1. Background
Deliberate self-harm (DSH) refers to non-fatal, acute acts of bodily harm or injury carried out intentionally by the individual themselves as a result of various motivations, either with or without suicidal intention (1, 2). According to the fifth edition of the diagnostic and statistical manual of mental disorders (DSM-5), DSH encompasses a broad spectrum of self-destructive behaviors that damage the body in every possible non-fatal way, regardless of intention to die (2). The individual may deliberately ingest a known poison, a medicinal substance that is known to be toxic in excess of the prescribed therapeutic dosage, or employ some other means to commit self-harm. This act is usually aimed at bringing about change, which the subject desires via the actual or expected consequences of DSH or escaping an intolerable situation (2). However, there is a broad category of self-injurious behaviors that result in direct harm to one's body, with definitions varying based on whether this behavior includes suicidal or non-suicidal intention (3). For instance, non-suicidal self-injury (NSSI), or parasuicide, is defined as an act of intentional, self-directed harm to one's body without the conscious intention of dying, while the term suicidality, including suicidal ideation and suicide attempts, covers thoughts, actions, and behaviors focused on deliberately ending one's own life (3-5). Such nomenclature is often used synonymously in the literature, with both DSH and NSSI used interchangeably to refer to behaviors and acts related to the self-inflicted destruction of bodily tissues without suicidal intent (1, 3, 5).
Existing research has shown that while DSH is multifactorial in origin, it occurs primarily in young people (6-8). A recent meta-analysis found that the aggregate lifetime prevalence of NSSI in children and adolescents was 22.1% (95% confidence interval [CI]: 16.9 - 28.4%) (8). Overall, DSH tends to be more frequent in females than males, as well as in individuals who are deprived or socially isolated (1, 9). Patients diagnosed with DSH are frequently aggressive and impulsive and demonstrate cognitive inflexibility (i.e., 'black-and-white' thinking) and impaired decision-making and problem-solving capabilities (9, 10). Moreover, associations have been reported between DSH and various mental health conditions, including anxiety, mood disorders, borderline personality disorder, conduct disorder, alcohol use disorder, post-traumatic stress disorder, and obsessive-compulsive disorder (10-13). Alarmingly, a history of self-harm is associated with an increased risk of subsequent suicide attempts; as such, DSH represents a serious public health concern requiring immediate intervention (14, 15).
Globally, the prevalence of DSH in the general population reportedly ranges from 4 - 10%, although this has increased tremendously in recent years to around 14% - 16% due to various psychosocial, familial, and biological factors (1, 4). However, there are comparatively few reports of such incidents originating from Arab countries (16). Several studies have documented the incidence of DSH in the Middle East region. In Jordan, Hanania et al. reported results indicating an overall lifetime prevalence of 22.6% for NSSI (17). Similar trends have been reported in Saudi Arabia (18), Kuwait (19), and Egypt (20).
Self-harm in all forms is expressly forbidden in Islam, a factor which may explain why Muslim populations tend to report low rates of suicide attempts or DSH; on the other hand, because such topics are considered highly taboo and invite considerable social and religious disapproval, such incidents may go under-reported because of their highly stigmatized public perceptions (16). In Oman, there is a similar dearth of DSH-related research, although one older study reported that the incidence of DSH increased from 1.9 to 12.8 cases per 100,000 individuals between 1993 and 1998 (21). Another slightly more recent study reported that a total of 117 patients were admitted following acts of DSH between 2012 and 2014 to a single hospital in Muscat (21, 22).
2. Objectives
The present study aimed to add to the literature on DSH in Oman by reporting more recent data regarding the demographic and clinical characteristics of patients presenting with non-suicidal DSH to a single tertiary center in Oman to identify any change in patients demographic and clinical characteristics amidst the rapid modernization and globalization.
3. Patients and Methods
This retrospective, cross-sectional study was conducted at the Sultan Qaboos University Hospital (SQUH), a tertiary hospital in Muscat, Oman. All patients with clinical diagnoses of DSH who presented to the SQUH or were admitted to the intensive care unit or the medical, psychiatry, or surgical wards of the hospital from January 2019 to December 2021 were deemed eligible for inclusion in the study. However, patients with accidental injuries or those suspected of having attempted suicide (i.e., patients with injuries associated with an intention to end one's life) were excluded. All clinical diagnoses of DSH were made by an expert, specialized psychiatrist based on the patient's unique medical history and clinical presentation.
