1. Background
Emotional disorders are common and recurring mental conditions that can severely affect individuals and have long-term economic consequences for society. Historically, anxiety disorders and depression have been categorized as emotional disorders, likely due to the high comorbidity observed among different mental disorders, particularly anxiety disorders and depression. Individuals with a history of significant depression and anxiety disorders have reported a lifetime prevalence of anxiety and depression at approximately 57% and 81%, respectively. Several reasons have been proposed to explain this comorbidity in psychopathology (1-5). Patients experiencing both anxiety disorders and depression tend to exhibit more severe symptoms, more frequent episodes of major depression, and a higher risk of suicidal ideation (6).
Emotional regulation is a fundamental concept in the development and nature of emotional disorders. It refers to how individuals manage their emotions, including how they experience and express their feelings (7). Effective emotional regulation and addressing dysregulation are crucial objectives in psychological treatments, as they play a significant role in the persistence of emotional disorders (8). Emotion regulation is among the most influential factors impacting individuals’ mental well-being (9). The difficulty in emotion regulation is characterized by challenges in recognizing, understanding, and accepting emotions, as well as a lack of adaptive strategies to cope with different emotional experiences or difficulties in controlling behavior during intense emotional states (10).
Based on the process model of emotion regulation, reappraisal and suppression are two distinct methods of regulating emotions that fall under various strategies of emotion regulation, each with its focus on the outcome and response. These strategies are associated with diverse emotional consequences (7).
Some researchers posit that experiential avoidance (EA) can be considered a unique form of emotion regulation (11). Engaging in avoidance of negative internal experiences may provide short-term relief from distress, but this approach has paradoxical effects over time and can exacerbate distress in individuals (12).
Experiential avoidance is associated with suicidal ideation (13), non-suicidal self-injury behaviors (14), and factors that contribute to self-harming behaviors, including emotional disorders (15). Additionally, EA can serve as a mediating factor in the relationship between psychological constructs and depressive disorder (16). As a relevant transdiagnostic factor, EA has been extensively studied for its impact on the development and progression of comorbid emotional disorders (17).
Although issues in emotion regulation and maladaptive strategies for regulating emotions contribute to emotional disorders, personality traits, such as neuroticism, may also have a pivotal role in the onset and perpetuation of emotional disorders (18, 19).
Neuroticism is a personality trait characterized by a tendency toward worry, anxiety, and negative emotions, and it has implications for a wide range of psychopathological and physical concerns (20, 21). Previous research has indicated that neuroticism is associated with deficits in emotion regulation (22, 23), and the problem of emotional regulation partially mediates the relationship between neuroticism and the presence of anxiety and depression symptoms. However, further studies are needed to confirm these findings (24). High levels of neuroticism have been linked to poor emotional regulation and emotional well-being (25). Different conceptualizations of neuroticism emphasize negative affectivity (the tendency to experience distressing emotions) or cognitive aspects such as worry or rumination (26).
Moreover, neuroticism is associated with EA (24) and negative repetitive thoughts. Negative repetitive thoughts generally encompass an individual’s tendency to dwell on problems and negatively experience them. This pattern of thinking first causes distress for the person; secondly, it becomes repetitive, and finally, it becomes challenging for the individual to break free from these thoughts (27). Negative repetitive thoughts include worry, rumination, threat monitoring, and other types of negative repetitive thinking that are central to anxiety and depression disorders (28), and they play a crucial role in the development and progression of symptoms related to emotional disorders (29). Research indicates that repetitive negative thoughts are associated with difficulties in emotion regulation (30) and experiential avoidance (31) and also act as mediators in prospective cross-disorder associations between anxiety and depression disorders and their symptoms (32).
However, no study has yet examined the relationship between the components of emotional regulation, EA, negative repetitive thoughts, and neuroticism through a structural equation model to comprehend their interplay in the clinical population with emotional disorders.
