1. Background
The global outbreak of the novel coronavirus (COVID-19) has garnered extraordinary attention from experts worldwide (1). Iran faced a dual crisis: It has one of the highest rates of opioid dependence globally (2) and is among the countries most affected by the novel coronavirus. The widespread use of opium in Iran appears to stem from a cultural norm and a positive attitude toward its use (2, 3). Opium dependence significantly impacts the cytokine network and the immune system (4). Individuals with compromised immune systems are more vulnerable to COVID-19 infection. The high mortality rate in COVID-19 patients is attributed to the cytokine storm caused by elevated levels of interleukin-6 (IL-6) in these individuals (5, 6).
The influence of opium on the prevalence, severity, and mortality rate of COVID-19 remains uncertain and controversial (7, 8). Some studies have reported a protective effect of opium addiction against COVID-19 infection (8). However, a study on the association between opium abuse and COVID-19 mortality in the Iranian population revealed a statistically significant connection between a positive history of opium abuse and increased mortality (9). Another study indicated that opium-addicted patients who contracted COVID-19 experienced higher fevers, more severe disease progression, and more specific symptoms. These patients also showed increased signs of inflammation in laboratory tests and were more likely to suffer from superinfections (10). A pilot study conducted at the same center as the present study found that the mortality rate among opium-dependent COVID-19 patients was higher than that of the general COVID-19-infected population (11). However, considering the wide confidence interval, the effect size regarding mortality in opium-addicted COVID-19 patients requires further investigation (11).
Additionally, nicotine-dependent patients, who have respiratory vulnerabilities, are at greater risk due to the up-regulation of the angiotensin-converting enzyme-2 (ACE2) receptor by smoking, which is the known receptor for both coronavirus and acute respiratory syndrome (12). However, the impact of cigarette smoking on susceptibility to COVID-19 is still being debated. Although it is widely known that smoking is linked to illness and death in numerous respiratory infections, certain studies have suggested a potential "smoker's paradox" in COVID-19, finding fewer active smokers among COVID-19 patients and suggesting that smokers might have some protection from infection and severe complications (13). In severe COVID-19 patients, the immune system is activated, pro-inflammatory cytokines are increased (14), and the release of many cytokines is induced (15). These events play an important role in mortality (5). In the cytokine storm, IL-6 plays a central role. IL-6 is a multi-effective cytokine with both anti-inflammatory and pro-inflammatory effects (16). On the other hand, ACE2 expression is upregulated by nicotine, increasing human pneumocytes' susceptibility to COVID-19 (17). However, some authors believe that nicotine reduces the number of ACE2 receptors, and a recent literature review has found no clear consensus regarding the impact of smoking on COVID-19 infection (18).
2. Objectives
We studied opium and tobacco use in general, and the different intensities of consumption of these two substances, and their outcomes in COVID-19 infected patients referred to Imam Khomeini Hospital in Sari, Mazandaran, Iran.
3. Patients and Methods
3.1. Study Population
This cross-sectional study was conducted among patients with COVID-19 infection who were referred to Imam Khomeini Hospital in Sari, Mazandaran, Iran, in 2019-2020. This hospital is a referral center that received many patients from all over the province during the pandemic of COVID-19. A convenience sample of 900 patients was studied. The sample size was calculated based on Saeedi et al.’s study (11) (with an opium addiction prevalence of 10% among COVID-19 infected inpatients) using a 95% confidence level and an acceptable error of 0.02.
Inclusion criteria were a clinical diagnosis of COVID-19 based on a positive polymerase chain reaction (PCR) test or a positive lung computerized tomography (CT) scan, and proficiency in the Persian language. Patients who did not respond to phone calls or did not answer the questions were excluded from the study.
3.2. The Method of Implementing the Plan and Data Collection
Prior to implementation, the study proposal (No. 7739) was approved by the Research Council of Mazandaran University of Medical Sciences (MAZUMS).
A total of 1924 patients were registered in the system. Parameters studied in the registry include demographic variables, the patient's complaints at the time of arrival at the hospital, vital signs, hospitalization indication and severity of the disease, history of medical diseases and previously consumed medications, lung CT-scan results, echocardiography, medications, hospitalization complications, and final status at discharge time. The present registry included both inpatient and outpatient cases (19).
