1. Context
Suicide is one of the major concerns of public health and a leading cause of death worldwide (1, 2). The World Health Organization estimates that 703,000 people die annually from suicide. Suicide accounted for 1.3% of deaths in 2019, with the highest suicide rates (per 100,000 people) in Africa, Europe, Southeast Asia, and the United States (3). A suicide attempt is a matter of immediate public health. Statistics in the United States showed that 1.4 million suicides were committed in 2018 (4). For each suicide-related death, there are approximately 25 suicide attempts (5). Suicide brings shame and disgrace to the survivors (6). It also results in economic costs to individuals, families, and society (7). Social stigma towards suicidal behaviors is pervasive, and socio-culturally, people with a history of suicide are considered impulsive, selfish, weak, and attention-seeking (8). However, "don’t stigmatize patients" is one of the most common recommendations of mental health professionals for clients with a history of suicide (9). However, negative beliefs about suicide survivors can cause distress for them, creating social isolation, reducing supportive behaviors, and increasing the risks of future suicidal behaviors (6). The whole idea of suicide is also essential (10), and thoughts of suicide indicate a high degree of psychological distress (11). Passive suicidal ideation is significantly associated with psychiatric illness and suicide attempts (12).
Moreover, suicide is a relatively specific endpoint (13) in which a vulnerable person is motivated to engage in a behavior destined to die (regardless of whether the behavior leads to harm or not (14). Numerous factors leading to suicide make its prediction difficult. It generally involves psychological, social, cultural, economic, medical, or situational factors. Because of its vital outcomes, predicting suicide is a critical challenge for clinical specialists. A clinical specialist can use various resources to collect data, including clinical interviews, patient history, current patient status, and projective tests to assess emotional and personal dynamism. Based on Sigmund Freud's theory and its unconscious importance, the projection tests attempt to assess the invisible part of the human personality (15). The Rorschach test is the most common in the clinical field among the projection tests. Although it is said that projective tests such as Rorschach can assist in the early detection of suicide behaviors, the use of the Rorschach test for suicide evaluation was reduced due to the development of cognitive-behavioral psychology in the 80s. Criticism is more related to (1) Rorschach is immensely theory-oriented, (2) extremely time-consuming, and (3) it is a subjective test. The majority of psychologists seek faster and more objective assessment methods. Thus, they emphasize the self-report criteria regarding personality assessment, such as the Minnesota multiphasic personality inventory (MMPI). Even though the self-report measures might be more statistically valid, they may sometimes be unable to demonstrate the richness and depth of the individual personality traits (16).
Rorschach test is still an important tool in clinical assessment (17-19), and since suicidal ideation is regarded as a severe threat to an individual’s life, it will be pretty beneficial if Rorschach can help identify the suicidal ideation. Rorschach’s researchers have followed several approaches in the assessment of suicide. Single-sign approach, multiple-sign approach, and suicide constellation approach. The first study regarding a single suicide-related symptom concentrated on content. Several researchers argued that the pathological content could be regarded as a potential sign of suicidal ideation (20-22). The pathological content comprises the contents of death, dying, mental breakdown, and being lost. Despite Hertz, Fleischer reported that merely one pathological response could be considered to indicate the possibility of suicide (23). Exner found that when three or more responses with pathological content are added to the criteria of the suicide system, it increases the chance of identifying a group of suicidal ideation from 74% up to nearly 80%. More signs indicate an increased risk of suicide (24). Phillips and Smith noted that perceptions associated explicitly with death indicated depression (25).
Furthermore, they stated that when depressed patients give pure C responses such as “blood” to the colored area of cards II and III, it represents pathological perception (25). Linder mentioned card IV as suicidal. They believed that the response to card IV, which includes describing it as something “rotten,” “decayed,” or “burned,” reflected severe depression with suicidal content (26).
