1. Background
Nonsuicidal self-injury (NSSI) is defined as intentional injury to body tissue that occurs in the absence of suicidal intent (1). These behaviors were classified as a condition requiring further study as NSSI to include in the Fifth Edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) (2). According to a large systematic review, approximately 4% - 23% of adults worldwide report at least a single episode of NSSI during their lifetime (3, 4). Nonsuicidal self-injury is associated with various psychiatric disorders and an elevated risk of suicidal behavior (5). To date, there is no universally agreed-upon best practice for the treatment of NSSI (6). A recent systematic review revealed that there are effective treatments (eg, dialectical behavior therapy) that include or can be expanded to include the treatment of NSSI. However, these approaches were not primarily developed for, nor specifically focused on, NSSI (ie, borderline personality disorder) (7, 8). Additionally, a number of psychosocial treatments (eg, cutting down programs) has been specifically developed to focus on NSSI (8, 9). Currently, there are few evidence-based interventions targeting NSSI in adults. This highlights the need for interventions that either target a set of factors common among those with NSSI, target a unique potential mechanism for NSSI, or consider the ability to better tailor interventions to each individual's presentation (9).
In recent years, transcranial direct current stimulation (tDCS) has shown promise in treating self-injury (10). For example, tDCS can be used to target stimulation of the dorsolateral prefrontal cortex (DLPFC), a key region implicated in adaptive emotion regulation and cognitive control (11). Specifically, several studies assessing neurocognitive indices of impulsivity have shown this construct to be associated with NSSI (12, 13). However, none of these studies have investigated individuals with NSSI.
The National Institute of Mental Health (NIMH) introduced the Research Domain Criteria (RDoC) in 2009 as a new approach to understanding psychopathology based on empirical findings. The RDoC framework aims to provide a comprehensive understanding of psychopathology and its mechanisms, which could lead to reliable diagnoses and evidence-based interventions (14). This approach focuses on domains of function and basic mechanisms instead of symptom clusters, which may lead to a better understanding of psychopathology and better interventions (15). Research shows that atypical biological functioning is associated with NSSI (16), and treatment development requires a better understanding of its neurobiological mechanisms (13). This study aims to bring together existing findings from neurobiological NSSI research and identify potential intervention strategies by examining previous systematic reviews. By examining previous systematic reviews (13, 16-20), we organized them based on RDoC constructs of negative valence systems, positive valence systems, cognitive systems, and social processes systems.
2. Objectives
Despite being a significant issue in clinical settings, there is a lack of effective, evidence-based, and affordable treatment options for NSSI. The objective of this study was to assess the efficacy of the transdiagnostic therapy based on the RDoC framework (TTB-RDoC) compared to tDCS and treatment as usual (TAU) within a randomized controlled trial (RCT).
3. Methods
3.1. Sample and Study Design
This study is a parallel-group RCT designed to investigate the efficacy of TTB-RDoC, TAU, and tDCS for NSSI in Iranian males from May 2021 to August 2022. Participants were randomly assigned to 3 groups: TTB-RDoC (n = 24), TAU (n = 22), or tDCS (n = 22). Assessments were conducted at baseline (pre-treatment), after 8 weeks (post-treatment), and following a 12-month post-treatment follow-up period. To determine sample size, we used G*Power with a significance level of 0.05, a power of 90%, and an effect size of 0.35, resulting in a requirement of 65 participants. Inclusion criteria were a primary DSM-5 diagnosis of NSSI, absence of medication usage, age between 18 and 30, fluency in speaking Persian, and the ability to participate in all assessment and treatment sessions. Exclusion criteria were the need for immediate medical treatment, receiving a full course of pharmacotherapy or psychotherapy within the past 5 years, presence of psychiatric disorders and substance abuse (excluding tobacco users), and history of neurological conditions or brain surgery.
TTB-RDoC is a group intervention program for adults with NSSI. It consists of 16 sessions conducted twice a week, each lasting 45 minutes. The program is divided into 4 modules: Module 1 focuses on emotion regulation, module 2 on cognitive training, module 3 on behavioral activation, and module 4 on interpersonal skills.
