1. Context
In late 2019, the first cases of coronavirus disease 2019 (COVID-19) infection were reported, which subsequently became a global pandemic as characterized by World Health Organization (WHO) (1-5). The coronavirus disease 2019 is very contagious (6). There is currently strong evidence of easy and rapid human-to-human transmission, often through small respiratory aerosols and droplets produced during speaking, sneezing, or coughing (6-8). These small particles may be suspended in the air for a long time before settling on the surfaces (1, 9, 10). Though the pandemic seems to go away due to vaccination, there are also some reports of its representation around the world (11). So, observing infection control precautions is the only current option for reducing new cases of infections (6).
Numerous studies have been conducted in the last few years in different populations and age groups, including children, since the appearance of the first COVID-19 case. Angelopoulou et al. studied the impact of COVID-19 on the oral health status of Greek children in 2023 and showed the adverse effects of the pandemic on brushing frequency, sugar consumption, dental caries, and dental treatment needs (12). A study performed by Bauer et al. in 2023 to reveal the impact of the COVID-19 crisis on the postponement of a child’s elective dental procedures showed no differences in extractions before and after the pandemic. However, the number of tooth restorations decreased significantly compared to the pre-COVID-19 period (13). Campagnaro et al.’s study evaluating the effect of COVID-19 spread on child’s fear, eating habits, and parent’s oral health perceptions disclosed changed eating habits of children and the routine daily life of families regarding seeking dental care for their children (1).
During the pandemic, the interventional dental needs of children were divided into two distinct categories: Emergency clinical conditions and non-emergency clinical conditions (10). Acute pulpitis and periodontitis, food impaction, and dental trauma are some kinds of emergencies in the field of pediatric dentistry (5, 10). With the global spread of COVID-19, specific guidelines were issued by the international communities to prevent further spread of the infection and provide a safe environment for people and dental professionals (10, 14). By adhering to these guidelines and strategies, the dental staff played a critical role in controlling the epidemic (2).
However, the question now comes to mind is how COVID-19 affects pediatric dentistry and oral health. As a pediatric dentist, the first author was repeatedly confronted with the parents' statement: “We did not bring our child for treatment due to fear of COVID-19,” or “We waited for the pandemic to end, but it did not end until the baby's teeth got worse and worse.”
In order to be aware of the effects of such a global crisis on the oral health status of children as our future generation, it is critical to avoid more complex dental treatment needs or some oral-health-related morbidity conditions. Moreover, reviewing the oral effects of COVID-19, suggesting practical recommendations, and emphasizing relevant global guidelines are the prerequisites to making appropriate decisions by policymakers to improve pediatric oral health. To the best of our knowledge, sparse reviews are now available investigating the impacts of COVID-19 and compensatory practical solutions as a whole. Therefore, given the importance of the matter, the authors decided to prepare a narrative review by searching international databases to provide useful and comprehensive information for readers regarding the impacts of COVID-19 on pediatric dentistry services and oral health status.
2. Evidence Acquisition
This narrative review was designated to focus on different studies relating to various impacts of the COVID-19 pandemic on pediatric dentistry and oral health status in the pediatric population, published from late 2019 to June 2023. Electronic searches were performed in Web of Science, PubMed, MEDLINE, EMBASE, Cochran Library, Scopus, Google Scholar, and Google scientific databases using Medical Subject Headings (MeSH) terms of “Coronavirus, COVID-19, Dental Care for Children, Dental Health Services, Pandemics, and Pediatric Dentistry” in the titles or abstracts of the published articles. Terms were also used in various combinations to search.
2.1. Article Selection and Quality Assessment Criteria
In the current review, the inclusion criteria included: (1) Articles written in English or Persian language, (2) original or review articles on the present topic published in accredited databases, and (3) articles dealing with human subjects. Articles presented at scientific conferences were also searched. Furthermore, articles that were unrelated to our review purpose or showed irrelevant data were excluded.