The Rorschach test has been investigated for more than 50 years to discover its potential value as a suicidal tool for assessment (27-29). There are almost no reviews to collect and summarize the results of the investigations conducted by specialists in this regard in recent decades. There is limited research on suicide indices in the Rorschach test. Therefore, the purpose of this review study was to evaluate studies related to suicide indicators in the Rorschach test to determine whether the use of this test can indicate a risk of suicide in individuals or not.
2. Evidence Acquisition
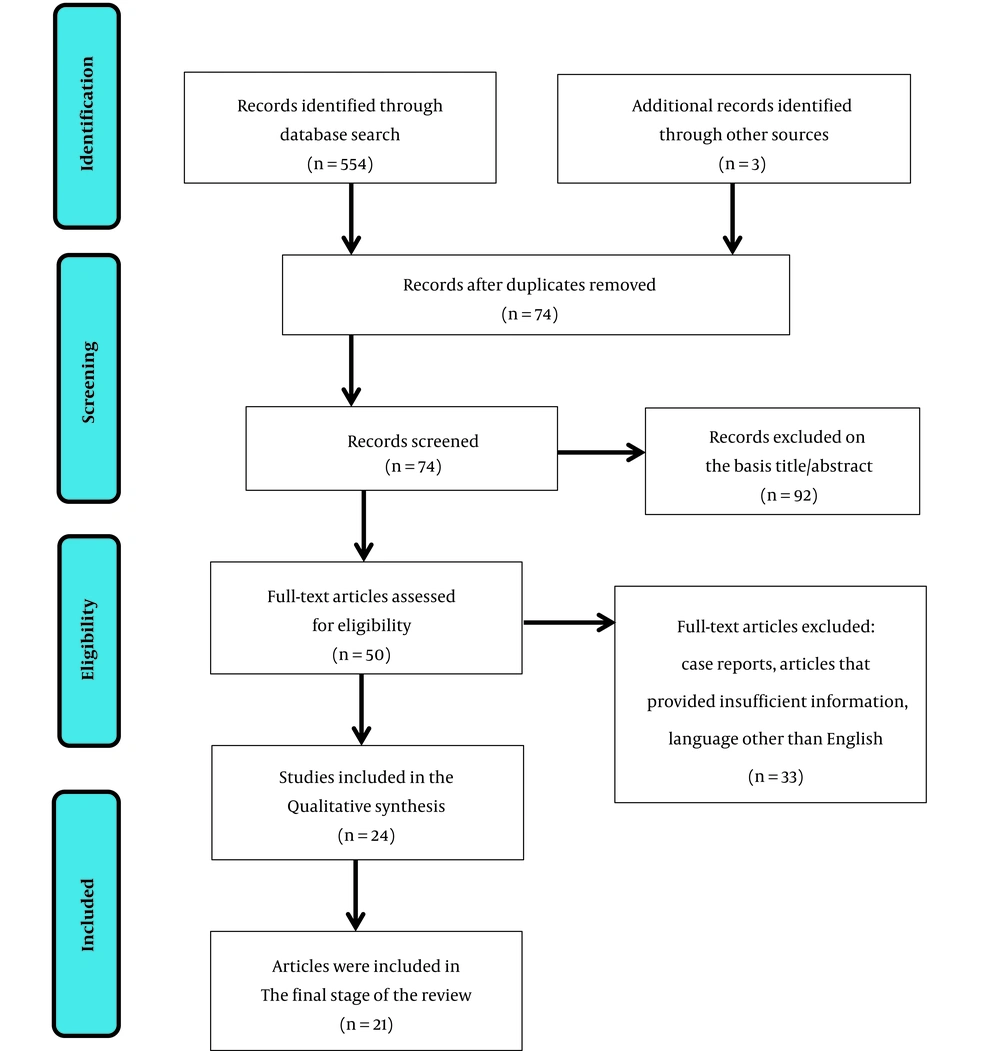
A narrative review study was carried out focusing on the investigations conducted on suicide indices regarding the Rorschach test from 1960 to the end of 2021. The articles were extracted from valid databases, including PubMed, Scopus, and Science Direct, and consequently, 554 articles were detected. The “Suicide” AND “Rorschach” keywords were used to search the databases.