For tDCS administration, two 5 × 7-cm electrodes were used. Electrodes were placed using a bipolar-balanced montage with the anode positioned on the right DLPFC at location F4 and the cathode on the left DLPFC at location F3, according to the EEG 10 - 20 system. The tDCS sessions were conducted daily, lasting 20 minutes, 5 days a week for 4 consecutive weeks. These sessions took place during the final 4 weeks of TTB-RDoC treatment. Active stimulation delivered a direct current at an intensity of 2 mA (current density of 0.06 mA/cm2) with a 20-second ramp-up and ramp-down of current. In the TAU group, a practical and accessible treatment program based on cognitive behavior therapy (CBT) principles for young people who had self-injurious behaviors was used within 15 sessions.
3.2. Diagnostic Screening Measure and Outcome Measures
A demographic questionnaire, structured clinical interview for DSM‐5 disorders-clinician version (SCID‐5‐CV) (21), and Inventory of Statements About Self-injury (ISAS) (1) was used to assess the severity and frequency of NSSI and conduct a diagnostic screening.
The RDoC constructs and outcome measures were evaluated using the Anxiety Sensitivity Index (ASI) (22), Snaith-Hamilton Pleasure Scale (SHAPS) (23), Distress Tolerance Scale (DTS) (24), Difficulties in Emotional Regulation Scale (DERS) (25), UPPS-P Impulsive Behavior Scale (UPPS-P) (26), Behavioral Activation, Behavioral Inhibition, and Frustrative Nonreward Responsiveness Scale (BIS/BAS/FNR Scale) (27), Wisconsin Card Sorting Test (WCST-64) (28), Emotional Stroop Test-Suicide Behavior Version SB (EST-SB) (29), Affective Go/No-Go (30), and Adult Rejection Sensitivity Questionnaire (A-RSQ) (31). All measures have shown acceptable psychometric properties.
4. Results
Demographic information of the participants is presented in Table 1. There were no significant differences between the groups in terms of demographic variables. Descriptive statistics of research variables are displayed in Table 2.
| Sociodemographic Variables | tDCS (n = 22) | TAU (n = 22) | TTB-RDoC (n = 24) | P-Value |
|---|---|---|---|---|
| Gender | ||||
| Males | 22 (100) | 22 (100) | 24 (100) | |
| Age | 21.9 ± 2.9 | 22.09 ± 3.2 | 21.7 ± 2.8 | 0.908 |
| Marital status | 0.461 | |||
| Single | 18 (81.8) | 17 (77.2) | 23 (95.8) | |
| Married | 3 (13.6) | 4 (18.1) | 1 (4.1) | |
| Separated/divorced | 1 (4.5) | 1 (4.5) | 0 | |
| Educational level | 0.105 | |||
| Middle/high school | 4 (18.1) | 2 (9) | 9 (37.5) | |
| Diploma | 12 (54.4) | 17 (77.2) | 11 (45.8) | |
| License | 4 (18.1) | 1 (4.5) | 4 (16.6) | |
| Master's | 2 (9) | 2 (9) | 0 | |
| Work status | 0.529 | |||
| Unemployed without allowance | 6 (27.2) | 5 (22.7) | 9 (37.5) | |
| Paid employment | 1 (4.5) | 2 (9) | 0 | |
| Student | 14 (63.6) | 15 (68.1) | 14 (58.3) | |
| Homemaker | 0 | 0 | 1 (4.1) | |
| ISAS behavior | 0.921 | |||
| History of self-injury in the last year | 11.7 ± 4 | 11.6 ± 3.4 | 11.4 ± 2.7 |
Demographic Information a
| Measures | tDCS (n = 22) | TAU (n = 22) | TTB-RDoC (n = 24) | |||
|---|---|---|---|---|---|---|
