1. Background
In recent times, substance abuse disorder has emerged as a pervasive global issue, constituting a prominent concern of the contemporary world. Drug utilization has evolved into one of the foremost worldwide crises, implicating nearly all countries to varying degrees (1). This reality gains further emphasis through rigorous epidemiological investigations into drug use. For example, within the preceding year, a staggering 275 million individuals (constituting 5.6% of the populace aged 15 - 64) globally engaged in drug experimentation (2). This data accentuates the enormity of the challenge, amplifying its status as a pervasive global concern.
Emotion regulation denotes the deliberate actions that impact an individual's emotional responses during the course of emotional processing (3). Emotional dysregulation, conversely, indicates a vulnerability in managing emotional reactions towards stimuli, culminating in heightened tendencies towards aggression and violence, as well as an augmented risk of substance misuse (4). Numerous studies have consistently underscored elevated levels of mood disorders and depression among those grappling with methamphetamine abuse (5). Substantive evidence highlights the inherent challenge faced by substance users in effectively modulating their emotional states, often leading to a prevalence of negative emotional experiences (6).
Empirical investigations have revealed that methamphetamine abusers often experience heightened emotion dysregulation and amplified negative mood states, both of which are exacerbated by irregular daily routines, encompassing disturbances in sleep patterns (7). The challenge of emotion regulation is intrinsically intertwined with the craving to use substances (8). Our study presents a novel exploration of Interpersonal and Social Rhythm Therapy (IPSRT) as a potential therapeutic intervention. While previous research has extensively documented the adverse effects of methamphetamine on emotion regulation and cravings, our study is distinct in its application of IPSRT—a therapy traditionally employed in bipolar disorder management—to methamphetamine abusers. This innovative approach addresses a significant gap in the literature by exploring non-pharmacological interventions tailored to the unique challenges faced by this demographic. By focusing on both interpersonal relationships and circadian rhythm stabilization, IPSRT offers a dual-targeted strategy that may prove more effective than conventional methods in improving emotional stability and reducing cravings among methamphetamine users. This study, therefore, stands as a pioneering effort to bridge the gap between bipolar disorder therapies and substance abuse treatments, potentially setting a new course for future research and clinical practice in the field.
In recent years, there has been a widespread and concerning increase in the use of stimulants in Iran, with a particular emphasis on methamphetamine. Concurrent usage of amphetamines and opiates has been observed to interfere with other therapeutic approaches, including maintenance methadone therapy, consequently affecting the overall recovery process (9). Recently, a range of non-pharmacological therapies has emerged, both collectively and individually, as potential interventions to aid individuals in recovery. Nevertheless, it is noteworthy that the attrition rate and instances of premature cessation from treatment remain notably high. One such intervention is Interpersonal and Social Rhythm Therapy (IPSRT), a structured 12-session treatment designed to enhance individuals' mood and sleep quality by ameliorating irregularities associated with their daily routines (10). Originally formulated by Allen Frank for individuals grappling with bipolar disorder, this therapeutic approach targets irregular and maladaptive circadian rhythm patterns. Through the dual action of ameliorating interpersonal difficulties and regulating circadian rhythms, IPSRT facilitates the cultivation of stable moods and extended periods of well-being (11).
Given the pronounced mood fluctuations and emotional volatility frequently experienced by methamphetamine users, coupled with pronounced disruptions in sleep-wake cycles that encumber daily functioning—paralleling the challenges faced by individuals with bipolar disorder—it is rational to surmise that IPSRT's efficacy in enhancing mood and lifestyle among those with bipolar disorder could potentially extend to mitigating emotion regulation issues in individuals grappling with methamphetamine abuse (12).
2. Objectives
This study aimed to assess the efficacy of IPSRT in reducing emotion dysregulation and cravings in methamphetamine abusers in Tehran.