2.1. Criteria for Selection and Assessment of Article Quality
First, a list of titles and abstracts of all articles searched in the databases was provided. Screening and selection of articles and their quality evaluation were performed by two authors independently.
Afterward, the articles with repetitive titles were removed. The abstract of articles was reviewed to determine appropriate research. Inclusion criteria included: (1) investigation must be original, and they must be published in accredited journals and related to the research's purpose; (2) all of them should be descriptive studies; (3) selected articles have to be related to suicide indicators in the Rorschach test. It should be noted that to increase the sensitivity of article selection, the minimum inclusion criteria were considered. However, the following exclusion criteria were regarded to find the most related and high-quality studies: (1) unrelated studies in terms of research design and purpose; (2) studies that provide inadequate information; (3) articles published in a language other than English.
2.2. Data Extraction
In the next step, the context of the articles were studied, and if the full text was unavailable, the researcher contacted the corresponding author via email. If the full text of the article was still not accessible and its abstract did not provide sufficient information, it was excluded from the research. In the initial research, 554 articles were identified. When the articles were checked based on the inclusion and exclusion criteria, merely 21 articles remained for the last stage (Figure 1).
3. Results
A total of 21 studies that met the inclusion criteria were included in the final analysis. Figure 1 shows the research selection process. The total number of samples was 1721, consisting of 19 cross-sectional studies, 1 case study, and 1 cohort study. Among them, three studies were carried out on young, one on children, and 18 on adults. All studies included both males and females. However, only one research in 1960 was conducted on men. Rorschach researchers followed several approaches to suicide assessment.
3.1. Results of Single-Sign Approach
Eleven studies were related to this approach, among which one cohort study addressed rotation. The results showed that the term rotation was primarily used in the mortality groups. In addition, two studies were concerned with the Sapolsky hypothesis regarding the response to the area D6 of Rorschach card VII. In Cooper’s research, the difference was insignificant. In three studies on transparency and cross-section responses about suicide, no significant difference was found in either study. However, the number of responses in a study was more than in the control group (30). Furthermore, five studies were found on the combination of color-shading blend and suicide, among which there was no significant difference just between Blatt and Ritzler (27) and Hansell et al. (31), but three other studies showed a significant relationship.
3.2. Results of the Multiple-Sign/Configurations Approach
We found three studies related to this multiple-sign/configuration approach that influenced suicide prediction.
3.3. Results of Suicide Constellation Approach
Seven studies were done based on the suicide constellation approach, two of which were based on the Martin checklist and five studies concerned with the S-CON index. A score of 7 or more predicts near-lethal suicide attempts.