| Pre | Post | Pre | Post | Pre | Post | |
| NSSI, follow-up | 6.59 ± 1.1 | (1.45 ± 0.85) - (5.31 ± 1.04) | 6.63 ± 1.1 | (0.50 ± 0.67) - (1.36 ± 1.1) | 6.54 ± 1.2 | (1.2 ± 0.99) - (0.79 ± 0.77) |
| ASI | 29.6 ± 3.6 | 24.6 ± 1.6 | 28.7 ± 3.4 | 13.5 ± 3.8 | 30.08 ± 3.7 | 12.4 ± 3.5 |
| SHAPS | 21.7 ± 2.9 | 23.6 ± 1.7 | 21.6 ± 2.9 | 30.2 ± 2.3 | 22.4 ± 2.7 | 30.8 ± 2.3 |
| DTS | 48.8 ± 7.8 | 44.09 ± 6.3 | 49.4 ± 7.4 | 29.5 ± 7.2 | 48.08 ± 7.7 | 25.3 ± 6.5 |
| DERS | 100.5 ± 19.8 | 97.4 ± 11.2 | 101.3 ± 19.6 | 65.8 ± 10.3 | 97 ± 17.9 | 60.2 ± 10.04 |
| UPPS-P | ||||||
| Negative urgency | 9.45 ± 1.2 | 8.90 ± 0.92 | 9.4 ± 1.18 | 7.9 ± 0.92 | 9.1 ± 1.3 | 7.7 ± 0.75 |
| Positive urgency | 9.2 ± 1.4 | 9.2 ± 0.86 | 9.4 ± 1.05 | 7.8 ± 0.85 | 9.7 ± 1.03 | 7.7 ± 0.77 |
| FNR | 10.4 ± 2.2 | 10.45 ± 1.8 | 10.5 ± 2.01 | 13.9 ± 2.03 | 9.7 ± 2.2 | 14.5 ± 2.2 |
| WCST | ||||||
| Number of completed | 1.95 ± 0.99 | 2.09 ± 0.92 | 2 ± 0.97 | 1.95 ± 0.99 | 1.87 ± 0.94 | 2.08 ± 0.88 |
| Number of errors | 12.9 ± 3.3 | 13.09 ± 3.5 | 11.9 ± 3.3 | 13.8 ± 4.1 | 13.7 ± 3.2 | 13.8 ± 3.8 |
| EST-SB | ||||||
| Neutral | 860.7 ± 235 | 869.7 ± 238.3 | 910.3 ± 209.1 | 831.4 ± 176 | 813.2 ± 218.8 | 751.6 ± 197.7) |
| Negative | 933.9 ± 193.1 | 819 ± 168.4 | 927.7 ± 195.5 | 854.9 ± 238 | 770.4 ± 214 | 760.6 ± 177.6 |
| Positive | 860.7 ± 235 | 922 ± 200.4 | 910 ± 209.1 | 883 ± 228.8 | 786.4 ± 213.3 | 751.3 ± 176.5 |
| Suicide related | 907 ± 195.5 | 961.3 ± 200 | 921.5 ± 228.1 | 794.7 ± 212.5 | 811.6 ± 205.2 | 780.4 ± 174.3 |
| Affective Go/No-Go | 29.7 ± 8.06 | 29.4 ± 7.45 | 27.6 ± 6.2 | 30.9 ± 7.9 | 29.8 ± 7.2 | 29.6 ± 7.5 |
| A-RSQ | 9.09 ± 1.7 | 8.4 ± 1.6 | 8.7 ± 1.5 | 7.1 ± 1.5 | 9.2 ± 1.6 | 7.08 ± 9.2 |
Means and SDs a
The results of the analysis of covariance (ANCOVA) indicated a significant effect of treatments. Post hoc comparisons revealed significant differences between the tDCS and TTB-RDoC groups for ASI (anxiety sensitivity index) [BCa] 95% CI, -9.6 to -13.03; P < 0.001), SHAPS (BCa 95% CI, 8.3 - 5.9; P < 0.001), DTS (BCa 95% CI, 14.8 - 22.8; P < 0.001), DERS (BCa 95% CI, -31.8 to -43.3; P < 0.001), UPPS-P (BCa 95% CI, -0.96 to -1.8; P < 0.001; BCa 95% CI, -0.58 to -1.6; P < 0.001), FNR (BCa 95% CI, 5.3 - 3.4; P < 0.001), EST-SB (BCa 95% CI, -58.4 to -262.9; P < 0.006; BCa 95% CI, -57.9 to -284.5; P < 0.006), and A-RSQ (BCa 95% CI, -0.33 to -2.1; P < 0.012). In other words, TTB-RDoC treatment, compared to tDCS treatment, resulted in a significant reduction in anxiety sensitivity, distress tolerance, difficulties in emotional regulation, impulsive behavior, positive and suicide-related emotional Stroop effects, and rejection sensitivity in adults with NSSI. Additionally, TTB-RDoC treatment, compared to tDCS treatment, led to a significant increase in pleasure and FNR among adults with NSSI. Post hoc comparisons further showed significant differences between TAU and TTB-RDoC groups for DTS (BCa 95% CI, 0.10-8.3; P < 0.049). In other words, TTB-RDoC treatment, compared to TAU treatment, led to a significant decrease in distress tolerance among adults with NSSI.