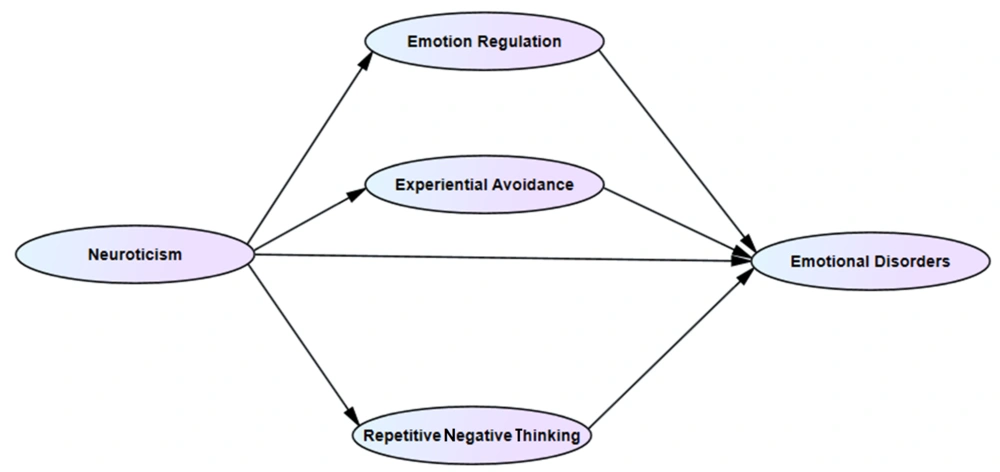
Given this gap in the literature and the significant prevalence of emotional disorders and their detrimental impact on individuals, families, and society, this study aims to propose and test a hypothetical model using structural equation modeling. The aim is to elucidate the specific roles of each predictor variable in relation to one another and emotional disorders more precisely. A comprehensive model can inform more effective treatments and contribute to future research by elucidating the underlying mechanisms of emotional disorders (Figure 1).
2. Objectives
This study aimed to predict emotional disorders in patients diagnosed with emotional disorders, using neuroticism, emotion regulation, EA, and repetitive negative thinking as predictors.
3. Patients and Methods
3.1. Participants
The current cross-sectional study conducted in Tehran (Iran). The population of interest comprises individuals residing in Tehran (Iran) diagnosed with emotional disorders.
These individuals encompass all clients who sought services at Shahid Beheshti University of Medical Sciences hospitals, as well as psychological and psychiatric clinics in Tehran from 2021 to 2022.
These individuals present with a variety of mood disorders, anxiety disorders, eating disorders, somatic disorders, dissociative disorders, trauma spectrum disorders, and obsessions, as outlined in the DSM-5.
The researchers employed an available sampling method. Sample size calculation was performed using Free Statistics Calculators software, taking into account an effect size of 0.03, power of 0.95, five latent variables, 180 observable variables, and a desired alpha level of 0.5, which resulted in a recommended sample size of 245.
The inclusion criteria for the study comprised individuals with a documented diagnosis of emotional disorders in their psychological files, based on DSM-5 criteria, assessed using Structural Clinical Interview for DSM-5-Research Version (SCID-5-RV) and Structured Clinical Interview for DSM-5 Personality Disorders (SCID-5-PD). Exclusion criteria encompassed severe psychiatric disorders, such as psychotic disorders, substance abuse or dependence, personality disorders, age below 18 years, education level below at least the third year of middle school, and lack of informed consent for participating in the research.
Exclusion criteria encompassed incomplete questionnaires, partial questionnaire completion, and random responses on the answer sheet (including the inclusion of a deviant question in the middle of each questionnaire, instructing participants to select “I know” in the “I agree” option).
3.2. Measurements
3.2.1. The Structural Clinical Interview for DSM-5-Research Version (SCID-5-RV)
The validity and reliability of the original version have been established through numerous studies (33). Moreover, a validity and reliability study of the Persian version of SCID-5 conducted on an Iranian sample demonstrated good internal consistency (0.95 - 0.99), test-retest reliability (0.60 - 0.79), and kappa reliability (0.57 - 0.72) (34).
3.2.2. The Structured Clinical Interview for DSM-5 Personality Disorders (SCID-5-PD)
This instrument is a semi-structured diagnostic clinical interview designed to assess DSM-5 personality disorders within clusters A, B, and C. The questionnaire comprises 106 questions and can be completed in under 20 minutes. A minimum education level of eight classes is required to answer the questions. The interviewer guides the interview based on the patient’s positive responses. A study conducted in Iran examined the psychometric properties of the Persian version of SCID-5-PD, confirming its validity and reliability within the Iranian population. Kappa coefficients exceeded 0.4 for diagnoses related to borderline, narcissistic, antisocial, paranoid, schizotypal, dramatic, and obsessive-compulsive personality disorders. Kappa coefficients were below 0.4 for diagnoses associated with dependent, avoidant, and other specific disorders. The highest agreement, with a Kappa value of 0.839, was observed between two psychiatrist reports and the SCID interviewer about borderline personality disorder (35).