Firstly, according to the initial search based on inclusion criteria, both title and abstract of each extracted article were listed and thoroughly studied. Secondly, the prepared list was checked, and repetitive and misleading articles were removed. Then, to find appropriate articles, all abstracts were critically reviewed. Both reviewers read, scanned, and recorded appropriate findings of the articles independently. Since it was possible for the authors to ignore some findings and highlight others, they reached a consensus on the final findings. Finally, the appropriate findings were reported. In the following, the manuscript’s drafting, critical reviewing, and editing were performed by both authors.
2.2. Data Extraction
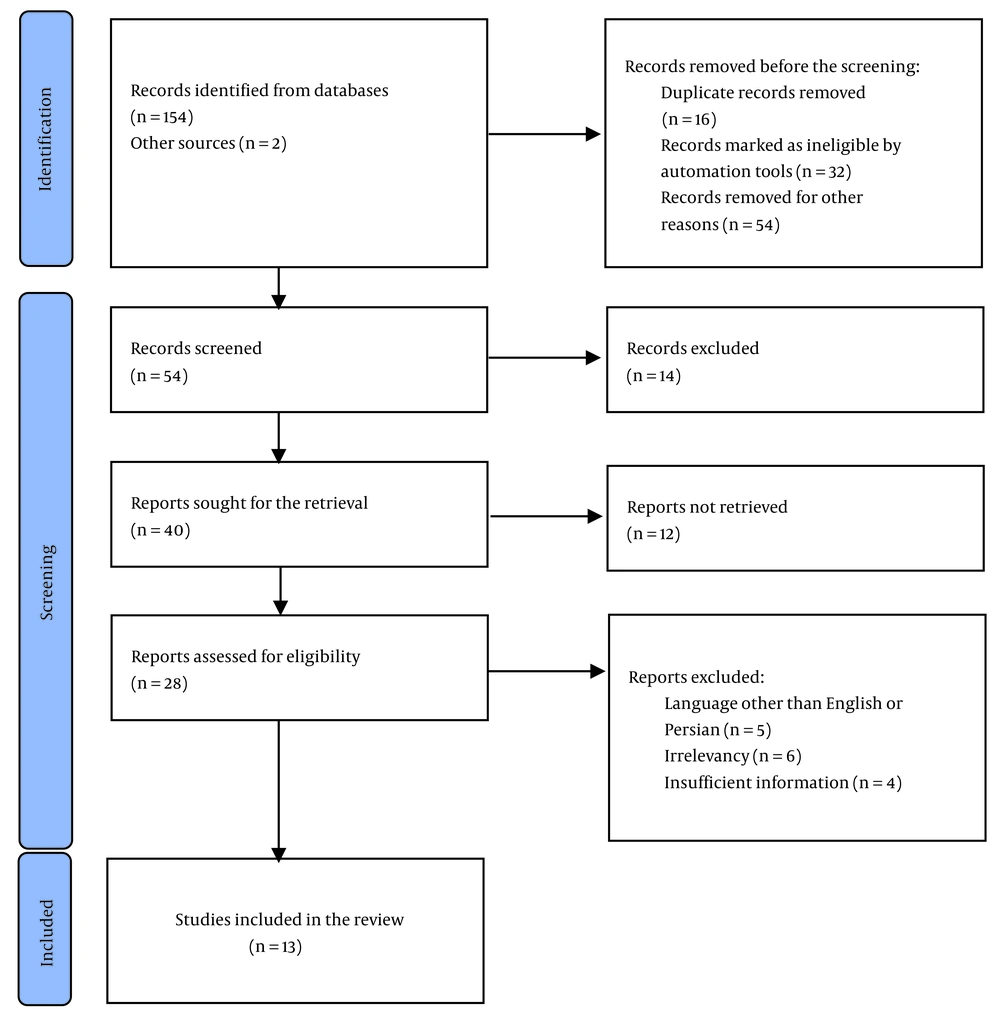
Articles published between 2019 and 2023 on the COVID-19 pandemic were used and critically reviewed in the current review. In addition, to collect more relevant articles, some articles’ references and scientific meetings were manually searched again. The corresponding authors were contacted if the full text was not accessible. Otherwise, the article was excluded. In the initial step, 156 studies were identified. After controlling based on inclusion criteria, only 13 remained that fulfilled the purpose of this review and fitted to discuss the subject (Figure 1). After reading the articles completely, a special form designed by the authors was used to record the titles and suitable findings of the final articles.
