1. Background
Drug addiction and substance abuse are some of the most critical problems of the present age that have spread worldwide, and the number of victims of drug use is increasing every day (1). The United Nations Office on Drugs and Crime (UNODC) announced in its 2012 report that almost 16.5 million people worldwide are illicit users of opioids (2). Afghanistan, the world's largest producer of opium poppy, is adjacent to the Persian Gulf countries, including Iran. Thus, the region has the largest market and consumers of illicit opioids globally (3). Methadone maintenance treatment (MMT) is one of the essential treatments based on scientifically substantiated evidence of opioid dependence (4). Methadone is effective in substance abuse treatment by blocking opioid receptors, preventing withdrawal symptoms, and reducing cravings (5). Also, previous studies have shown the positive consequences of MMT, including reducing the frequency of criminal behavior (6), mortality (7), HIV transmission (8), and improving employment status (9).
Sexual dysfunction (SD) is expected as a potential side effect of opioid substitute treatment (10, 11). Opioid suppressive effects on the hypothalamus-pituitary-gonadal axis are among the mechanisms proven in animal studies to develop sexual dysfunction in patients on MMT (12). Several human studies have shown the association between hypogonadism and sexual dysfunction in opioid patients (13). Sexual dysfunctions, such as erectile dysfunction (ED), ejaculatory disturbances, and loss of sexual desire, are often reported in a significant number of male patients on MMT (14). The prevalence of sexual dysfunction among this population varies from study to study, and its exact prevalence is yet to be determined (15). Previous studies found that sexual dysfunction is higher in MMT patients than in the general population (30% to 100%) (16).
Previous studies have shown that many MMT users are experiencing psychological problems, such as depression and anxiety (17, 18). Depression is strongly linked to male sexual dysfunction. The association between depression and ED is likely bidirectional, so that depressed affect may cause ED by impairing sexual arousal (19), while decreased sexual activity and dissatisfaction with one's sexual life can initiate depressive symptoms (20, 21). The third factor, substance abuse, may cause both of them (22). The presence of depressive symptoms is commonly linked with ED, even in the absence of a syndromal depression (23, 24). Depression is also associated with premature ejaculation (PE) (25). Various anxiety disorders, such as panic disorder and generalized anxiety disorder, are also associated with ED and social phobia with PE (26-28).
Child sexual abuse (CSA) is significantly associated with sexual dysfunction in adulthood (29). A study showed a significant association between CSA and sexual dysfunction, even after controlling for depression (30). Extensive research has been conducted on the association between CSA and sexual dysfunction in women, while less attention has been paid to the role of CSA in male sexual dysfunction (31).
Sexual dysfunction is one of the issues that must be carefully identified and addressed by adequate measures. Failure to address this vital issue (due to the particular taboo in society) may lead to social and personal harm and the gradual and hidden decline of health in patients on MMT. The main emphasis currently is on recognizing these abnormalities from a medical and physiological point of view, and less attention is paid to the role of psychological factors in explaining these cases. This is especially evident in the country due to special cultural issues, lack of necessary tools, particular sampling problems, and, most importantly, lack of experts in this field.
2. Objectives
This study aimed to determine the prevalence of sexual dysfunction in men on MMT and the role of psychological factors, including anxiety, depression, and childhood trauma, on the sexual function of MMT patients.
3. Patients and Methods
3.1. Participants and Procedure
The current study was conducted in 2020. The participants included 100 MMT patients selected from the MMT clinic of Baharan Psychiatric Hospital, Zahedan, Iran. They completed self-report standard questionnaires, including Beck Depression Inventory-II (BDI-II), Beck Anxiety Inventory (BAI), Childhood Trauma Questionnaire (CTQ), and International Index of Erectile Function (IIEF-15). Informed consent was taken from all patients, and they were assured that their information would remain confidential. The Ethics Committee of Zahedan University of Medical Sciences (ZAUMS) approved the study design and procedures.
Married men aged 20 - 40 years undergoing MMT services for at least one month and with a literacy of six years or above were eligible to participate in the study. Those who were diagnosed with chronic psychiatric disorders (schizophrenia, bipolar disorder, and major depression), hormonal problems, genital anatomical disorders, arteriopathy, neurological and metabolic problems such as diabetes, those with a history of sexual dysfunction before addiction, and those using substances other than methadone were excluded from the study.
3.2. Measurements
The assessment tool gathered demographic characteristics, methadone treatment status (duration of MMT and methadone dose), and drug use details (such as the history of drug use).