3.2.3. Difficulties in Emotion Regulation Scale (DERS)
This scale, initially developed by Gratz and Roemer, assesses self-reported difficulties in emotional regulation (10). The scale consists of 41 questions designed to evaluate clinical and emotional aspects based on a 5-point Likert scale. After factor analysis, the authors removed five items from the original scale, resulting in a total of 36 items (10). The factor analysis revealed six factors: Non-acceptance of emotional responses, difficulties with goal-directed behavior, problems with impulse control, lack of emotional awareness, limited access to emotion regulation strategies, and lack of emotional clarity. The overall internal reliability of the scale was found to be 0.93, with individual subscales demonstrating reliabilities of 0.85, 0.89, 0.86, 0.80, 0.88, and 0.84, respectively. The scale exhibited significant correlations with the acceptance and commitment scale, further supporting its validity (18). Cronbach’s alpha coefficient was used to examine and confirm the internal consistency reliability of the instrument, which yielded a value of α = 0.86. The reliability of the scale was also confirmed in the Iranian sample (36).
3.2.4. Negative Repetitive Thoughts Questionnaire (NRTQ)
This 31-item scale assesses negative repetitive thoughts using a five-point Likert scale. The scale demonstrates good internal consistency with Cronbach’s alpha coefficients ranging from 0.72 to 0.93. To evaluate the predictive validity and correlation of the scale, Beck’s depression and anxiety questionnaire was utilized, resulting in correlation coefficients of 0.42 and 0.38, respectively. The Persian version of the scale exhibits a reliability coefficient of 0.89 (37).
3.2.5. Experiential Avoidance Questionnaire (EAQ)
This 32-item tool, originally developed by Hayes et al. (12), is the latest version used in the current study. It consists of ten questions rated on a seven-point Likert scale (ranging from never = 1 to always = 7). Previous research reported a single-factor structure for this scale, with a Cronbach’s alpha coefficient of 0.84. The questionnaire’s reliability was evaluated in Iran, resulting in a Cronbach’s alpha of 0.82. Correlation coefficients with the Beck’s depression and anxiety questionnaire and the emotional disorder scale were measured at 0.44, 0.59, and 0.59, respectively. Furthermore, factor analysis demonstrated appropriate factor loadings for the items (38).
3.2.6. Inventory of Depression and Anxiety Symptoms (IDAS)
To assess symptoms of emotional disorders, the Symptoms of Depression and Anxiety Disorders questionnaire developed by Watson et al. was utilized (39). This questionnaire consists of 64 items that evaluate 11 factors related to anxiety and depression. These factors include lethargy, insomnia, suicidal thoughts, weight gain, weight loss, boredom, well-being, morbid mood, panic, social anxiety, and automatic thoughts (39). Each item is scored on a five-point Likert scale, ranging from never (1) to always (5). A score of one is assigned to a “never” response, while a score of five is given for an “always” response. The alpha values for each subscale exceed 0.80 (40). It is important to note that the well-being subscale is scored in reverse. In an Iranian study, the questionnaire demonstrated an alpha value of 0.95 (29).
3.2.7. NEO Personality Questionnaire (NEO FFI)
This questionnaire comprises 60 questions, with each set of 12 questions measuring one of the five factors: neuroticism, extraversion, openness to experience, conscientiousness, and sociability. Each question is rated on a 1 - 5 Likert scale. The short form of the questionnaire demonstrates a correlation of 0.68 with the long form and exhibits good internal reliability. Numerous studies conducted in Iran have reported satisfactory internal reliability and validity for the questionnaire’s subscales. For instance, a study by Nilforooshan et al. (41) involving Isfahan couples indicated acceptable and good reliability and validity. The Cronbach’s alpha values for neuroticism, extraversion, openness to experience, conscientiousness, and sociability were 0.76, 0.63, 0.31, 0.48, and 0.81, respectively.
3.3. Procedure
After conducting a thorough case study and initial interview conducted by clinical psychologists, the purpose of the research was explained to the patients. The subjects were individually assessed in a quiet room. Following a face-to-face interview and utilizing the structured clinical interviews for SCID-5-RV and SCID-5-PD and considering the inclusion and exclusion criteria, the participants were provided with instructions on completing the questionnaires. Subsequently, the subjects were assessed using the Emotional Regulation Scale, Negative Repetitive Thoughts Scale, Short Form of the NEO Personality Questionnaire, Experimental Avoidance Questionnaire, and Psychological Symptoms Assessment.