3. Materials and Methods
The study employed a semi-experimental design, featuring both a control group and an intervention group. This approach included comprehensive pre-test, post-test, and follow-up assessments conducted from December 2020 to July 2021 in Tehran, Iran. The sample included 40 methamphetamine abusers who had sought treatment at addiction recovery centers, where they typically underwent standard therapeutic interventions, commonly referred to as 'usual interventions.'
The inclusion criteria for participant selection included the following parameters: An age range of 20 to 45 years, proficiency in literacy skills (both reading and writing), meeting the diagnostic criteria for methamphetamine abuse disorder as outlined in DSM-5 TR, stable physical health condition allowing active participation in the study, not undergoing any other psychological therapy or pharmacological treatments for substance abuse during the study period, voluntary enrollment without coercion or undue influence, and no more than five months since the last instance of substance use. Exclusion criteria included psychiatric disorders (except for substance use disorder) determined by structured clinical interviews, insufficient literacy skills, severe substance abuse requiring hospitalization or intensive medical intervention within the last year, legal constraints or incarceration impeding regular participation, and significant cognitive impairments affecting therapy engagement or understanding.
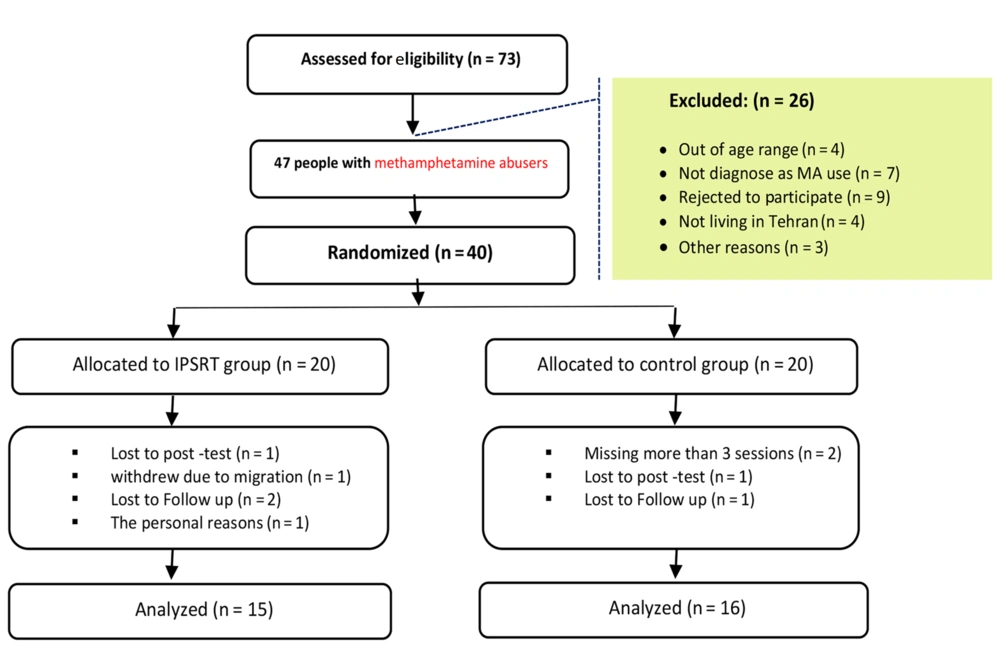
The participants were randomly assigned to two distinct groups: The intervention group (n = 20) and the control group (n = 20). Due to these exclusions, the final analysis was based on a cohort of 16 individuals in the intervention group and 15 individuals in the control group (Figure 1).
All participants in the study actively engaged in the administration of assessment tools during the pre-test, post-test, and follow-up stages. The intervention group underwent an IPSRT regimen comprising 12 sessions. Obtaining informed consent from clients is a fundamental ethical consideration in research. The study employed a meticulous process to ensure adherence to ethical standards, prioritizing ethical principles and adhering to the latest iteration of the Declaration of Helsinki to safeguard the rights and well-being of participants. These measures were taken to protect the confidentiality of sensitive information related to substance abuse and addiction. The present study received approval from the independent ethics committee at Shahid Beheshti University (IR.SBU.REC.1398.048), confirming adherence to ethical standards outlined in the latest iteration of the Declaration of Helsinki. In accordance with ethical guidelines, the control group did not receive IPSRT. Instead, they received usual therapeutic interventions commonly provided in addiction recovery centers.