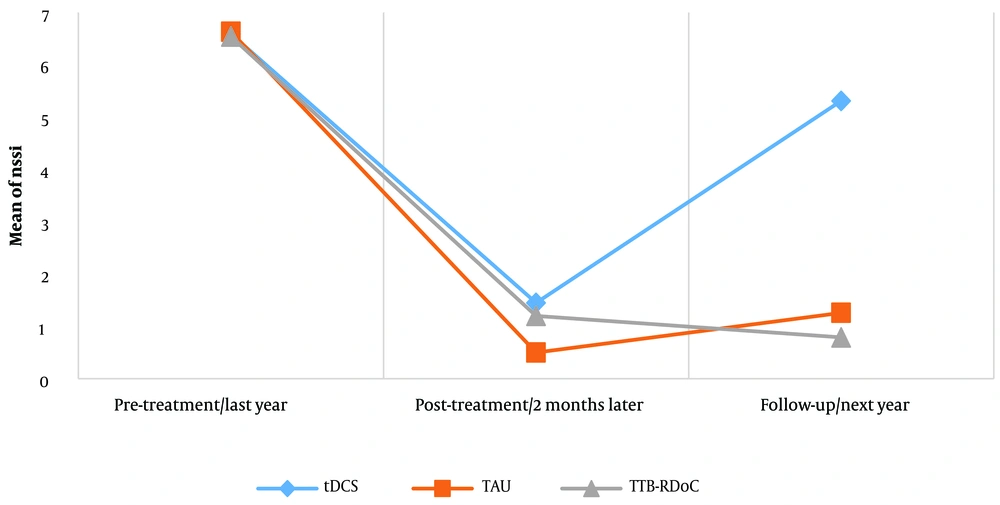
The results of the 3 × 2 combined 2-way repeated-measures analysis of variance (ANOVA) in the time factor showed that the main effect of time on self-injurious behaviors in adults with NSSI was significant (NSSI; F2.130 = 559.5; P < 0.001; η2 = 0.89). The effect of the group on the frequency of self-injurious behaviors in adults with NSSI was significant (NSSI; F2.65 = 58.5; P < 0.001; η2 = 0.64). The interactive effect of group and time on self-injurious behaviors in adults with NSSI was also significant (NSSI; F4.130 = 38.2; P < 0.001; η2 = 0.54). The Bonferroni post hoc test was used to simplify the interaction effects. Post-treatment post hoc comparisons indicated significant differences between the tDCS and TTB-RDoC groups for self-injurious behaviors (BCa 95% CI, -0.04 to -1.05; P < 0.041). In other words, TTB-RDoC treatment, compared to tDCS treatment, led to a significant decrease in self-injurious behaviors in adults with NSSI. Post-treatment post hoc comparisons showed no significant differences between TAU and TTB-RDoC groups for self-injurious behaviors (BCa 95% CI, -0.87 to -0.05; P < 0.126). Furthermore, follow-up post hoc comparisons showed significant differences between tDCS and TTB-RDoC groups for self-injurious behaviors (BCa 95% CI, -3.9 to -5.1; P < 0.001), indicating that TTB-RDoC treatment was more effective in reducing self-injury in adults with NSSI compared to tDCS treatment. Follow-up post hoc comparisons showed that there were no significant differences between the TAU and TTB-RDoC groups for self-injurious behaviors (BCa 95% CI, -0.03 to 1.1; P < 0.051; Figure 1).
5. Discussion
The findings of this study showed that treatment with TTB-RDoC, TAU, and tDCS significantly reduced scores related to anxiety sensitivity, distress tolerance, difficulties in emotional regulation, impulsive behavior, emotional Stroop test related to suicide, and rejection sensitivity. Additionally, there was an increase in pleasure and FNR among adults with NSSI at post-treatment. These results are consistent with previous studies that have highlighted the role of RDoC constructs, including negative valence systems, positive valence systems, cognitive systems, and social processes systems, in suicidal behaviors (14, 16, 18-20).