3.4. Data Analysis
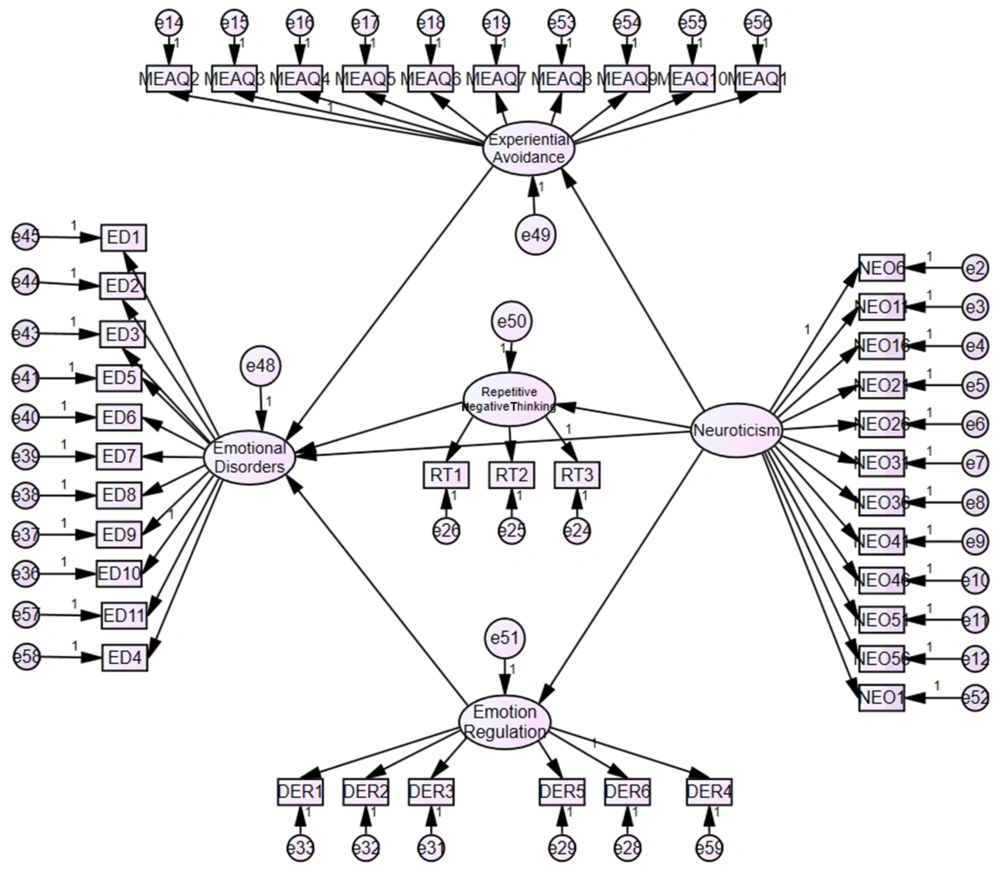
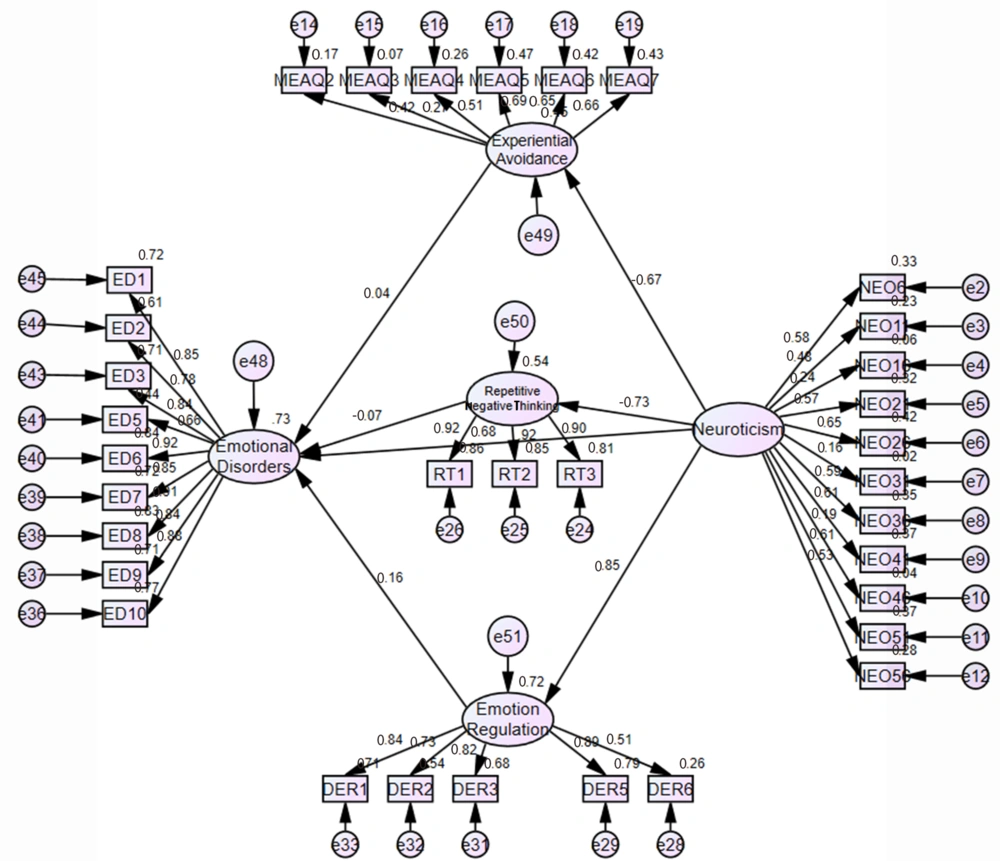
The data collected in this study were analyzed using descriptive statistics such as frequency, mean, standard deviation, and percentage, as well as inferential methods, including multiple regression analysis, with the assistance of SPSS-22 software. Structural equation modeling tests were performed using both SPSS-22 and AMOS-24 software. For the utilization of structural equation modeling, the initial model of the research was first developed in the AMOS22 software environment (Figure 2). Subsequently, the initial model was tested, and the fit indices for the initial model were calculated (comparative fit index (CFI) = 0.82, Tucker-Lewis fit index (TLI) = 0.81). These values indicate that the fit of the initial research model does not fall within the acceptable range, suggesting that the initial model does not have an acceptable fit (0.90 > 0.90, CFI > TLI). Therefore, in the next step, the path coefficients of the items were examined to achieve acceptable fit indices. Items with factor loadings below 0.4 were removed from the research process, leading to modifications in the initial model. The modified model is illustrated in Figure 3.
4. Results
