1. Background
Transgender people are one of the most marginalized social groups in the world, and they often expose to neglect and discrimination (1). Transgender individuals experience several maltreatment because they are prohibited by existing challenges in legal identity. This can result from no employment or social support and inadequate access to quality health (2, 3). Studies have shown that transgender persons confront several fundamental and systemic barriers to accessing health services (4).
According to the results of a study, there were higher scores of transsexual women’s concerns about their body image and feminine role compared to normal people. This fear affects different aspects of their quality of life, especially sexual health (5). According to health protocols, there are different aspects of sexual health, including prevention and treatment of sexually transmitted infections (STIs), human infection virus (HIV) prevention and transmission routes, high-risk sexual behavior, and breast and reproductive system cancer screening. Competent primary care is needed, particularly after having received limited education for transgender people (6).
A meta-analysis showed that 22% of trans-feminine people are living with HIV in the United States (7). Centers for disease control and prevention for HIV testing measures reported that the percentage of the transgender population diagnosed with HIV was three times the general (8). To reduce the side effects of hormone therapy, female-to-male (FTM) transgender persons need to be screened for breast and cervical cancers, especially those who have not removed the uterus or have not had a mastectomy. There are several needs related to sexual health, such as counseling regarding fertility and infertility decisions, because individuals who have a demand saving gametes and have children. Male-to-female (MTF) transgender should be evaluated in terms of prostate and breast cancer, respectively (9). For cancer screening, a study found higher rates of screening need in transsexual people born as males that changed their gender to female; however, they underwent cervix, breast, and colorectal cancer screening less than the general population (10). In addition to these threats, this group is also exposed to violence, and they experience various forms of violence. Physical and sexual violence is prevalent. This issue predisposes them to substance abuse (11).
Peitzmeier's study showed that transgender individuals experienced 1.7 times more likely any intimate partner violence compared with cisgender individuals. They experience 2.2 times more likely physical violence and 2.5 times more likely sexual violence than other participants (12). Sexual health has been paid little attention in the transsexual population globally (13).
Laws have been passed that support sex reassignment in people with ambiguous sexual identification in Iran, but they are subject to a great deal of mental pressure due to cultural norms (14). There are no accurate statistics which sexual and also high-risk behaviors such as drug abuse in transsexual persons in Iran. According to an Iranian study on 104 transsexual women, two women were diagnosed with HIV. The prevalence of HIV positivity and condom use was 1.9% and 39.7%, respectively (15). Few studies were carried out for STI screening by transgender people. Moreover, there is no study on the prevalence screening of cancer in this group in Iran. Considering these gaps, fundamental research is needed to identify high-risk behaviors and sexual health-related behaviors in the transgender population.
2. Objectives
The present study was conducted to determine the distribution of high-risk behaviors and sexual- and reproductive health-related behaviors of sex-reassigned transsexual subjects.
3. Materials and Methods
Ninety-six sex-reassigned transsexual individuals of both genders presenting to Salamat Bonyan Psychology Clinic were enrolled in a cross-sectional study. This clinic is a center with the most significant number of transsexual subjects in the country. Inclusion criteria were the ability to read and write, a confirmed diagnosis by a trusted psychiatrist, an interval of at least one month between the completion of hormone therapy or gender reassignment surgery and the beginning of the study, lack of genetic or sexual abnormalities like hermaphroditism, a positive history of at least one sexual intercourse, age above 15 years, and lack of registered mental disorders according to the medical record.
The Ethics Committee of the Iran University of Medical sciences (IR.IUMS.REC.1397.340) approved the study protocol. The researcher was introduced to authorities and transsexual subjects by an official letter from the university. Participants were informed that their data would be anonymized and kept confidential before completing the questionnaires.