3. Results
Considering inclusion criteria, a total of 13 articles were used to extract our results, consisting of 6 descriptive-analytical original and 7 review studies. All studies included both sexes. Figure 1 demonstrates the study selection process. As presented in two parts, the main findings of the electronic search throughout sequential elimination steps of irrelevant articles are as follows.
3.1. The Results of Factors Affecting Pediatric Dentistry in the Coronavirus Disease 2019 Period
What is certain is that the COVID-19 outbreak severely and negatively affected different preventive and treatment modalities in pediatric dentistry through factors listed below:
I. Social isolation, known as quarantine: Peloso et al.’s study addressed this issue, and quarantine was demonstrated to have an impact on dental appointments (15).
II. Dentists’ reduced work: Three investigations were regarding dental professionals’ reduced time work, including Coulthard (2), Schwendicke et al. (16), and Gasparro et al. (17), and found that daily working hours reduced in dentistry dramatically.
III. Not attending dental treatments: Chisini et al.’s research in Brazil indicated that the percentage of dental services obviously decreased after the virus’s first appearance (18).
IV. The possibility of children being carriers: Four studies, including Luzzi et al. (10), Chisini et al. (18), Mallineni et al. (19), and Cianetti et al.’s (5) studies, were found concerning this tip, all concluding that children might be potential carriers of the virus, and agreed that special considerations should be made in this regard.
V. Other risk factors in pediatric dentistry: There was only one study, i.e., Luzzi et al.’s (10), assessing more risk factors in pediatric dentistry than in adult dentistry causing additional virus transmission among pedodontists, dental assistants, and other involved individuals, which concluded that the unavoidable presence of a child’s parent or guardian might act as a risk factor for additional contamination.
VI. Changed dietary habits: According to our search, there were three related articles, i.e., Campagnaro et al. (1), Angelopoulou et al. (12), and Cianetti et al.’s (5) studies in this regard, showing that school closures and reduced physical activity led to increased time to stay at home and altered and frequent consumption of sugary foods.
3.2. The Results of Factors Helping us Prevent More Virus Contamination
As dental team members, how can we still prevent further spread of COVID-19?
I. Essential primary triage (after triage by phone call or telemedicine): By finding two studies, it was shown that potentially infected or suspected patients should be yet identified at check-in. As concluded by Cianetti et al. (5) and Luzzi et al.’s (10) studies, at the beginning of arrival, questions are asked about the symptoms of infection in the child and their carers, the history of attending areas judged to be high-risk places of infection over the past two weeks, and the history of contact with a confirmed affected or suspected patient over the past month. The next step is to take the body temperature and then complete the screening form. This form includes questions about the possibility of fever and chills over the past two weeks and symptoms such as dry cough, sore throat, fatigue, shortness of breath, difficulty breathing, nausea, vomiting, headache, body or muscle aches, stomachache, chest pain, loss of taste or smell, and loose stool.
II. Personal protective measures and office preparation: Three articles were found in this regard (5, 9, 20), showing that involved individuals should use medical disposable gloves, shoe covers, masks, gowns, eyeglasses, and face shields, and wash their hands frequently. As stated by Cianetti et al. (5) and Bahramian et al. (20), the risk of transmission and contagion will increase whenever one item is refused. Based on Cianetti et al. (5) and Medeiros et al.’s (9) studies, another point that needs attention is setting a safe and secure time frame for patients to avoid contact or even proximity with other patients and avoiding overcrowding and overlapping dental appointments.