Patients treated at SQUH get all their medical data, including their clinical history, signs, symptoms, and physical investigations, recorded in the electronic health records system. An international disease classification-10 (ICD-10) code is assigned to each patient's visit episode by the specialist physician. The ICD-10 codes related to self-injury, self-harm, poisoning, and suicide attempts were used in conjunction with the patient's Omani nationality, age of 10 years or older, and the time period from 2019 to 2021 to retrieve patient data for this study from the hospital information system (HIS) and medical records. A total of 246 patients were obtained from the HIS. A psychiatrist specialist further screened this list, and 148 patients were excluded for reasons related to inaccurate diagnosis, suspected suicide attempt, or suicide intention.
Information on a total of 98 patients was collected regarding the patients' sociodemographic characteristics, including their age, gender, marital status, and education level, as well as their clinical characteristics, including the number of DSH-related hospital admissions throughout the study period, the presence of additional mental health comorbidities, any stressors or factors reported to have triggered the DSH incident, and information regarding the method (and nature of the DSH act itself).
Collected data were analyzed using the statistical package for social sciences (SPSS) software, version 23 (IBM Corp., Armonk, NY). The obtained raw data were first checked for errors, outliers, and uniformity. Secondly, the data were categorized for some variables or left in their continuous form based on the set study objectives. Descriptive results were presented as frequencies and percentages. Univariate analysis using Pearson's chi-squared test was performed to determine associations between DSH categorical outcome variables and the patient's various sociodemographic and clinical characteristics. The level of statistical significance was set at P ≤ 0.05. Ethical approval for this study was obtained from the Medical Ethics and Research Committee of the College of Medicine and Health Sciences, Sultan Qaboos University, Muscat, Oman (MREC #2762). Patient direct consent was not required due to the retrospective nature of the data collection process. Patients treated at the SQUH give their data knowing that it may be used for research purposes. However, no potentially identifying information was included in order to preserve data confidentiality and the patient's privacy and anonymity.
4. Results
4.1. Patient Demographic and Clinical Characteristics
A total of 98 patients were clinically diagnosed with DSH during the study period, of whom 17 (17.3%) were male and 81 (82.7%) were female. In terms of marital status, the majority of patients were single (n = 65; 66.3%). Overall, most were aged 10 - 25 years (n = 60; 61.2%), while just over a quarter were 25 - 40 years of age (n = 27; 27.6%), and only 11 (11.2%) patients were > 40 years of age. Over half of the sample were either college students (n = 27; 27.6%) or school students (n = 24; 24.5%).
Most patients (n = 62; 63.3%) were admitted to the SQUH only once during the study period, although a few (n = 4; 4.1%) required multiple admissions due to recurrent DSH acts. The remaining 32 (32.7%) patients did not require admission and were treated as outpatients (Table 1). There was a high rate of mental health comorbidities in the sample [61 (62.2%)], with the most common being psychotic disorders 27 (27.6%), followed by major depressive disorder 24 (24.5%), and personality disorders 10 (10.2%).