3.1. Instruments
The demographic form included age, education level, occupation, gender, birth time, insurance, identity certificate status, and married status. The scale was a researcher-made questionnaire about sexual health and high-risk behaviors. To develop the sexual health questionnaire, the researcher extensively searched books, journals, and valid websites for related studies and carried out a systematic search in protocols and guidelines formulated for transsexual subjects, and during a qualitative manner with transgender people and based on the experience of the researcher for years. This scale has two dimensions: First, the questions for cancer-related screenings and tests related to sexually transmitted infections. Second, the questions for evaluating sexual and high-risk behaviors. Finally, 38 questions were selected. The content validity of the questionnaire was performed by an expert group in this field, including two persons with reproductive health Ph.D. degrees, one sexologist, one psychologist, one epidemiologist, and one general surgeon. Modification comments about the questionnaires were sought from experts. The content validity index (CVI) was calculated using the guidelines proposed by Waltz and Bausell (quoted in Polit et al.). It was found to be acceptable as it > 0.79 (16). Reliability was assessed by thirteen transgender people using test-retest (r = 0.83) and Cronbach’s alpha coefficient (0.89). Questions related to scale were the type of condom (usual, vaginal), HIV infection, STI infection in the present time, type of substance abuse, source of information about STI (social media, friend, family, and clinic), condom use in the last sex act, and type of breast screening (sonography and mammography). All data are shown in Tables 1 and 2. This scale describes the prevalence of high-risk sexual behaviors in three dimensions, including cancer screening and tests for STIs, factors related to high-risk sexual behaviors, and distribution of high-risk sexual behaviors in reassigned trans-sexual individuals. This questionnaire did not have a cut-off point. Individuals just respond to questions via “yes” or “no” or number.
| Variables | No. (%) | CI%95 (L - H) |
|---|---|---|
| Prostate cancer | (0.89 - 0.99) a | |
| Yes | 1 (4.34) | |
| No | 22 (95.65) | |
| Breast cancer | (0.86 - 0.97) b | |
| Yes | 8 (8.33) | |
| No | 88 (91.66) | |
| Pap smear test | (0.95 - 0.99) c | |
| Yes | 2 (2.73) | |
| No | 71 (97.26) | |
| HPV vaccination | (0.92 - 0.99) b | |
| Yes | 4 (4.16) | |
| No | 92 (95.83) | |
| HBV vaccination | (0.52 - 0.72) b | |
| Yes | 36 (37.5) | |
| No | 60 (62.5) | |
| HIV test | (0.68 - 0.85) b | |
| Yes | 22 (22.91) | |
| No | 74 (77.08) |
Abbreviations: HPV, human papilloma virus; HBV, hepatitis B virus; HIV, human infection virus.
a Prostate cancer follow-up in male-to-female (MTF) subjects, N = 23.
b Breast cancer follow-up in all participants, N = 96.
c Pap smear test follow-up in female-to-male (FTM) subjects, N = 73.
| Variables | No. (%) | CI%95 (L - H) |
|---|---|---|
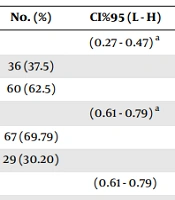
| Sexual violence history | (0.27 - 0.47) a | |
| Yes | 36 (37.5) | |
| No | 60 (62.5) | |
| Having partners in the present time | (0.61 - 0.79) a | |
| Yes | 67 (69.79) | |
| No | 29 (30.20) | |
| Type of partner | (0.61 - 0.79) | |
| Steady | 29 (30.20) | |
| Casual | 67 (69.79) | |
| Number of casual partners | - | |
| Two | 19 (28.35) | |
| Three-five | 35 (52.23) | |
| Six-nine | 8 (11.94) | |
| 10 > above | 5 (7.46) | |
| Condom use | (0.68 - 0.77) b | |
| Yes | 26 (27) | |
| No | 70 (72.91) | |
| A history of an STI | (0.18 - 0.36) a | |
| Yes | 26 (27.08) | |
| No | 70 (72.91) | |
| Information about STI | (0.71 - 0.99) b | |
| Yes | 3 (3.13) | |
| No | 93 (96.87) | |
| Oral sex | (0.89 - 0.99) a | |
| Yes | 90 (93.75) | |
| No | 6 (6.25) | |
| Vaginal sex | (0.75-0.91) b | |
| Yes | 16 (16.66) | |
| No | 80 (83.33) | |
| Anal sex | (0.24 - 0.44) a | |
| Yes | 34 (34.41) | |
| No | 62 (64.58) | |
| Age of sexual debut (y) | (-0.94 - 0.99) c | |
| 6 - 14 | 30 (31.25) | |
| 15 - 30 | 66 (68.75) | |
| Substance abuse (smoke, alcohol, drug) | (0.20 - 0.39) a | |
| Yes | 29 (30) | |
| No | 67 (70) | |
| Substance use before the sex act | (0.61 - 0.79) a | |
| Yes | 7 (7.30) | |
| No | 88 (92.70) |
Abbreviation: STI, sexually transmitted infections.