The IPSRT encompasses four primary objectives: (1) Identifying domains of concern; (2) addressing mood disruptions associated with these areas; (3) examining ongoing interactions between patients and significant individuals; (4) and regulating patients' circadian rhythms, as posited by Frank et al. (13). This exploration extends to the addict's relational dynamics, anticipations associated with these relationships, and both positive and negative facets of these associations.
The independent variable is the application of IPSRT, while the dependent variables are emotion regulation, addiction severity, and craving, each assessed using the following standardized tools:
3.1. Difficulties in Emotion Regulation Scale (DERS-18)
The original version of the scale (36 items) was developed by Gratz & Roemer in 2004. Victor and Klonsky (14) developed a short form of the DERS-18. It is an 18-item test that measures the extent of difficulty in emotion regulation in a five-point range in six subscales as follows: Awareness, Clarity, Goals, Impulses, Non-Acceptance, and Strategies. The psychometric properties of the DERS-18 have been confirmed in Iranian populations (15). In the present study, Cronbach's alpha coefficient was 0.79 for this scale.
3.2. Drug Desire Questionnaire (DDQ)
A 14-item questionnaire originally developed by (16), possesses the capacity to assess a wide range of substances and has subsequently been employed for gauging cravings pertaining to diverse substances. This questionnaire serves to investigate prevailing cravings, with respondents providing their responses on a seven-point Likert scale. Empirical investigations have demonstrated the commendable convergent validity, internal consistency, and test-retest reliability of this scale (17). The reported Cronbach's alpha coefficient in the Iranian population was 0.78 (18). In the present study, Cronbach's alpha coefficient, indicative of reliability and internal consistency, was calculated to be 0.85 for this scale.
3.3. Severity of Dependence Scale (SDS)
It constitutes a self-administered questionnaire comprising five items, designed to gauge the extent of dependency on substances (19). Each of these items is evaluated on a four-point scale. Aggregating the individual item scores yields a cumulative SDS score, ranging from 0 to 15. Notably, the SDS exhibits commendable internal consistency, a unidimensional factor structure, and remarkable sensitivity and specificity in the identification of cannabis dependence. Various populations have indicated cutoff scores ranging from two to four. Within the Iranian context, the Cronbach's alpha coefficient for the SDS was 0.83 (20). In the present study, the Cronbach's alpha coefficient was 0.73.
3.4. Data Analyses
The data were analyzed using the statistical software SPSS version 26. A mixed repeated ANOVA was employed to assess the efficacy of IPSRT in enhancing emotions, reducing substance dependence, and mitigating craving.
4. Results
In terms of demographic characteristics, including age, marital status, job status, and substance use traits, it is noteworthy to observe that no substantial differences (P > 0.05) emerged between the two groups (Table 1). The sole exception to this pattern was discerned in the area of education.
| Variables | IPSRT; 16 (51.61%) | Control; 15 (48.38%) | Statistical Analyses |
|---|---|---|---|
| Age (y) | 29.44 ± 6.02 | 27.80 ± 6.29 | t (29) = 0 .74, P > 0.05 |
| Age of unset substance use (y) | 18.75 ± 3.45 | 19.73 ± 2.91 | t (29) = 0 .86, P > 0.05 |
| Methamphetamine use duration (y) | 3.51 ± 1.54 | 3.77 ± 1.85 | t (29) = 0 .42, P > 0.05 |
| Education (y) | 11.06 ± 2.48 | 9.13 ± 2.55 | t (29) = 2 .13, P ≤ 0.05 |
| Job status | χ2 (2) = 1.55, P > 0.05 | ||
| Unemployed | 3 (9.67) | 2 (6.45) | |
| Part time | 7 (22.58) | 11 (35.48) | |
| Employed | 5 (16.12) | 3 (6.45) | |
| Marital Status | χ2(2) = 0 .89, P > 0.05 | ||
| Single | 10 (32.25) | 8 (25.80) | |
| Married | 3 (9.67) | 5 (16.12) | |
| Divorced | 3 (9.67) | 2 (6.45) | |
| Substance use in family | χ2(1) = 1.55, P > 0.05 | ||
| Yes | 11 (35.48) | 7 (22.58) | |
| No | 5 (16.12) | 8 (25.80) |
a Values are expressed as No. (%) or mean ± SD.