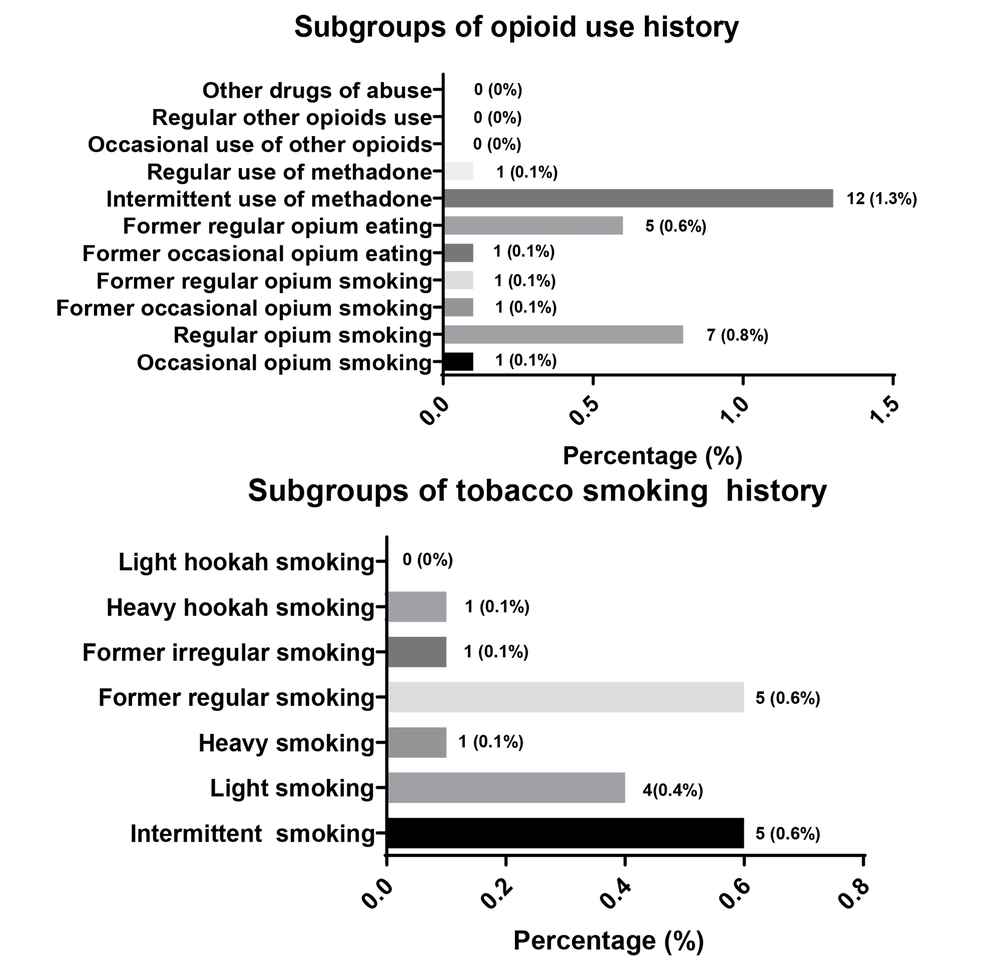
After obtaining permission from the hospital manager and the patient registrar, a trained psychiatric resident filled out the checklist for convenient samples that had even numbers (including 900 patients). Additional required information that was not in the file, especially about the details of tobacco smoking (cigarette and/or hookah) and opioid consumption (opium and/or methadone and/or other opioids), was completed by telephone interviews with the patient or the patient's companion. Subgroups of tobacco smoking and opioid consumption included intermittent smoking, light smoking, heavy smoking, former regular smoking, former irregular smoking, heavy hookah smoking, light hookah smoking, occasional opium smoking, regular opium smoking, occasional opium eating, regular opium eating, former occasional opium smoking, former regular opium smoking, former occasional opium eating, former regular opium eating, regular use of methadone, intermittent use of methadone, former regular use of methadone, former intermittent use of methadone, and current and former use of regular and occasional other opioids. Phone calls were made to the numbers listed in the registry file.
3.3. Ethical Considerations
This study was conducted in full compliance with the Declaration of Helsinki and the ethical principles of the ethics committee of MAZUMS (code: IR.MAZUMS.REC.1400.146). Informed consent was obtained from all participants prior to their participation in the study.
3.4. Data Analysis
Using descriptive statistics, continuous variables were presented as mean ± standard deviation, while qualitative variables were reported as number (percent). All statistical indices were calculated by weighting data based on population size. Before the main analysis, the Kolmogorov-Smirnov test was performed to check for normality. Independent sample t-tests or Mann-Whitney U tests were used for comparing quantitative variables, and chi-square and Fisher's exact tests were used for comparing qualitative variables between tobacco/opium users and non-tobacco/opium users. Statistical analysis was performed using SPSS version 25 software package (SPSS Inc., Chicago, IL, USA). A P-value of 0.05 or lower was considered statistically significant.
4. Results
Out of 900 participants, 542 (60.2%) were male and 358 (39.8%) were female. Of these patients, 808 (89.8%) were discharged, while 92 (10.2%) unfortunately died.
Opioid use was reported by 29 (3.2%) patients, and 17 (1.9%) patients were tobacco smokers. The subgroups of tobacco and opioid use were investigated, and the results are shown in Figure 1.
Fatigue was significantly lower in opioid users compared to other patients (P = 0.009). However, no statistically significant relationship was found between other initial symptoms and signs and opium use. Additionally, no statistically significant relationship was found between any of the initial symptoms and signs and tobacco use.
Opium use was higher among men, individuals aged 70 years or older, urban dwellers, and illiterate people (P < 0.05). Tobacco use was significantly higher in male patients (P = 0.001), and death was significantly higher in tobacco smokers compared to nonsmokers (P = 0.023).