a Answer with yes.
b Answer with no.
c Age of sexual debut < 14 years.
3.2. Statistical Analysis
This study was conducted from September to December 2019. Descriptive variables are presented as numbers, percentages, mean, and standard deviation (SD). SPSS software version 16 was used for data analysis.
4. Results
According to demographic findings, 96 individuals completed the hormone therapy process, of whom 43 underwent sex-reassignment surgery. Moreover, 73 subjects were FTM, and 23 persons were MTF. Additional demographic characteristics of the participants are summarized in Table 3.
| Variables | No. (%) (n = 96) |
|---|---|
| Age (y) | |
| 16 - 29 | 67 (69.79) |
| 30 - 45 | 26 (27.08) |
| > 45 | 3 (3.1) |
| Education level | |
| High school | 2 (2.3) |
| Diploma | 52 (53.95) |
| Academic | 42 (43.75) |
| Occupation | |
| Employed | 42 (43.75) |
| Unemployed | 55 (56.25) |
| Gender birth | |
| Girl | 73 (76) |
| Boy | 23 (24) |
| Having insurance | |
| Yes | 45 (46.87) |
| No | 51 (53.13) |
| Identity certificate status | |
| Change | 38 (39.58) |
| No change | 58 (60.41) |
| Married status | |
| Unmarried | 88 (91.66) |
| Married | 8 (8.34) |
In this study, 97.9% of the participants did not take a Pap smear test (CI: 0.95 - 0.99). Moreover, 96% and 92% of the participants were not screened for prostate cancer (CI: 0.89 - 0.99) and breast cancer (CI: 0.86 - 0.97), respectively. Also, 62.5% of the participants never received hepatitis B (HBV) vaccine (CI: 0.52 - 0.72), and 95.83% did not receive human papillomavirus (HPV) vaccines (CI: 0.92 - 0.99). Furthermore, 87.09% did not take a human infection virus test (CI: 0.68 - 0.85) (Table 1). Oral sex was the most common sexual act (93.75%), and 72.91% had never used condoms (CI: 0.68 - 0.77). Regarding the age of sexual debut, 31% of individuals were under fourteen years old (CI= -0.94 - 0.99). Also, 34.4% of the participants had anal sex. Anal intercourse was the most high-risk sexual behavior according to 23% of the participants. Moreover, just 17% of them had vaginal sex. Furthermore, 37.5% of the participants experienced sexual violence and harassment (Table 2). Also, 57% of the participants desired to preserve fertility (CI: 0.47 - 0.67), and 23% had a bad feeling about self-sex-reassigned (CI: 0.14 - 0.3). In addition, 37% of the participants had perceived discrimination and stigma (CI: 0.27 - 0.47). Moreover, 75% of the participants experienced violence (CI: 0.66 - 0.84). Further, 27% of supporter persons in sex-reassigned just were family (CI: 0.18 - 0.36). Besides, 73% of the participants had an experience of committing suicide (CI: 0.64 - 0.82) and 25% had suicidal ideation (CI: 0.16 - 0.34). Satisfaction of sex-reassigned in sex act time was 12% (CI: 0.05 - 0.19). Sexual satisfaction was described as poor or not satisfactory in 42% of the participants (CI: 0.38 - 0.58). Finally, 76% of the participants perceived no threat of unproductive sex acts (CI: 0.67 - 0.85), and 86% of the participants had a bad feeling about referring to a health center (CI: 0.79 - 0.93) (Table 4).