b There was no significant differences between groups.
Repeated measures ANOVA was employed to scrutinize the distinctions between the IPSRT and control cohorts in relation to Emotion Dysregulation. The analytical framework entailed treating the group factor (IPSRT vs. control) as a between-subject element, while the assessment time points (pre-intervention, mid-intervention 1 & 2, post-intervention, and follow-up) were treated as within-subject variables. At the commencement of the study, an examination of the pretest data unveiled parallels between the two groups. Subsequently, a noteworthy disparity was ascertained to exist between the IPSRT and control groups [F (1, 29) = 8.68, P ≤ 0.01, η2 = 0.23]. This divergence was further explicated by the interplay between the between-subject and within-subject factors, as evidenced by interaction effect (TIME*GROUP) [F (4, 116) = 59.75, P ≤ 0.001, η2 = 0.67]. Moreover, within-subject dynamics (TIME) [F (4, 116) = 179.28, P ≤ 0.001, η2 = 0.86] exhibited considerable statistical significance (Figure 2 and Table 2).
Abbreviations: M, mean; SD, standard deviation.
a No significant differences between groups were observed in F test.
bT0 = pre-intervention (week 0).
cT1 = mid-term (week 2).
dT2 = mid-term (week 4).
eT3 = post-intervention (week 6).
fT4 = 1-month follow-up (week 10).
This study employed repeated measures ANOVA methodology to examine disparities between the IPSRT and control cohorts with respect to Craving. In this analytical framework, the group factor (IPSRT vs. control) was considered a between-subject variable, while assessment time points (pre-intervention, mid-intervention 1 - 2, post-intervention, and follow-up) were treated as within-subject variables. Upon examination of the pretest data, comparability between the two groups was evident. Subsequent analysis revealed notable dissimilarities between the IPSRT and control groups [F (1, 29) = 3.19, P ≤ 0.05, η2 = 0.10]. This divergence was further elucidated by the interplay between the between-subject and within-subject factors, as exemplified by the interaction effect (TIME*GROUP) [F (4, 116) = 31.51, P ≤ 0.001, η2 = 0.52]. The within-subject dynamics (TIME) [F (4, 116) = 65.63, P ≤ 0.001, η2 = 0.69] exhibited considerable statistical import (Table 3 and Figure 3).
Abbreviations: M, Mean; SD, Standard Deviation.
a No significant differences between groups were observed in F test.
b T0 = pre-intervention (week 0).
c T1 = mid-term (week 2).
d T2 = mid-term (week 4).
e T3 = post-intervention (week 6).
f T5 = 1-month follow-up (week 10).
The outcomes of the Repeated ANOVA unveiled discernible distinctions between the IPSRT and control cohorts concerning the Severity of Dependence Scale (SDS). This analytical inquiry featured the group factor (IPSRT vs. control) as a between-subject variable, juxtaposed with the assessment time points (pre-intervention, mid-intervention 1-2, post-intervention, and follow-up), which were treated as within-subject variables. At the inception of the investigation, no noteworthy divergence emerged between the IPSRT and control groups during the pretest assessment. However, upon subsequent analysis, notable disparities were evident between the IPSRT and control groups [F (1, 29) = 3.27, P ≤ 0.05, η2 = 0.101]. This differentiation was further expounded through the interplay of the between-subject and within-subject factors, as evidenced by the interaction effect (TIME*GROUP) [F (4, 116) = 6.76, P ≤ 0.01, η2 = 0.19]. The within-subject influence (TIME) [F (4, 116) = 6.66, P ≤ 0.001, η2 = 0.19] demonstrated substantial statistical significance (Figure 4).