| Hospital Admissions | No. (%) |
|---|---|
| 0 | 32 (32.7) |
| 1 | 62 (63.3) |
| 2 | 2 (2.0) |
| ≥ 3 | 2 (2.0) |
Frequency of Hospital Admissions Among Patients Presenting with Deliberate Self-harm to a Tertiary Hospital in Oman (N = 98)
4.2. Clinical Characteristics of Deliberate Self-harm Acts
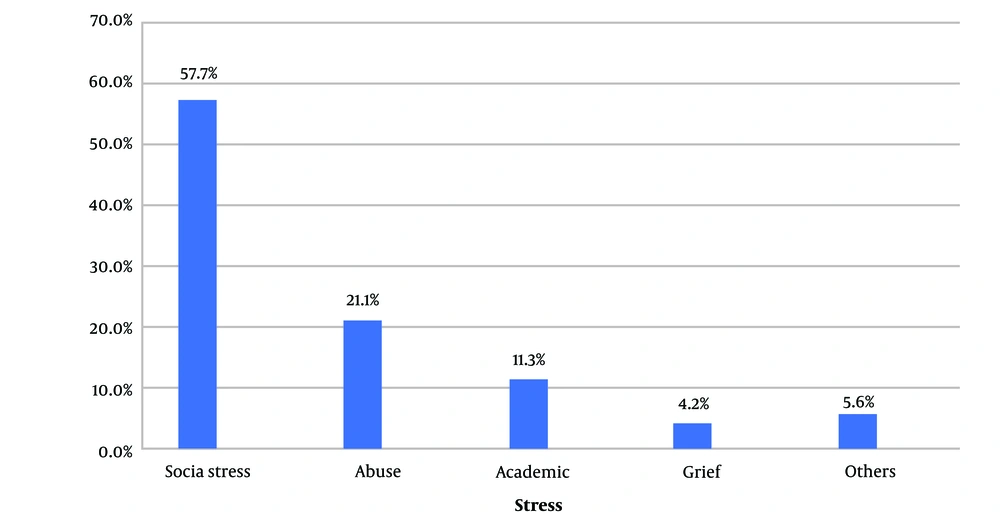
The overwhelming majority, 87 (88.9%), of DSH acts were impulsive in nature, with only 11 (11.1%) patients having been found to commit DSH in a premeditated manner. Among the 71 (72.4%) patients for whom DSH triggers were reported, the most frequently reported was social stress (n = 41, 57.7%), followed by abuse (n = 15, 21.1%), academic/study stress for students (n = 8, 11.3%), grief (n = 3, 4.2%), and other stressors, including financial- and work-related triggers (n = 4, 5.6%) (Figure 1).
The most common DSH method involved drug overdoses, especially with analgesics (n = 58, 58.2%), followed by self-cutting (n = 28, 28.6%), particularly of the wrist but also the upper limb and femoral veins, ingestion of chemical solutions (n = 11, 11.2%), including cleaning disinfectant, antiseptics, bleach, and other detergent solutions, hanging (n = 8, 8.2%), jumping from heights (n = 2, 2.0%), and other methods of DSH, including car accidents and attempts at electrocution (n = 7, 7.1%).
4.3. Associations Between Patient Characteristics and Deliberate Self-harm Methods
Self-cutting tended to be more prevalent in patients aged > 40 years (54.5% vs. 25.3%; P = 0.070), while drug overdoses were more common in patients aged < 40 years (60.9% vs. 36.4%; P = 0.067) (Table 2).
| Methods | Age Group (y), No. (%) | P-Value a | |
|---|---|---|---|
| < 40 | ≥ 40 | ||
| Drug overdose | 53 (60.9) | 4 (36.4) | 0.067 |
| Self-cutting | 22 (25.3) | 6 (54.5) | 0.070 |
Associations Between Age and Methods of Deliberate Self-harm Among Patients Presenting to a Tertiary Hospital in Oman (N = 98)
Similarly, drug overdoses represented a more common method of DSH for female patients (63.0% vs. 35.3%; P = 0.067), while male patients more frequently participated in self-cutting (47.1% vs. 24.7%; P = 0.080) (Table 3). However, none of these associations met the necessary threshold for statistical significance (P ≤ 0.05).
| Methods | Gender, No. (%) | P-Value a | |
|---|---|---|---|
| Male | Female | ||
| Drug overdose | 6 (35.3) | 51 (63.0) | 0.067 |
| Self-cutting | 8 (47.1) | 20 (24.7) | 0.080 |
Associations Between Gender and Methods of Deliberate Self-harm Among Patients Presenting to a Tertiary Hospital in Oman (N = 98)
5. Discussion
This study aimed to investigate the characteristics of patients presenting with DSH to a tertiary hospital in Oman between January 2019 and December 2021. A total of 98 patients were diagnosed with DSH during the three-year period, of whom just under two-thirds were 10 - 25 years old (61.2%), with only a minority (11.2%) being aged > 40 years. In addition, most patients were unmarried (66.3%) and students (52.0%), findings to be expected given the youthful nature of the sample. A similar study conducted in India reported comparable findings in which DSH was more common in patients aged < 40 years (84.4%) and in college and school students (27.6% and 24.5%, respectively) (23). Another study from Pakistan found DSH to be most frequent among 21-25-year-old patients (24). Researchers have hypothesized that younger individuals face additional social and financial stressors and have fewer coping mechanisms, thereby compromising their mental well-being and their capacity to adjust to stressful situations (11). Other explanations include their susceptibility to peer pressure, impulsivity, and recklessness, and their lower capacity for emotional self-regulation (10, 25). Moreover, studies on DSH in Western populations showed a similar trend of the act among adolescent and younger adult age groups with female gender predominance (26). This indicates a common worldwide demographic characteristic of individuals with DSH regardless of their cultural and religious background.