| Factors Related to High-risk Sexual Behaviors | No. (%) | Results |
|---|---|---|
| Desire to preserve fertility | (0.47 - 0.67) a | |
| Yes | 55 (57) | |
| No | 41 (43) | |
| Feeling to self- sex-reassigned | (0.14 - 0.3) b | |
| Good | 64 (66) | |
| Bad | 22 (23) | |
| Not feeling | 10 (11) | |
| The desire for the gender of the partner | - | |
| Male | 23 (23) | |
| Female | 73 (76) | |
| Perception of discrimination and stigma | (0.27 - 0.47) a | |
| Yes | 36 (37) | |
| No | 60 (63) | |
| Experience of violence | (0.66 - 0.84) a | |
| Yes | 72 (75) | |
| No | 24 (25) | |
| Supporter person in sex-reassigned | (0.18 - 0.36) c | |
| Family | 26 (27.5) | |
| Friend | 33 (34.87) | |
| Others | 37 (38.63) | |
| Committing suicide | (0.64 - 0.82) a | |
| Yes | 71 (73) | |
| No | 25 (27) | |
| Suicidal ideation | (0.16 - 0.34) a | |
| Yes | 24 (25) | |
| No | 72 (75) | |
| Satisfaction of sex-reassigned in sex act time | (0.05 - 0.19) d | |
| Satisfied | 3 (3.1) | |
| Relatively satisfied | 81 (84.4) | |
| Not satisfied | 12 (12.5) | |
| Sexual satisfaction | (0.38 - 0.58) d | |
| Satisfied | 25 (26.1) | |
| Relatively satisfied | 24 (25.05) | |
| Poor satisfied | 28 (29.1) | |
| Not satisfied | 18 (18.75) | |
| The perceived threat of unproductive sex act | (0.67 - 0.85) e | |
| Yes | 23 (23.95) | |
| No | 73 (76.05) | |
| Feeling about referring to the health center | (0.79 - 0.93) b | |
| Good | 7 (7.29) | |
| Bad | 83 (86.45) | |
| Not feeling | 6 (6.26) |
a Answer with yes.
b Answer is bad.
c Supporter persons in sex-reassigned just were family.
d Answer is satisfy.
e Answer with No.
5. Discussion
The mean age of the participants was 28 ± 9.93 years. Results of a study in chili showed that the mean age of MTF transsexual subjects was 31.88 years (17). That study is consistent with the current study. Moreover, 43.75% of individuals had a university education. In a study, 43.7% of participants also had a diploma and academic degree (15). According to present results, taking a Pap smear test was scarce among transgender individuals. A study found a lower prevalence of the Pap smear test in FTM compared to cisgender (non-transgender) individuals (18). That study was in line with the current study. Female-to-male individuals are more likely to have an inadequate Pap test due to a combination of physical changes induced by testosterone therapy and FTM discomfort with the examination (19). It seems that lack of knowledge, lack of access to health centers, lack of belief, self-stigma in transgender people, and discrimination by healthcare providers may be the reasons for this finding. As White Hughto and colleagues also reported, transgender people face suspiciously high rates of discernment, violence, and other forms of stigma (20). However, this requires further studies.
In the present study, the majority of the MTF individuals did not undergo prostate cancer screening. Based on a report Nik-Ahd et al. between males to females, the prostate is retained even after gender-affirmation surgery, thereby needing continuing screening for prostate cancer (21). Male-to-female transgender persons are at risk for prostate cancer. Transgender patients on hormone therapy for gender affirmation may be at risk for both over-grading of prostate cancer and are not recognized (22).