5. Discussion
The findings illuminated a reduction in both emotion dysregulation and craving within the intervention group subjected to IPSRT. For instance, Haynes et al. (21) underscored the potency of IPSRT in alleviating depression scores in individuals contending with PTSD, depression, and sleep disorders. Furthering this trajectory, Crowe et al. (22) elucidated the effectiveness of Social Rhythm Therapy (SRT) in modulating depression scores amongst those grappling with major depressive disorder. These congruent findings resonate with the results gleaned from our present inquiry.
Methamphetamine abusers are commonly beset by disruptions in their daily routines, owing to the substance's perturbations of sleep patterns. Prolonged periods of wakefulness often ensue, culminating in disordered circadian rhythms and ensuing sleep dysfunction. This cascade contributes substantively to mood disturbances and despondency in methamphetamine abusers. The IPSRT, which regulates quotidian activities and circadian rhythms—such as sleep-wake cycles—stands forth as a pivotal modality for mood regulation. To this end, Robillard et al. (23) showed the salutary effects of sleep-wake cycle regulation in significantly diminishing depression amongst individuals grappling with mood disorders. IPSRT, in addition to its direct impact on mood regulation, exerts an indirect influence on emotional undulations by virtue of its enhancement of interpersonal relationships, amplification of social networks, and furnishing of social support (24). This comprehensive approach harmonizes with the insights proffered by Walker et al. (25), who accentuate the nexus between sleep disturbances and mood disorders. Methamphetamine abusers often find themselves ensnared in an injurious cycle: Methamphetamine consumption disrupts sleep patterns, engendering negative mood states that, in turn, impede the regulation of emotions. IPSRT intervenes sagaciously in this cycle, orchestrating the regulation of circadian rhythms and thus engendering amelioration in mood and bolstering emotional stability.
Craving assumes a pivotal mediating role in the dialectic between mood disorders and substance utilization. The elevated levels of craving concomitant with negative affect contribute substantively to escalated substance consumption (26). Moreover, extant scholarship underscores the bi-directional rapport between negative mood states and craving, with the former accentuating the latter (27). Consequently, interventions that proficiently calibrate emotional states, IPSRT among them, harbor the latent potential to abate drug cravings. The IPSRT’s role in mood regulation, underscored by the regulation of circadian rhythms, emerges as an instrumentality that effectually diminishes the impulse to succumb to temptation and craving.
This study makes a valuable contribution to our understanding of the potential benefits of IPSRT in addressing emotion regulation, addiction severity, and craving among methamphetamine abusers.
The current study reveals several inherent limitations that merit careful consideration. Primarily, its focus on methamphetamine users in Tehran restricts, thus it is crucial to acknowledge that each substance of abuse has unique neurobiological, psychological, and social dynamics influencing treatment response. Therefore, extrapolating these findings to other substances or populations requires caution. Moreover, the participant pool might not fully represent the broader methamphetamine user demographic, especially in terms of diverse demographics, socio-economic backgrounds, and treatment histories. This limitation underscores the need for a more diverse and representative sample to enhance the study's external validity. The timeframe for assessing the treatment effects of IPSRT may not adequately capture the long-term impacts and sustainability of the therapy. A longer follow-up period is essential to determine if improvements in emotion regulation, addiction severity, and craving are enduring or transient post-intervention. Variability in treatment delivery and therapist adherence could affect outcomes. Hence, standardizing the treatment protocol and ensuring fidelity are crucial for reliable results and robust comparisons across studies. The study recognizes the complex interplay of co-occurring factors like mental health disorders, socio-economic challenges, and deficits in social support among methamphetamine users. However, these factors' potential impact on treatment outcomes is not entirely controllable within the current research design. Furthermore, the design may not fully account for placebo effects or participant expectations about IPSRT's efficacy. Including control groups receiving placebo treatments or alternative interventions would better delineate IPSRT's specific therapeutic effects.