| First Author (Year) | Objectives | Method | Major Findings |
|---|---|---|---|
| Palmieri et al. (2018) (18) a | Investigating the suicidal thoughts in participants who were mourning due to suicide (suicide survivors) using the Rorschach test. | A Rorschach test was carried out based on the Exner system on 21 suicide victims and 23 healthy participants of the control group. | The t-test demonstrated that the mean S-CON score of survivors with suicidal ideation was significantly higher than that of the control group. |
| Blasczyk-Schiep et al. (2011) (32) b | Studying suicidal behaviors among adolescents and youth using suicide index of Rorschach test. | Four groups included: 1. Suicidal ideation group (n = 30) 2. Suicide attempts group (n = 30) 3. Near-lethal suicide attempts group (n = 26) 4. Control group (n = 30) | The Rorschach’s test response revealed six potential indices of suicidal behavior. At least four indices out of six Rorschach suicidal indices can identify 69% of participants who took severe measures to commit suicide. |
| Petot (2002) (33) c | Identifying suicidal ideation among children using the color-shading index of the Rorschach test. | 43 children in three groups; 1. Suicidal group (n = 14); 2. Depressed non-suicidal group (n = 15); 3. Anxious participant group (n = 14) | The combination of color-shading was the main variable distinguishing suicidal children from the other two groups. |
| Fowler et al. (2001) (34) a | Investigating the relationship between the suicide system of a comprehensive system of Rorschach and lethality of a suicide attempt during hospitalization of patients in the Austen Riggs Center. | Three groups include:; 1. Non-suicidal group (n = 37); 2. Suicide attempts group (n = 37); 3. Near-lethal suicide attempts group (n = 30); and 50 students as the group of non-clinical comparison | The logistic regression analysis indicated that the S-CON score of seven or higher among nine psychiatric and demographic variables merely predicted the near-lethal suicide attempts. |
| Silberg and Armstrong (1992) (35) a | Assessment of Rorschach test in predicting suicide of hospitalized depressed adolescents. | 26 severely depressed suicidal adolescents; 26 severely depressed non-suicidal adolescents; 28 non-depressed non-suicidal adolescents. | Four out of six variables of the suicide system identified 64% of suicidal adolescents. |
| Hansell et al. (1988) (31) c | Assessment of the validity of single-sign Rorschach indices as low indices of current suicide. | A Rorschach test was carried out on 41 depressed hospitalized patients. | It was revealed that the color-shading sign is related to a low risk of suicide. Sign of transparency has no relationship with the current risk of suicide. However, a suicide attempt background might indicate a suicidal personality, and they might be or might not be at the immediate risk of committing suicide. |
| Thomas and Duszynski (1985) (36) c | The frequency of the use of the term whirling in the Rorschach test. | A cohort study was carried out on 1337 graduated medical students from 1948 to 1964. Among them, 1154 students participated in the Rorschach test. | When the ratio of individuals was compared using the rotation terms among the healthy, suicidal, etc., groups, the mortality group used the highest ratio of these terms. |
| Arffa (1982) (37) b | Assessment of multiple-sign approach of Rorschach test in predicting suicide in adolescents. | Forty-eight hospitalized adolescents were divided into four groups (n = 12). | Based on variance analysis, the Rorschach scores at the level of 0.001 in all suicidal groups differed from the control group. |
| Kendra (1979) (38) b | Predicting suicide using the Rorschach test. | A sample including 375 Rorschach protocols was divided into three groups (n = 125). Control group, suicide attempt group, and factors affecting suicide group. | The step-by-step method of multiple analysis demonstrated that six variables successfully classified the factors of suicide, suicide attempt, and psychiatric controls. |
| Rierdan et al. (1978) (30) c | Mutual approval of Blatt and Ritzler (1974) per responses of suicide and Rorschach transparency. | Comparing the Rorschach protocols of 14 participants who committed suicide with 14 participants with no suicide attempt. | The number of transparency and cross-section responses in the suicide groups was more than in the control group. |
| Kestenbaum and and Lynch (1978) (39) c | Examining the hypothesis that transparency responses occur in patients with suicidal attempts. | From the clinical files, the Rorschach records of 10 psychiatric suicide records and ten psychiatric patients who have never committed suicide. | Responses of transparency and cross-sections in the suicidal group were not different from the non-suicidal group. |
| Exner (1977) (24) a | Determining whether the suicidal system scored higher on Rorschach protocols of participants who committed suicide or not. | Three groups per Rorschach protocols include:; Committed suicide before (n = 59); Suicide attempts (n = 31); participants who participated in the Rorschach test 5 days after committing suicide (n = 33) | Eleven variables with the cutting line of 8 or more distinguished the suicidal participants from three control groups. S-CON accurately identified 44 out of 59 suicidal cases (approximately 75%). |