In addition, the vast majority (82.7%) of patients presenting with DSH in the present study were female. Many researchers have similarly observed a greater prevalence of DSH in females than in males in both community and hospital settings (22-25). This has been attributed to the fact that female adolescents and young women tend to be more emotionally sensitive than their male counterparts and often suffer from low self-esteem, thereby being more likely to harm themselves when under stress (22, 25). Alternatively, other researchers have claimed that these prevailing assumptions are due to the over-representation of females in clinical compared to community-based research or the under-reporting of DSH in males (27, 28). However, there is some evidence to indicate that the effect of gender may be modified by age, with NSSI being significantly more frequent among females in mid-adolescence (i.e., at 16 - 19 years of age), partly explained by the increased frequency of psychological distress in this group at this age, with no significant gender differences found in either younger or older individuals (29).
A recent systematic review also addressed the positive link between NSSI and perfectionism, similarly noting that the majority of the included studies consisted of predominantly female participants (30). In some cases, perfectionism represents a maladaptive coping mechanism and can result in feelings of intense shame and self-criticism regarding any perceived failure (30, 31). Such factors can lead to DSH as a form of self-punishment or, alternatively, as a means of re-exerting control or personal mastery (32-34). Moreover, DSH has been reported as a method of relieving emotional distress and replacing it with physical discomfort or pain (34).
There is strong evidence linking both DSH and suicidal behaviors to various mental health conditions, indicating that such disorders should be considered important risk factors for DSH (6, 9-12). Indeed, the current study observed a high rate of mental health comorbidities (62.2%), with the most common being psychotic disorders (27.6%), including schizophrenia, acute psychotic episodes, schizoaffective disorder, and bipolar affective disorder, followed by major depressive disorder (24.5%) and personality disorders (10.2%). This is in agreement with a previous study from India in which more than half of the patients with DSH (52.3%) had a diagnosable psychiatric illness at the time of presentation (23). Another study from Pakistan also indicated that 76.4% of patients admitted to a tertiary university hospital for DSH suffered from comorbid psychiatric disorders (24).
In addition, DSH has been linked to specific mental health disorders. Son et al. reported that component factors of anxiety (oversensitivity and physical and sleep problems) and depression (negative self-image) were significantly linked to self-harming behaviors among Korean adolescents (25). According to another study, 28.6% of 327 individuals diagnosed with schizophrenia and substance misuse problems reported incidents of self-harm or attempted suicide (35). The link between DSH and depression is also well supported, especially as one criterion for a diagnosis of major depressive disorder is suicidal ideation, a factor linked to recurrent acts of DSH (2, 15, 29). Furthermore, a small percentage of cases of DSH have been associated with personality disorders, namely borderline personality disorder, with related symptoms including impulsivity, mood lability, and suicidal acts (36). Overall, the vast majority (88.9%) of acts of DSH identified in the present study were reported to be impulsive in nature, with only a minority of patients participating in planned or premeditated acts of DSH. This finding is in line with a previous systematic review in which the majority of included studies indicated an association between impulsivity and acts of self-harm (10).
Among the subset of patients in the current study for whom there was information available regarding triggering stressors for DSH, social stressors were found to be the most common (n = 41, 57.7%); this included family disputes, stress related to romantic or social relationships, conflict with others, and bullying. This was followed by various types of abuse in 21.1% (n = 15) of patients, including psychological, sexual, physical, and verbal abuse. Study- and academic-related triggers were reported in 11.3% (n = 8) of patients in this study, with grief and other triggers like financial or professional/work-related stressors being the least common. A study in Pakistan similarly showed that precipitating factors for acts of DSH included conflict with family, marital problems, and, in some cases, unemployment and chronic illnesses (24).