In this study, a total of 414 questionnaires were collected. The demographic characteristics of the participants are presented in Table 1. The table reveals that 91.5% of the participants fall within the age range of 18 to 37 years, while 8.5% are between 38 and 58 years. Regarding gender distribution, 44.7% are female, and 55.3% are male. Regarding marital status, 74.9% are single, 24.6% are married, and 0.5% are divorced. Education-wise, 36.7% have a diploma degree, 48.1% have a bachelor’s degree, 8% have a master’s degree, 5.8% have a Ph.D., and 1.4% have an MD. Furthermore, 13.3% are single children, 34.1% are the first child, 26.6% are the middle child, and 26.1% are the last child in their respective families. A summary of the socio-demographic data can be found in Table 1.
| Variables | No. (%) |
|---|---|
| Gender | |
| Male | 229 (55.3) |
| Female | 185 (44.7) |
| Marital status | |
| Single | 310 (47.9) |
| Married | 102 (24.6) |
| Divorced or widow | 2 (0.5) |
| Education | |
| Diploma | 152 (36.7) |
| Bachelor | 199 (48.1) |
| Master | 33 (8) |
| Ph.D. | 24 (5.8) |
| M.D. | 6 (1.4) |
| Age | |
| 18 - 37 | 388 (91.5) |
| 38 - 58 | 26 (8.5) |
| Birth order | |
| Single child | 55 (13.3) |
| The first child of the family | 141 (34.1) |
| The middle child of the family | 110 (26.6) |
| The last child of the family | 108 (26.1) |
Socio-demographic Characteristics of Participants (n = 414)
4.1. Data Analysis
Data analysis and hypothesis testing were conducted using structural equation modeling with the AMOS22 software. Descriptive statistics for the research variables (neuroticism, emotional regulation, negative thoughts, EA, and emotional disorders) are presented in Table 2.