Furthermore, the findings revealed that treatment with TTB-RDoC, TAU, and tDCS significantly reduced the frequency of NSSI after treatment. This is consistent with previous studies, indicating the effectiveness of TTB-RDoC (6-8, 32, 33) and tDCS (10-12) in managing emotional/impulsive disorders and suicidal behaviors, particularly in the context of NSSI. However, it is important to note that TTB-RDoC and TAU resulted in significantly greater improvements in NSSI frequency compared to tDCS.
Moreover, the study observed slightly higher remission rates at post-treatment, with 77% for tDCS, 92% for TAU, and 81% for TTB-RDoC. This difference became more pronounced at the 12-month follow-up, with remission rates of 19% for tDCS, 80% for TAU, and 87% for TTB-RDoC.
Overall, the results suggest that TTB-RDoC is more effective in reducing NSSI frequency. These findings contribute to our understanding of treatment options for NSSI in adults and highlight the potential of TTB-RDoC as a promising approach to achieve lasting positive outcomes.
Previous studies have shown that patients receiving mindfulness-based therapy (MBT), dialectical behavior therapy (DBT), and Unified Protocol (UP) treatments completed significantly more therapy sessions compared to TTB-RDoC patients, who completed an average of only 16 sessions (33). In contrast, the TAU groups in other studies had session numbers similar to their respective index groups (32). In our study, the TAU group had comparable group sizes to previous studies (32). However, the effect sizes for NSSI reduction in previous TAU groups were small, with Cohen d values ranging between 0.23 and 0.40, in contrast to the large effect size found in our study (Cohen d = 0.77) (32). This RCT holds high ecological validity, particularly regarding the majority of patients engaging in NSSI. Since NSSI can occur in the context of various disorders and is commonly associated with suicidality (5), TTB-RDoC appears effective in treating NSSI in the context of a broad spectrum of transdiagnostic symptoms (33). Furthermore, our study focused on adults, a period during which NSSI prevalence rates peak while help-seeking is commonly low (5).
Additionally, previous studies on tDCS have shown positive impacts on neurocognitive functioning, including cognitive control strategies (12), which play a crucial role in adaptive emotion regulation, such as cognitive reappraisal (10).
Cathodal tDCS applied to the right DLPFC has been shown to regulate hyperactivity and reduce anxiety, as this region plays an essential role in cognitive functions and emotion regulation (12). Impairments in the activity of the right DLPFC can result in difficulties disengaging attention from pain and negative emotions, representing a core biological vulnerability in NSSI (11, 12). By targeting this region with tDCS, which aims to enhance emotion regulation skills, greater improvements in emotion regulation, decreased impulse control, and reductions in mood-related symptoms may be achieved in individuals (10, 11, 25).
5.1. Conclusions
In both the post-test and follow-up phases, all 3 intervention groups had a significant impact on self-injurious behaviors. However, there was a significant difference between the average frequency of self-injurious behaviors in the post-test and follow-up periods among individuals with self-injury in the tDCS, TAU, and TTB-RDoC treatment groups. In other words, TAU and TTB-RDoC treatments, compared to tDCS treatment, led to a significant reduction in self-injurious behavior among individuals dealing with self-injury. Furthermore, there was no significant difference in the average frequency of self-injurious behavior between the post-test and follow-up assessments among individuals with self-injury in the TAU and TTB-RDoC treatment groups. It is recommended that future research includes individuals with other emotional disorders, particularly borderline personality disorder with self-injury. Additionally, to enhance the comparability of treatment effects, future studies should incorporate a sham tDCS treatment group. Exploring stimulation in different brain areas (such as the left DLPFC, orbitofrontal cortex (OFC), nucleus accumbens (ACC), insula, etc) and comparing the effects among groups would also be valuable. Furthermore, future research should consider including female participants for gender-based comparisons to enhance the generalizability of results.
5.2. Limitations
In the second study, we faced challenges in establishing a waitlist control group and instead used conventional treatment. Additionally, the absence of sham electrical brain stimulation limited our ability to control for the placebo effect.