| Blatt and Ritzler (1974) (27) c | Testing the hypothesis that the responses of transparency first occur in suicidal patients. | Clinical records of Rorschach tests of 12 psychiatric patients who committed suicide and 12 who never committed suicide were compared. | Per the result of the t-test, the responses of transparency and cross-sections in the suicidal group were more than in the non-suicidal group, and the difference was significant. |
| Colson and Hurwitz (1973) (40) c | Discovering a new tool for more examination of color-shading and its relationship with suicide. | Per records of 35 hospitalized patients with at least one serious suicide attempt, 17 volunteers were selected. | Seventeen pairs of hospitalized psychiatric patients who committed suicide gave considerably higher shaded responses to the colored cards than participants with no records of suicide. |
| Cutter et al. (1968) (41) a | Examining the Rorschach suicide signs and suicide attempts. | 60 hospitalized war veterans were divided into two groups: A group of participants with records of suicide attempts and a group without records of a suicide attempt. | The biserial correlation coefficient results revealed a significant relationship between the Rorschach suicidal signs and suicidal attempts. |
| Appelbaum and Colson (1968) (42) c | Reinvestigation of Rorschach color-shading in relation to suicide. | Per clinical records, the experimental group consisted of 42 participants with a mean age of 32. | The color-shading responses among the group who committed suicide were considerably higher than those who never committed suicide. |
| Cooper (1965) (43) c | Taking measures to mutually confirm the Sapolsky hypothesis in response to the D6 area of Rorschach card VII. | Per records of 299 patients hospitalized in a psychiatric hospital, 53 participants responses to the D6 area who belonged to the experimental group, and 53 participants were selected as the control group. | The findings did not confirm the Sapolsky hypothesis. There was no significant difference between the groups concerning suicidal ideation. |
| Sapolsky (1963) (44) c | Examining the D6 area of Rorschach card VII. | Two groups included:; Experimental Group: (n = 28); control Group: (n = 28) | The results suggested that the D6 area predicted suicide in 70% of participants. |
| Appelbaum and Holzman (1962) (45) c | Investigation of Rorschach color-shading dimensions in relation to suicide | Two experimental groups and three control groups. Twenty-nine psychiatric patients in the experimental group comprised the suicide group and 120 participants in the control group. | Results revealed that Rorschach color-shading index is a good predictor for suicide assessment. |
| Weiner (1961) (46) a | Mutual validation of Martin checklist and its relationship with suicidal tendency. | Records of the Rorschach test of 24 psychiatric patients who committed suicide and 63 patients who never committed suicide were compared. | Two signs of C or CF first appeared in cards VIII-X, plus P<3 and F+ % >60 were found in protocols of the suicide group. Martin signs accurately identified 79% of participants with a suicide attempt. |
| Daston and and Sakheim (1960) (47) a | Comparing Martin’s checklist with Rorschach’s records in the suicidal ideation group. | All male adults hospitalized with functional psychosis were divided into three groups: 1. Suicide attempt group (SA) (n = 36); 2. successful suicide group (SS) (n = 36); 3. control Group (n = 36) | Variance analysis suggested a significant difference between the suicidal group and control group, plus it distinguished six signs of the suicidal group from the control group out of 17 signs of the Martin approach. |
a Suicide constellation approach
b Multiple-sign approach
c Single-sign approach
4. Discussion
Suicide per 800,000 deaths annually is on the list of the top 20 causes of death worldwide (4). For every person who dies by suicide, over 20 others make a nonlethal effort, and others have serious thoughts about ending their lives (48). A close link exists between psychiatric disorders and a high risk of suicide or suicide attempt (49, 50); the risk of lifetime suicide is about 5 - 5.6%, but the suicide rate is higher and ranges between 10 and 50% (51, 52). Forty percent of patients experienced recurrent suicidal ideation that continued or increased in the first years of treatment (53). There is ample evidence to support several psychological therapies, including cognitive-behavioral and dialectical behavioral therapy, to prevent suicide (54, 55). In recent years, brief patient-specialist interventions have been defined to reduce the risks of suicidal behavior (56, 57). It is vital to focus on suicide; however, ideation is the predictor of suicide and the basis for prevention (58). Identifying suicidal ideas in a person is crucial to timely interventions and can save many lives. The individual might not seriously express their intentions to hurt themselves, and the signs might be revealed merely after their suicide attempt. As such, the clinical specialist must be able to identify people who have suicidal thoughts but cannot explicitly express them. The projective psychological tests can identify the suicidal ideation in a person’s mind by detecting the traits and conditions related to suicidal behavior, such as impulsivity and despair, and provide crucial clues for clinical specialists. Hence, projective tests like Rorschach are the best option possible in this regard. The patient is not aware of the purpose of the assessment and is incapable of detecting them (59).