| Variable | Minimum | Maximum | Mean ± Standard Deviation | Skewness | Kurtosis |
|---|---|---|---|---|---|
| Neuroticism | 0 | 38 | 20.98 ± 7.81 | -0.37 | -0.61 |
| Emotion regulation | 53 | 178 | 107.71 ± 20.57 | 0.23 | 1.13 |
| negative thoughts | 31 | 155 | 105.67 ± 21.4 | -0.33 | -0.03 |
| EA | 10 | 66 | 40.92 ± 7.8 | 0.15 | 0.72 |
| Emotional disorders | 56 | 280 | 161.92 ± 44.41 | 0.14 | -0.37 |
Results Related to the Descriptive Statistics of Research Variables
Table 2 displays the mean and standard deviation values for the variables in the study. The neuroticism variable has a mean of 20.98 and a standard deviation of 7.81. Emotional regulation has a mean of 107.71 and a standard deviation of 20.57. Negative thoughts have a mean of 105.67 and a standard deviation of 21.4. EA has a mean of 40.92 and a standard deviation of 7.8. Lastly, emotional disorders have a mean of 161.92 and a standard deviation of 44.41.
To assess the normality of the data, skewness and kurtosis values were calculated for the research variables. Table 2 indicates that the skewness and kurtosis values for all variables (neuroticism, emotional regulation, negative thoughts, EA, and emotional disorders) fall between +2 and -2. This confirms the normality of the data (42).
The reliability coefficient for the research variables (neuroticism, emotional regulation, negative thoughts, experimental avoidance, and emotional disorders) was calculated using Cronbach’s alpha. The results of Cronbach’s alpha can be found in Table 3. Table 3 displays Cronbach’s alpha values of 0.76, 0.87, 0.95, 0.65, and 0.97 for neuroticism, emotional regulation, negative thoughts, EA, and emotional disorders, respectively.
| Variable | Neuroticism | Emotional Regulation | Negative Thoughts | EA | Emotional Disorders |
|---|---|---|---|---|---|
| Cronbach’s alpha | 0.76 | 0.87 | 0.95 | 0.65 | 0.97 |
Cronbach’s Alpha Reliability Coefficient
4.2. Conceptual Model of Research
To utilize structural equation modeling, the initial conceptual model of the research was created within the AMOS22 software environment (Figure 2). Subsequently, the initial model was adjusted to achieve improved fit indices. The adjusted model is depicted in Figure 3. Table 4 displays the goodness-of-fit indices for the modified research model. The table reveals that the root mean square error of estimation (RMSEA) is 0.06 (RMSEA < 0.08), CFI is 0.90, TLI is 0.89, and the parsimonious fit value (CMIN/DF) is approximately 2.67 (CMIN/DF > 5). The fit indices indicate that the model fits well within an acceptable range. Therefore, the modified model demonstrates a good fit, enabling the examination of research hypotheses. Table 5 presents the regression weights of the modified model based on the studied variables.
| Index | RMSEA | CFI | TLI | CMIN/DF |
|---|---|---|---|---|
| Optimal range | RMSEA ≤ 0.08 | CFI ≥ 0.9 | TLI ≥ 0.9 | CMIN/DF > 5 |
| Value | 0.06 | 0.90 | 0.89 | 2.67 |
Indices of the Modified Research Model
| Path | Estimate | C.R. | P Value |
|---|---|---|---|
| Neuroticism→ emotional regulation | 2.21 | 8.26 | 0.001 |
| Neuroticism → EA | -0.64 | -6.38 | 0.001 |
| Neuroticism → emotional disorders | 3.17 | 5.36 | 0.001 |
| Neuroticism → repetitive negative thoughts | -8.48 | -10.69 | 0.001 |
| Emotional regulation → emotional disorders | 0.28 | 1.85 | 0.06 |
| Repetitive negative thoughts → emotional disorders | -0.03 | -1.38 | 0.17 |
| EA → emotional disorders | 0.17 | 0.63 | 0.52 |
Regression Weights of an Emotional Disorders Prediction Model Based on Neuroticism with Emotional Regulation, Experiential Avoidance, and Repetitive Negative Thoughts
Table 5 presents the following results:
The significance level of the effect of neuroticism on emotional regulation is less than 0.001 (P < 0.001), confirming the first hypothesis that “neuroticism affects emotional regulation.” The significance level of the effect of neuroticism on EA is less than 0.001 (P < 0.001), confirming the second hypothesis that “neuroticism affects EA.” The significance level of the effect of neuroticism on emotional disorders is less than 0.001 (P < 0.001), confirming the third hypothesis that “neuroticism affects emotional disorders.” The significance level of the effect of neuroticism on repetitive negative thoughts is less than 0.001 (P < 0.001), confirming the fourth hypothesis that “neuroticism affects repetitive negative thoughts.” The significance level of the effect of emotional regulation on emotional disorders is 0.06, indicating that