5.1. Conclusions
Summarizing the findings of this research, it becomes evident that IPSRT stands as a crucial intervention in the realm of mental health, particularly for its efficacy in stabilizing mood and addressing emotion dysregulation. This therapy emerges not only as a potent tool for individuals grappling with methamphetamine addiction but also as a versatile strategy applicable across a broad spectrum of conditions marked by emotional and mood disturbances. The application of IPSRT extends beyond the confines of substance abuse, demonstrating significant potential in managing bipolar disorder, high-risk behaviors in adolescents, and other clinical scenarios where mood dysregulation is a core challenge. The current study has illuminated IPSRT's effectiveness within a particular demographic, yet it also opens the door to broader, more diverse applications. Future research should aim to incorporate a wider array of participant profiles, including varied demographics and clinical backgrounds, to thoroughly assess the therapy's applicability and effectiveness across different populations. Such inclusive research approaches would provide a more comprehensive understanding of IPSRT’s role in diverse clinical contexts and its adaptability to varying individual needs. Moreover, extending the duration of observation and follow-up in future studies is crucial. Longer-term studies would allow for a deeper understanding of the sustained impact of IPSRT, offering insights into its long-term efficacy and potential for lasting change in emotional regulation and mood stability. This approach would be invaluable in discerning the enduring benefits of IPSRT and its role in long-term therapeutic strategies. In conclusion, IPSRT emerges from this study as a promising, multifaceted therapeutic intervention. It holds significant promise in addressing a range of mood and emotional regulation challenges, indicating its potential as a key addition to the therapeutic arsenal. As research continues to evolve in this field, IPSRT is poised to play an increasingly important role in offering effective, tailored approaches to individuals facing the complexities of mood disorders and emotional dysregulation. The implications of this study are far-reaching, suggesting new avenues for treatment and a deeper understanding of the intricate dynamics of mental health interventions.
![Emotion dysregulation at pre- (T0), mid- (T1 and T2), post-intervention (T3), and 4-weeks follow-up (T4) (error bars represent a 95% confidence interval [CI]). Emotion dysregulation at pre- (T0), mid- (T1 and T2), post-intervention (T3), and 4-weeks follow-up (T4) (error bars represent a 95% confidence interval [CI]).](https://services.brieflands.com/cdn/serve/3170b/ea5c3d73ec45f12db40b4feb1275db95e58f9809/ijhrba-140136-i002-F2-preview.webp)
![Craving at pre- (T0), mid- (T1 and T2), post-intervention (T3), and 4-weeks follow-up (T4) (error bars represent a 95% confidence interval [CI]). Craving at pre- (T0), mid- (T1 and T2), post-intervention (T3), and 4-weeks follow-up (T4) (error bars represent a 95% confidence interval [CI]).](https://services.brieflands.com/cdn/serve/3170b/142d745d1c76364ae73f0fd078486492bea92a4f/ijhrba-140136-i003-F3-preview.webp)
![Severity of dependence scale (SDS) at pre- (T0), mid- (T1 and T2), post-intervention (T3), and 4-weeks follow-up (T4) (error bars represent a 95% confidence interval [CI]). Severity of dependence scale (SDS) at pre- (T0), mid- (T1 and T2), post-intervention (T3), and 4-weeks follow-up (T4) (error bars represent a 95% confidence interval [CI]).](https://services.brieflands.com/cdn/serve/3170b/af8ba688cce6de0c81f09ef4d6adba2e59987100/ijhrba-140136-i004-F4-preview.webp)