The BDI-II is a self-report questionnaire consisting of 21 items measuring the severity of depressive symptoms. This scale is scored on a four-point Likert scale from 0 to 3. Scores range from 0 to 63. The severity of depressive symptoms is divided into four categories: no or minimal depression (scores 0 to 13), mild depression (scores 14 to 19), moderate depression (scores 20 to 28), and severe depression (scores above 29) (32). The validity of the BDI-II Persian version was 0.73, and its reliability was 0.91 (Cronbach's α = 0.87) (33)
The BAI is a self-report questionnaire consisting of 21 items measuring anxiety symptoms. This scale is scored on a four-point Likert scale from 0 to 3. The anxiety levels include low anxiety (scores 0 to 21), moderate anxiety (scores 22 to 35), and severe anxiety (scores above 36) (34). The validity of the BAI Persian version was 0.83, and its reliability was 0.72 (Cronbach's α = 0.92) (35).
The Childhood Trauma Questionnaire (CTQ) is a 28-item self-report questionnaire designed to measure physical, sexual, and emotional abuse and physical and emotional neglect. Each item is rated on a five-point Likert-type scale (never = 1 to always = 5). The scores range from 5 to 25 for each subscale and 25 to 125 for the whole questionnaire (36). In Iran, Cronbach's alpha for the short form of the test has been estimated from 0.81 to 0.98 (37).
The IIEF is a reliable and multidimensional scale for assessing sexual function in men in both research and clinical trials (38). This index has 15 items that evaluate five areas of male sexual function: erectile function (6 items), orgasmic function (2 items), sexual desire (2 items), intercourse satisfaction (3 items), and overall satisfaction (2 items). The maximum scores for the sexual function subscales are as follows: 30 scores for erectile function, 10 scores for orgasm performance, 10 scores for sexual desire, 15 scores for sexual satisfaction, and 10 scores for overall satisfaction. Higher scores indicate lower sexual dysfunction. Based on the score that the person gets on this questionnaire, sexual dysfunction is divided into five categories: severe (scores below 11), moderate (scores between 11 and 16), mild to moderate (scores between 17 and 21), mild (scores between 22 and 25), and no sexual dysfunction (scores between 26 and 30) (39). The divergent validity of the IIEF Persian version was 0.74 based on Spearman's rank correlation, and its test-retest reliability was 0.95 (40).
3.3. Statistical Analysis
Bivariate correlation analyses and stepwise regression models in SPSS version 24 software were employed to determine the predictors of sexual function in MMT patients (the total scores of the IIEF were used as the dependent variable). The study reported 95% confidence intervals (CIs) and considered p values less than 0.05 as statistically significant.
4. Results
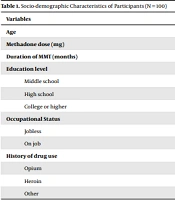
A total of 100 men were included in this study. The mean age of the participants was 32.72 ± 5.49 years (20 - 40 years). Methadone's mean dosage was 15.70 ± 4.08 mg (range 5 - 30 mg), and the mean duration of MMT was 40.23 ± 30.23 months (range 2 - 120 months). The other socio-demographic data and types of substance use before MMT are shown in Table 1.
| Variables | Values a |
|---|---|
| Age | 32.72 ± 5.49 |
| Methadone dose (mg) | 15.70 ± 4.08 |
| Duration of MMT (months) | 40.23 ± 30.23 |
| Education level | |
| Middle school | 47 (47) |
| High school | 39 (39) |
| College or higher | 14 (14) |
| Occupational Status | |
| Jobless | 23 (23) |
| On job | 77 (77) |
| History of drug use | |
| Opium | 49 (49) |
| Heroin | 10 (10) |
| Other | 41 (41) |
Socio-demographic Characteristics of Participants (N = 100)
There were 17 (17%) patients who had various levels of sexual dysfunction, including mild (n = 1, 1%), mild-moderate (n = 2, 2%), moderate (n = 5, 5%), and severe (n = 9, 9%). The mean and standard deviation of sexual function scores are presented in Table 2.
| Variables | Range | Mean ± SD |
|---|---|---|
| Sexual desire | 1 - 10 | 5.26 ± 2.10 |
| Erectile function | 1 - 30 | 15.17 ± 6.57 |
| Orgasm satisfaction | 1 - 10 | 5.19 ± 2.63 |
| Intercourse satisfaction | 1 - 15 | 7.42 ± 3.73 |
| Overall satisfaction | 1 - 10 | 6.12 ± 2.30 |
| Total score | 5 - 75 | 39.16 ± 15.63 |
Sexual Function of Participants (N = 100)
According to the bivariate correlation analysis, higher depression and child sexual abuse significantly reduced sexual function, while anxiety and childhood trauma subscales, except for sexual abuse, had no significant association with sexual function. Also, there was no significant association between methadone dose and MMT duration and sexual function. Table 3 shows the result of the correlation analysis.
