months after treatment. These results suggest that both treatments could have the same effect on child weight gain. However, after four months of CBT, the results showed a significant difference between the groups in weight gain. Mothers treated with CBT were found in children with a significantly higher weight gain than those on routine treatment.
The small size of this randomized clinical trial (leading to low power) and the short length of follow-up could be considered our limitations. In this regard, studies with larger sample sizes and longer follow-ups are suggested to demonstrate the effectiveness of CBT in PPD and child weight gain.
5.1. Conclusions
In conclusion, this study showed that CBT based on virtual content was effective for women with PPD and their children. Hence, CBT may be considered a novel treatment for PPD compared to conventional medical treatment.