III. Remote communication: As perceived by two relevant articles by Barabari and Moharamzadeh (3) and Mallineni et al. (19), many activities, including instruction regarding preventive measures in the field of oral health, can be taught remotely, such as through online communication.
4. Discussion
Maintaining good oral health is the highest goal of pediatric dentistry (10, 21). However, what has been gained over the years might be lost in the COVID-19 period. Indeed, the negative impacts of the epidemic could jeopardize the preservation of good outcomes obtained before the pandemic (18). For example, quarantine, which means restrictions on the transit of people, social activities, and cancellation of many gatherings (a kind of isolation), was accomplished and severely affected the number of dental attendance. As we all know, many countries have implemented different courses of quarantine to reduce sources of interpersonal transmission which, in turn, has greatly affected various dental specialties, including dentistry.
Dental treatment of children during the pandemic crisis included measures pursuing two important goals: First, to prevent the transmission of infection from the patient to the dental health workers and vice versa, and second, to return the patient to the previous state of well-being (5).
According to the WHO guidelines, the vast majority of dental professionals drastically reduced their workload to the extent that some procedures were close to a complete cessation (18). Evidence suggested that the disease became a challenge for various professions, such as dentistry, as it forced those involved in this profession to reduce ordinary work (1, 19). In a Brazilian study, the effect of the outbreak on the total number of pediatric dental procedures was calculated by comparing two different time points: At the time of identifying the first COVID-19 case (February 2020) and at the peak of the epidemic (April 2020). Compared to the pre-epidemic period, the analysis showed a 66% and 89% reduction in pediatric treatments completed at the time of the first case report and at the peak of the epidemic, respectively (18). Another factor was the unwanted and natural fear of COVID-19 infection in families when the situation quickly got out of control. It caused not attending dental clinics and consequently increased cases of self-medication for pain relief. Thus, a high percentage of children remained untreated.
It is important to pay attention to the presence of symptoms, although their absence does not mean the disease rejection (22). Any age group might be susceptible to infection (5). Although the highest rate of virus transmission occurs from symptomatic individuals to others, some people, including children infected with COVID-19 with no developed symptoms, might be able to spread the infection and the virus, which could then infect others. Since children can be asymptomatic carriers of the virus or have mild and nonspecific symptoms of infection compared to adults (10, 18, 19), they can further reduce the number of treatments provided to children.
The patient’s parent or guardian’s unavoidable presence may lead to further spread of infection, particularly when more than one person accompanies the child patient. Discomfort and intolerance perceived by the child to wear personal protective equipment was another factor to the extent that it can be said that children under the age of 2 never wore a mask. Moreover, there were potential risks, including self-contamination of the mask with contaminated hands in the pediatric population.
The sedentary habits of staying at home and the resultant altered diet, in turn, facilitated the accumulation of debris, plaque, and microbial biofilm and ultimately increased dental caries as the most prevalent infectious disease and periodontal involvement (1, 5).
Both dental professionals and patients are still at great risk of involvement through cross-infection and being the potential carriers of the virus (5, 7, 8, 10, 19, 23-26). There is still a major risk of infection transmission in dentistry because the virus is mainly transmitted through respiratory droplets, sneezes, aerosols, and breathing (5). So, according to guidelines and standard precautions, dental practitioners across the world should consider sufficient time intervals between patients, daily disinfection of surfaces, regular hand washing with soap and water, hygienic disposal of waste, and attention to issues such as rubber dam usage, high-volume suction, ventilation, and disinfection (5, 10, 27), particularly designated handpieces with valves that act as anti-retractive pieces, significantly decrease virus transmission. Regular disinfection precautions with ethanol or sodium hypochlorite-based solutions are among the principles of infection control during the COVID-19 period (5). Mouthwash also helps a lot in reducing the contamination load. Although the possibility of proper rinsing is little at a young age, swabbing the mucous surfaces of the mouth with gauze moistened with disinfectant mouthwash may be a practical alternative in young children. Rubber dams should also be used as a routine during dental treatment for patients (5). Additionally, adherence to the following guidelines is strongly recommended: Installing visual alerts such as posters instructing personal hygiene at the entrance and waiting room, providing hand sanitizer, paper towels, and no-touch receptacles for disposal, etc., placing physical barriers such as glass windows to minimize contact in the waiting room, keeping chairs at least six feet (2 meters) apart in the waiting room, removing magazines, books, and toys, and other unnecessary items from the waiting room, and accompanying each child by only one family member and no more. Antimicrobial mouthwashes such as 1% hydrogen peroxide or 0.2% povidone may also be useful (20). Furthermore, it should be ensured during the pre-appointment phone call that the child comes to the office with only one accompanying person.