Results of Bivariate Correlation Analysis
The stepwise linear regression model was used to determine the predictors of sexual function. Methadone dose, MMT duration, depression, anxiety, and childhood trauma subscales were considered the independent variables. Methadone dose, MMT duration, anxiety, physical and emotional abuse, and physical and emotional neglect were omitted from the model. Depression predicted sexual dysfunction in men on MMT. In the second step, where child sexual abuse and depression were considered the independent variables, sexual abuse could predict sexual dysfunction along with depression. Child sexual abuse and depression could predict 12% of the variance in sexual function (F = 6.61; P < 0.002). The results are shown in Table 4.
Results of Stepwise Regression Model of Predictors of Sexual Function
5. Discussion
Although some research has been conducted on the prevalence of psychological problems and sexual dysfunction separately in substance abuse patients, most of these studies have examined the effects of substance abuse on sexual dysfunction. However, based on a literature review, we did not find a comprehensive research has been done on the association between these patients' psychological problems and their sexual dysfunction. Therefore, this study investigated the association of depression, anxiety, and childhood trauma with sexual dysfunction in MMT patients. The results of this study on the prevalence of sexual dysfunction in substance abuse patients are contrary to the popular belief that substance abuse improves sexual function and is in line with the scientific findings that sexual dysfunction is prevalent among substance abusers (41, 42) The other result of this study, the prevalence of sexual dysfunction in patients receiving methadone treatment, was not in line with the results of some previous studies, and the epidemiological results showed that the prevalence was lower in this study than in previous studies (16, 43, 44). This mismatch can be attributed to several reasons. The first one may be the sample type because previous studies used patients with a wide age range whose average age was more than the sample in the present study. The prevalence of sexual dysfunction was lower in this study than in previous studies because the rate of sexual dysfunction increases with age. The second reason for this discrepancy may be the type of methodology because studies that used interviews reported higher rates of sexual perversion than studies that used questionnaires. The third reason may be the type of drug because studies have shown that sexual dysfunction is much higher in methadone-treated patients who have used heroin than in other opioid-derived drug users (44). In this study, a small number of people had a history of heroin use before treatment. Another finding of this study was that depression and child sexual abuse were associated with sexual dysfunction, significantly predicting 12% of sexual dysfunction.
The results of this study on the prediction of sexual dysfunction in adulthood based on sexual abuse in childhood are consistent with the results of previous research (45). Researchers believe that when explaining sexual dysfunction in people with a history of child sexual abuse, it is better to look at it from the perspective of a traumatic experience. People who have been sexually abused as children and suffer from distressing symptoms may have experienced various aspects of sexual intercourse, such as touching, nudity, flirting, genital and oral stimulation, and any penetration. It may be considered stimuli reminiscent of childhood sexual trauma (46-48). Experiencing dissociative symptoms or flashbacks related to child sexual abuse can lead to sinful or embarrassing responses about sex and feelings of disgust during sexual intercourse (49, 50). Thus, these people experience re-experiences and flashbacks of childhood trauma during sexual intercourse, interfering with their normal sexual intercourse (51-53).
Depression was another component associated with sexual dysfunction in this study. Research has shown that men with depressive symptoms lose nocturnal penile tumescence (NPT), suggesting that depression can lead to neurophysiological defects in arousal and congestion of the arteries of the genitals, resulting in decreased sexual desire (54). The results also showed that decreased sexual desire is the most common type of sexual dysfunction among depressed people, which can be due to anhedonia, the main symptom of depression (55).
Despite the above findings, this study has some limitations that should be considered in generalizing the findings. First, this study was performed on men, so caution should be exercised in generalizing the results to women. Second, as this study's main aim was to control the effect of variables such as age, in the initial screening, when the sample size was 350 people, the sample was reduced to 100 people. Third, this study only used questionnaires to measure research variables and neglected other data collection tools, such as biological and objective tools. Fourth, due to the study's cross-sectional nature, it was not possible to assess the temporal relationship of variables in the present study. Finally, in this study, depression and child sexual abuse could explain only 12% of the variance in sexual dysfunction, and the rest was ambiguous. Given the limitations mentioned, it is suggested that future studies consider female populations and accurate and broader tools.
5.1. Conclusions
Since people on MMT suffer from psychological problems that can be risk factors for sexual dysfunction, identifying risk factors can help health staff take action to prevent sexual dysfunction. It is also crucial to develop effective sexual dysfunction prevention programs in treatment protocols. Comprehensive sexual dysfunction prevention efforts necessitate conducting more research on protective and risk factors and developing appropriate prevention strategies to increase the mental health of MMT patients.