In the current study, drug overdoses (58.2%) were the most frequently applied method of DSH; this finding differs from the existing literature, which indicates that self-cutting is the most common method (45%) (37). This discrepancy may be due to sociocultural factors in Middle Eastern populations in which DSH is considered a taboo and highly stigmatized topic due to religious teachings, resulting in patients possibly choosing to apply a less 'visible' or life-threatening method of self-harm. Moreover, the rate of DSH recurrence in the present study was very low (4.0%) compared to other populations (12.4 - 22%) (38, 39). This low rate of repetition might further indicate the acute or highly stigmatized nature of DSH in Omani society or may indicate that affected patients received effective and appropriate counseling and behavioral support after their first incident, thereby helping them to cope with future stressors and triggers.
Although not statistically significant, the current study revealed that self-cutting tended to be more frequent among patients aged > 40 years (54.5% vs. 25.3%), while drug overdoses were more common among those aged < 40 years (60.9% vs. 36.4%). This could be because younger adults are more likely to use non-fatal methods with the intention of drawing attention or as a 'cry for help', while older adults are more likely to use more fatal methods that have been associated with the purpose of ending one's life, especially if the previous attempt failed. Similarly, drug overdoses were more frequent among females (63.0% vs. 35.3%) in the present study, whereas males more commonly participated in self-cutting (47.1% vs. 24.7%). This might be because self-cutting is inherently a more violent and aggressive act of DSH compared to a drug overdose, with such traits being more frequently associated with the male gender (40).
In an analysis of the first national DSH registry, Perry et al. also found that self-cutting was more frequent in Irish male patients than female patients (20% vs. 13%; P < 0.001) (38). However, the researchers noted that drug overdoses were significantly more likely to occur in older patients, a finding contradictory to that of the present study (38). Other researchers have also reported conflicting findings to those seen in the current study, with Sornberger et al. reporting that adolescent girls were more likely to use DSH methods that involved blood-letting (e.g., cutting or scratching themselves), whereas adolescent boys were more likely to punch or burn themselves or bang their heads (41). Similarly, in another study involving an adult sample, women were more likely to engage in cutting acts, whereas men were more likely to punch themselves (42). Such discrepancies are likely related to the individual patient's intention and motivation for committing the act (34, 43).
5.1. Study Strengths and Limitations
There is a considerable dearth of information concerning DSH originating from Arab countries (44). Unfortunately, recent research has indicated that suicidality and self-harm in this part of the world may be more prevalent than previously believed, thereby representing an urgent health problem (45). The objective of the research was to provide more recent insight into the sociodemographic and clinical features of such patients, as well as information regarding the nature and methods of specific DSH acts. However, the small sample size and the inclusion of patients presenting to a single center could have affected the representativeness of the findings and the power of the study to detect associations. Secondly, the retrospective nature of the data collection method impacted the ability of the researchers to provide more detailed information concerning the motivations behind DSH acts. Further studies are recommended to address these limitations.
5.2. Conclusions
In conclusion, this study found that DSH was more common among young, unmarried female students with comorbid mental disorders. As DSH is considered a preventable act and carries the risk of subsequent suicide attempts, primary care physicians in Oman should ensure that they are familiar with the specific signs, symptoms, risk factors, and correlates of DSH, including comorbid psychiatric conditions. In addition, public awareness of DSH should be increased in order to reduce the social stigma surrounding this topic and highlight the importance of counseling for at-risk individuals, including the provision of an anonymous public helpline to encourage this patient group to seek appropriate mental health support and to learn more constructive and less hazardous adaptive coping mechanisms. Moreover, given the high prevalence of DSH among adolescent and young adult age groups, public health campaigns to promote mental health well-being among this population group should be considered in schools and colleges. This can be achieved through raising awareness, implementing screening and early intervention, and fostering inter-sectoral collaboration to create a supportive environment that prioritizes mental health needs.