the fifth hypothesis that “emotional regulation affects emotional disorders” was not accepted (P > 0.05). The sixth hypothesis, which states that “repetitive negative thoughts affect emotional disorders,” was not supported (P > 0.05) as the significance level of the effect of repetitive negative thoughts on emotional disorders was found to be 0.17. Similarly, the seventh hypothesis proposing that “EA affects emotional disorders” was not supported (P > 0.05), as the significance level of the effect of EA on emotional disorders was found to be 0.52. Regarding the eighth hypothesis, suggesting that emotional regulation plays a mediating role between neuroticism and emotional disorders, it was not supported. The significance level of the effect of neuroticism on emotional regulation was less than 0.001, but the effect of emotional regulation on emotional disorders was not statistically significant (P = 0.06). Similarly, the ninth hypothesis proposing that experiential avoidance plays a mediating role between neuroticism and emotional disorders was not supported. While the effect of neuroticism on EA was highly significant (P < 0.001), the effect of EA on emotional disorders was not statistically significant (P = 0.52). The significance level for the effect of neuroticism on repetitive negative thoughts is less than 0.001, while the significance level for the effect of repetitive negative thoughts on emotional disorders is 0.17. Therefore, the tenth hypothesis was not accepted, stating that repetitive negative thoughts mediate between neuroticism and emotional disorders.
The coefficient of determination for emotional disorders was calculated as 0.73, indicating that 73% of the variability in emotional disorders can be explained by predictor variables such as neuroticism, emotional regulation, negative repetitive thoughts, and EA. This suggests a robust research model for predicting emotional disorders using these variables (43).
5. Discussion
According to the hypothesis, neuroticism is directly associated with negative emotional regulation. The results of this study revealed that neuroticism contributes to the development of negative emotional regulation. Increased neuroticism has detrimental effects on emotional regulation. This finding aligns with previous research conducted by Singh (44) and Mohammadkhani et al. (24). The hypothesis suggests that neuroticism is inversely related to the use of cognitive reappraisal strategies, a form of emotion regulation. Individuals with lower levels of neuroticism were more effective at regulating negative emotions due to their tendency to employ cognitive reappraisal strategies. Consequently, they experienced fewer negative emotions. Conversely, individuals with high levels of neuroticism exhibited poor emotional regulation and unfavorable emotional states (25). The neuroticism scale encompasses a broad range of negative emotions, including fear, sadness, arousal, anger, guilt, and boredom. Overall, neuroticism involves more factors than susceptibility to psychological distress, as it can impact an individual’s adaptation to personal and environmental circumstances.
Consistent with prior studies, this study established a significant association between neuroticism and EA. This finding aligns with the research findings of Spinhoven et al. (16). Individuals exhibiting traits such as nervousness, anxiety, worry, moodiness, incompetence, uncertainty, instability, unhappiness, irritability, and high sensitivity tend to engage in situational avoidance or escape when faced with unwanted experiences. The cycle of anxiety and worry perpetuates increased neuroticism and EA toward unpleasant situations. Additionally, individuals suffering from various mood disorders often experience physical and mental distress, leading to anxiety and unhealthy communication patterns with their physical and social environment. This can result in neglect of others and impulsiveness. Such detrimental behavioral patterns contribute to biased interpretation of events, heightened attention to internal and external stimuli, and the development of inappropriate judgments and perceptions. Biased attitudes foster a problematic cycle of avoidance and escape (EA), as well as irritability and uncertainty (neuroticism). Conversely, individuals with lower scores on the neuroticism index demonstrate emotional stability, exhibiting calmness, an even mood, and the ability to cope effectively with stressful situations without confusion or behavioral issues (45).