The present results showed that the majority of the individuals did not undergo breast cancer screening. Based on a report by Clarke et al., there are risk factors for breast cancer increase, and a lot of data support breast cancer screening in transgender females and males (23). A systematic study and meta-analysis determined that FTM and MTF individuals were at significantly higher risk of increasing breast cancer in comparison to cisgender males; however, they were at lower risk than cisgender females (24).
The findings of this study indicate that less than 14 years old was the age of sexual debut for 30% of individuals. In a previous study, the youngest age of sexual debut was reported to be 12 years old (25). Additionally, 70 % of individuals reported having more than one sexual partner during their life time. Among the participants, 73% FTM transsexual subjects had female sexual partners. while 23 MTF transsexual subjects had male sexual partners. Furthermore, 30% of individuals reported having casual or paying sexual partners. The results of Herbst et al.'s study were consistent with the findings of the present study. They showed that 31.7% of transgender females had multiple sex partners (26). The study conducted revealed that 73% of the individuals had never used a condom. In this regard, a study found that MTF transsexual people had multiple partners, but FTM transsexual subjects often had steady sexual partners. Moreover, 47.6% of the subjects never used a condom (27). In the present study, the majority of participants had never received HBV and HPV vaccines. Besides, 77% of them were never tested for HIV. Nematollahi et al.’s study is consistent with the present study. They revealed more than 72% of transgender persons never underwent HIV tests (25). In Meites et al.’s study, 83% of the participants received at least one dose of HPV vaccine. They found that education level has been a strong predictor of receiving HPV vaccination (28). Based on the findings of the study, genital warts were more prevalent in men that had sexual intercourse with other men or with transsexual women, 77% of whom had unprotected oral or anal sex in the past six months. Moreover, 52% of them received no information about HPV, or it was incomplete. They believed that condom use prevented HPV, and warts indicated HPV infection in a person. The high price of the HPV vaccine was reported as a barrier to vaccination (29). According to the current study, it appears that insufficient information and limited access to free vaccination are likely key factors contributing to low HPV vaccine uptake.
In the present study, 73% of the individuals reported no symptoms indicating STIs throughout their lifetime. However, our findings are inconsistent with those of two other studies. Their results showed that the prevalence of STIs was between 13 and 21% in transgender females (30, 31). Moreover, one participant suffered from HIV, and two people suffered from STIs, of whom 26% reported unprotected sex with casual partners and alcohol consumption before intercourse (32). In this study, 34.4% of the participants had anal sex. Anal intercourse was the most high-risk sexual behavior according to 23% of the participants because sex acts were without a condom. Moreover, 94% had oral sex, and just 17% of them had vaginal sex, respectively. Study results were consistent with the present study; the majority of transgender participants are sexually active and prefer anal sex (33). The results of a study showed that 57% of transsexual subjects had bisexual tendencies, and 30% of MTF transsexual subjects had sex with non-transsexual males in the past three months (34). In the present study, 70% of the subjects believed that the chances of transmission are lower in anal sex than vaginal sex. A previous study was consonant with our findings, which found that 70% of transsexual subjects believed that a healthy person might appear to be HIV-positive. Therefore, they can be considered potential HIV transmission routes (32).
The current study found that 37.5% of the participants reported experiencing sexual violence and harassment. These findings are congruent with the results of Johns et al.'s study. They showed that the prevalence of all experiences of violence and discrimination was higher among transgender persons, including 23.8% forced to have sexual intercourse and 26.4% physical violence (35).
This is a cross-sectional survey in which causality cannot be concluded from the findings. It is necessary to carry out a qualitative study to find reasons for not referring to screening from deep layers of anecdotes and experiences of FTM and MTF. A strong point of this study was the research environment, which was the largest center for all transsexual people from the whole country. Moreover, the sample represented the transsexual population. However, this study had a limitation, including transsexual people who have not been referred to the clinic for their status so far.
5.1. Conclusions
High-risk behaviors are common in transsexual participants. It can be recommended that establishing specialized health centers are needed for transsexual subjects. Also, healthcare providers should offer services without stigma and discrimination. It may be prevented or reduce high-risk sexual behaviors and substance abuse outcomes.