The findings suggested that the single-sign approach used a particular l Rorschach sign to predict suicide. Immediate identification of suicide from a Rorschach variable, which is easily detectable, is an advantage (31).
White argued that rotation is one of the Rorschach responses, identifying a mind dealing with death wishes (29). Thomas and Duszynski examined the Rorschach responses of more than 1000 medical students (36). They found that whirling and its synonyms are more frequent in the protocols of individuals who will have suicidal thoughts in the future (36). Another research showed examples of whirling and its synonyms in other studies (60). Studies revealed that individuals with suicidal thoughts often provide more transparent responses (27, 30, 39). Transparent responses are considered to be a sense of losing or being disparate (27). Also, Sapolsky noted a significant relationship between suicidal ideation and response to small details in area D6 of Rorschach card VII (44). The first hypothesis is obtained from a psychoanalyst concept and suggests that the suicidal idea reflects the subconscious intention to return to the mother’s womb. The lower central details on card VII are frequently perceived as an area of the vagina. Patients with suicidal thoughts are expected to provide more responses to this area than patients without suicidal thoughts (44). Studies found no evidence to support the Sapolsky hypothesis (41, 43, 44, 61).
The color-shading responses are regarded as sensitive suicide indicators. The combination of color-shading demonstrates a failure to deal with pain effectively (34). Furthermore, it can reflect a confusing, pleasurable, and painful emotional experience (24). Appelbaum and Holzman found a relationship between the color-shading responses and the records of suicidal attempts (45). Various results were obtained regarding the validity of this hypothesis. Several studies provided evidence in support of this assumption (40, 42). While it was not confirmed in other studies (27, 31), Petot pointed out that color-shading responses are more frequent in the Rorschach protocols for children with suicidal ideation (33). The presence of shadow-color responses in the protocols of individuals attempting to commit serious suicide has been reported in many studies (Table 1). Therefore, the presence of shadow-color responses in a protocol must be taken seriously, even if their number is minimal (16). Apart from that, several other signs, such as a weak form of motor responses and responses, including pathological content, were observed in Rorschach protocols of individuals with suicidal ideation and the suicidal system (33, 35). The absence of signs in a person should not be regarded as a lack of suicidal ideation. Some individuals might be unable to provide complicated cognitive responses such as transparency and cross-sections (27). Moreover, it is not necessary for the existence of a sign to be related to current suicidal ideation. Hansell et al. suggested that transparency of responses had no relationship with current risks of suicide (31).
In addition, Hertz Multiple-signs/Configurations approach presented the most comprehensive and completed theory based on the research data (62). For them, suicide is aggressive behavior that can lead to self-destruction. Hertz's approach perfectly covers the factors leading to suicide, which helps conduct a better prediction (62). Hertz believed that the Rorschach test does not predict suicidal behaviors, yet it assesses the personality traits that can lead to such behavior (62). The Hertz approach identifies the combination of signs, content analysis, and 14 various Rorschach indices, which indicate the possibility of suicide (62). Among 14 indices, 10 cases differed between the suicidal and non-suicidal groups. They found that the most significant configuration of suicide includes depressed mood, deep anxiety, confliction, arousal, pathological thoughts related to hypochondriasis, horrifying physical imaginations, and a sense of futility. These factors include a higher risk of suicide (62). Their findings were proven numerous times, and their study is the most complete and influential research concerning the configural approach. However, suicide is a complicated behavior, and a single-sign or a configural approach must be approved together with other clinical data.