Another significant finding of the current study was the strong relationship between neuroticism and emotional disorders. The effect of neuroticism on emotional disorders had a significance level of less than 0.001 (P < 0.001), confirming the hypothesis that neuroticism influences emotional disorders. This finding aligns with the research conducted by Zemestani et al. (46) and Tonarely et al. (47). To explain this result, it can be stated that individuals who exhibit negative cognitive styles such as self-blame, rumination, catastrophizing, and blaming others are more susceptible to emotional problems compared to others (48). Gross and Thompson (49) argue that it is logical to expect emotional disorders in individuals with high scores in the neuroticism dimension. Moreover, increasing evidence highlights the impact of emotional disorders on physical health, particularly considering the role of anger, anxiety, and depression in the context of physical disorders (49).
Surprisingly, the results revealed no significant relationship between EA and emotional disorders. The effect of EA on emotional disorders had a significance level of 0.52, indicating that the hypothesis stating “EA affects emotional disorders” was not supported (P < 0.05). Notably, this finding differs from the results reported by Hajishabani and Abdi (15). Previous research led to the expectation that avoidance would significantly contribute to emotional disorders, including anxiety and depression. It was anticipated that individuals displaying higher levels of EA would be more prone to experiencing symptoms of depression and anxiety (17). This expectation stemmed from the understanding that EA extends beyond being merely a secondary symptom of emotional disorders; instead, it is conceptualized as a transdiagnostic factor influencing the development and course of emotional disorders (17).
The current study unexpectedly found no significant relationship between negative emotional regulation and emotional disorders. This means that emotional regulation does not act as a mediating factor between neuroticism and emotional disorders. The significance level of the effect of emotional regulation on emotional disorders was 0.06, indicating that the hypothesis stating “emotional regulation affects emotional disorders” was not supported (P < 0.05). This finding contradicts the research results of Saadat et al. (50) and Ong and Thompson (51) regarding the role of emotion regulation strategies in clinical disorders and problems. It was anticipated that emotional regulation would significantly impact emotional disorders.
Contrary to our expectations, the association between EA and emotional disorders was not as strong as anticipated. One potential explanation for these findings is that individuals with emotional disorders do not consistently respond to negative emotions, suggesting the involvement of additional psychological and cultural mechanisms in this relationship.
Another significant finding of the current study was the strong relationship between neuroticism and negative repetitive thoughts. The effect of neuroticism on repetitive negative thoughts had a significance level of less than 0.001 (P < 0.001), confirming the hypothesis that neuroticism influences repetitive negative thoughts. This finding aligns with the research conducted by Toulabi et al. (52). Additionally, Roshandel Hesari et al. (53) examined personality traits, stress, and religious beliefs among individuals who have committed suicide and found that they exhibited higher levels of introversion, neuroticism, and psychotic traits compared to the control group. Furthermore, Joorbonyan et al. (29) investigated negative repetitive thoughts and concluded that these thoughts are significant predictors of emotional disorders.
This research was conducted as a cross-sectional study, which means that definitive conclusions about the causation of emotional disorders by neuroticism cannot be made. Therefore, further detailed analysis is necessary to obtain more accurate findings. The study sample consisted of individuals with various types of illnesses who sought treatment at Shahid Beheshti University of Medical Sciences hospitals and psychology and psychiatry clinics in Tehran during 2021 - 2022, which may limit the generalizability of the findings to other populations. The research employed self-report measures, so caution should be exercised when generalizing the results. It is important to note that the study solely focused on individuals with emotional disorders; thus, the findings may not be generalized with high certainty. Considering the influential role of personality and psychological factors in susceptibility to disorders, attention to these factors is crucial. The results of this study offer a valuable guideline for the development of prevention and treatment programs for emotional disorders, emphasizing an integrated, culturally sensitive, contextual, and psychosocial approach. It is recommended to conduct similar research on larger and more diverse samples in different societies to test the replicability and generalizability of the current study.
5.1. Conclusions
Based on the research findings, it was determined that neuroticism has an impact on emotional regulation, emotional disorders, and negative repetitive thoughts. Therefore, it is crucial to consider the influence of personality and psychological factors on disease susceptibility. Given psychologists’ expertise in diagnosing and addressing psychological and personality issues, incorporating psychological counseling into medical treatments should be prioritized.
Numerous studies have examined the shared factors involved in the development and persistence of emotional disorders and have attempted to establish connections among these factors. However, further investigation is required to enhance the assessment and psychotherapy domains, aiming for a more direct, cost-effective, and efficient tool to evaluate and address emotions and associated disorders using relevant underlying factors.