There are still some important points about COVID-19 in children, predisposing them to become active carriers of COVID-19. Child patients may be thoroughly asymptomatic or represent nonspecific symptoms (28). In most cases, involvement of the inferior respiratory tract rarely happens (20). Comparing adults with pediatric populations, the probability of cross-infection from children is higher due to their mild symptoms of infection and longer incubation period (29), showing the need for more attention from the pediatric dental team to adopt infection control guidelines and adhere to restrictive precautions.
From the perspective of pediatric dentistry, due to the COVID-19 pandemic, many pediatric subjects have been left untreated. Subsequently, their dental status is getting worse day by day (19), and with increasing dental problems, the vicious cycle begins and continues. Pain, dental abscess, increased number of extracted teeth, impaired chewing function, and malocclusions are inevitable consequences (5, 30). Therefore, to avoid these consequences, we have to offer the option of providing services with a strong emphasis on infection control.
Apart from worrying about the future, with the affected dental health under the heavy shadow and consequences of COVID-19, including the high costs of future treatments in the long run, the oral health-related quality of life has been affected as an immediate consequence (19). In addition, the condition has led to increased stress and anxiety (1, 31). In addition to the psychological effects, changes in diet, along with the lack of preventive dental care, can affect the oral health of people, especially pediatric subjects across the world (1). After the crisis, optimistically eliminating or reducing the onset of adverse dental conditions and therefore improving oral health should therefore be fundamental (10).
In the case of mild pathological conditions that do not require direct intervention or can be postponed, parents can also be given remote training to control the circumstance (10). It is the dentist's ability to monitor the child's oral health status through effective interaction with parents to guide them to correct daily oral hygiene measures (10). The main focus of the recommendations provided in distance education is on adequate at-home daily oral hygiene, using caries-preventive products such as fluoride compounds at home (children who are categorized in the moderate- and high-risk categories based on caries risk assessment), and proper nutritional considerations provided by adults for the child (5, 10, 20). Particularly for the preschool age group, parents-child bacterial transmission is an important issue often forgotten. So, rigorous adherence of parents themselves to oral hygiene performance is highly recommended. Hence, efforts should be made to compensate for the situation, including new distance technologies and teledentistry as efficient communication tools between dentists and parents (5, 9, 19, 30).
4.1. Limitations
We faced some limitations in our review. The number of selected articles was limited. However, due to the previous coronavirus pandemic, an active research field has been created, and more research in this regard is suggested. In the current fragile context of COVID-19, and until further research results are available and the release of future updates, it may be necessary to reconsider the range of pediatric dental activities to minimize the risk of cross-infection again. The authors re-emphasize that treatments on a scheduled basis are allowed in accordance with infection prevention protocols by adopting strict protective measures for all involved. In addition, we all know that previous interruptions or slowness in dental healthcare provision may increase demand and put overburden pressure on dental services. On the other hand, since regular and periodic dental check-ups were difficult during the COVID-19 period and in line with the measures taken to control the COVID-19 outbreak, preventive multimedia training is recommended for parents and guardians to prevent the child’s dental status from deteriorating. Thus, there is a great emphasis on telecommunication and distance learning. This outbreak may be a turning point in modern biosafety technology, as it has already been in other distance learning.