The findings suggested that one of the earliest proposed suicide systems was Martin checklist, which comprised 17 Rorschach signs (63). Martin specified several Rorschach factors associated with suicide tendencies, which in terms of area (D < 6 or > 20; D% < 60 or > 79), shape surface (F + %: 60), color (CF > 0, ∑C > EM, 8 - 9 - 10% > 29), shading (including perspective and Y responses), and content (H + Hd > 6, P < 3 or > 6, number of categories < 6 or > 13) (63). Several investigations supported the relationship of Martin signs and suicide potential (46, 47). White and Schreiber demonstrated that the sixth Martin sign identifies the suicide potential (29).
Exner and Willy offered a constellation on the basis of a comprehensive system (CS), known as S-CON (28). Several aspects of S-CON were identified in the studies. Rorschach variables included 12, and the cut line was considered seven (Table 2).
| Single-Signs | Comprehensive System's S-CON | Suicidal Index for Adolescents |
|---|---|---|
| 1. Whirling responses | 1. FV + VF + V + FD > 2 | 1. CF + C > FC |
| 2. Transparency responses | 2. Color shadingblend > 0 | 2. FV + VF + V > 0 |
| 3. Color-shading responses | 3. Egocentricityindex < 0.31, > 0.44 | 3. Color shading blend > 1 |
| 4. Responses with morbid contents | 4. Mor > 3 | 4. Weighted specialscores > 9 |
| 5. Zd > ± 3.5, Zd < -3.5 | 5. M- > 1 | |
| 6. es > EA | 6. Mor > 0 | |
| 7. CF + C > FC | ||
| 8. X + % < 0.70 | ||
| 9. S > 3 | ||
| 10. P < 3, > 8 | ||
| 11. Pur H < 2 | ||
| 12. R < 17 | ||
| Cut-off ≥ 7 | Cut-off ≥ 4 |
a Source: Kumar et al. (59)
Palmieri et al. showed that the mean score (S-CON) was significantly higher among suicide survivors than the score (S-CON) of the Rorschach test compared to controls (18). S-CON is one of the most common methods used for the assessment of suicide and accurately identified 44 out of 59 suicide cases. Thus, it is recommended to consider the protocols of individuals with an S-CON score of eight or higher. In addition, it must be taken into account that about 25% of people who committed suicide did not score 8 in the S-CON. Therefore, even the lower scores must be precisely assessed as a sign (16).
In general, it is possible to conclude that projective tests can predict and identify the risk of suicide. However, most findings are preliminary and require additional research to achieve definite results. Numerous studies have been carried out on suicide assessment using the Rorschach test, and none of the proposed hypotheses have been confirmed. It does not signify that the hypotheses are clinically useless. Therefore, there are no studies to assert with certainty that a single sign or configural sign might be an indication of the possibility of suicide risk. Suicide is a multifaceted action, and the most statistically valid suicide predictor is devoid of meaning with no clinical specialty.
In this study, we encountered some limitations. The available data were collected through a narrative review instead of a meta-analysis for two reasons. First, the studies were only a few, and the sample size for many studies was minimal. Consequently, further research was required to conduct a meta-analysis. Second, the results of the studies varied widely across investigations; therefore, it was challenging to integrate the data into these studies for a meta-analysis. This review study emphasizes the importance of suicide prevention to formulate a hypothesis for future studies and can be used as a diagnostic tool to help psychiatrists and clinical psychologists. Given the issue’s importance and the severe and irreversible consequences of suicide, it is suggested that more research and clinical work be done in this area to reduce suicide attempts. We are hopeful that these preventive efforts might create a broader perspective and lead to an understanding of the complexity and heterogeneity of individuals with suicidal tendencies and behaviors, strengthen human beings so they can maintain themselves, wish to live, and reduce the incidence of suicide in society.