Cardiovascular (P = 0.000) and airway diseases (P = 0.004) were significantly more prevalent in opioid users but not in smokers. One or more coexisting diseases were significantly higher in opium users (P = 0.014), while this feature was not significantly different between tobacco users and other patients (P = 0.513).
Heart rate was significantly higher in opioid users compared to other patients (P=0.009), but no statistically significant relationship was found between other initial clinical information of patients with a positive history of opium use and other patients. No statistically significant relationship was found between any of the initial laboratory tests of patients with a positive history of opioid use and other patients. Only systolic blood pressure was significantly higher in tobacco users (P = 0.010), and the erythrocyte sedimentation rate (ESR) was significantly lower in tobacco users (P = 0.046).
No statistically significant relationship was found in any of the subgroups of opioid and tobacco users in terms of outcome (death or discharge) (P > 0.05) (Table 1).
| Subgroups | Outcome; (Death = 92) | Outcome; (Discharged = 808) | P-Value b |
|---|---|---|---|
| Opioid use history | |||
| Intermittent opium | 0.102 | ||
| Yes | 1 (100) | 0 (0) | |
| No | 91 (10.1) | 808 (89.8) | |
| Regular opium | 0.155 | ||
| Yes | 2 (28.6) | 7 (71.4) | |
| No | 90 (10.1) | 803 (89.9) | |
| Former intermittent opium | 1 | ||
| Yes | 0 (0) | 1 (100) | |
| No | 92 (10.2) | 807 (89.8) | |
| Former regular opium | 0.102 | ||
| Yes | 1 (100) | 0 (0) | |
| No | 91 (10.1) | 808 (89.9) | |
| Former regular opium eating | 1 | ||
| Yes | 0 (0) | 5 (100) | |
| No | 92 (10.3) | 803 (89.7) | |
| Intermittent Ex opium eating | 0.352 | ||
| Yes | 2 (0) | 10 (83.3) | |
| No | 90 (10.3) | 798 (89.9) | |
| Intermittent methadone | 1 | ||
| Yes | 0 (0) | 1 (100) | |
| No | 92 (10.2) | 807 (89.8) | |
| Regular methadone | 1 | ||
| Yes | 0 (0) | 1 (100) | |
| No | 92 (10.2) | 807 (89.8) | |
| Tobacco smoking history | |||
| Intermittent smoking | 0.418 | ||
| Yes | 1 (20) | 4 (80) | |
| No | 91 (10.2) | 804 (89.8) | |
| Light smoking | 0.054 | ||
| Yes | 2 (50) | 2 (50) | |
| No | 90 (10) | 806 (90) | |
| Heavy smoking | 1 | ||
| Yes | 0 (0) | 1 (100) | |
| No | 92 (10.2) | 807 (89.8) | |
| Former regular smoking | 0.084 | ||
| Yes | 2 (50) | 2 (50) | |
| No | 90 (10.1) | 805 (89.9) | |
| Former irregular smoking | 1 | ||
| Yes | 0 (0) | 1 (100) | |
| No | 92 (10.2) | 807 (89.8) | |
| Heavy hookah | 1 | ||
| Yes | 0 (0) | 1 (100) | |
| No | 92 (10.2) | 807 (89.8) |
a Values are expressed as No. (%).
b Fisher's Exact test; significance level P-value < 0.05.
5. Discussion
The purpose of the current study was to determine the effect of opioid and tobacco consumption on the outcomes of COVID-19 patients, including an analysis of specific subgroups of tobacco and opioid users. The study found no association between the number of hospital days, the duration of hospitalization in the intensive care unit (ICU), and opioid use. Furthermore, no statistically significant relationship was found in any of the subgroups of opioid users or tobacco users in terms of death or discharge.
However, cardiovascular diseases, airway diseases, and multiple coexisting diseases were significantly higher in opioid users than in other patients. The WHO reports that a significant number of COVID-19-related deaths are linked to comorbidities (20, 21).
Opium use was reported in 36 patients (6.5%) in Riahi et al.’s study in Tehran (Iran), whereas the opioid use rate was 3.2% in our study. This difference may be related to the data collection method. Additionally, the prevalence of substance use varies across different provinces in the country (10). There was no significant difference between the groups in terms of mean hospitalization days in that study, which is consistent with our findings. The need for hospitalization in the ICU was significantly higher in opium users in Riahi et al.’s study (10), but this was not observed in our study.
The percentage of patients with fever, anosmia/hyposmia, and dysgeusia at the beginning of hospitalization was lower in opium users in Riahi et al.’s study (10). In our study, only fatigue was significantly lower in opioid users, and no significant differences were found in other initial symptoms and signs of patients. In laboratory tests, only the number of WBCs was higher in the opium users in Riahi et al.’s study. Segmented cells were more and lymphocyte cells were fewer in the opium users in their study. However, no relationship was found in any of the initial laboratory tests in our study. Regarding these tests, only the ESR was significantly lower in tobacco smokers among our patients.
The effect of tobacco was not investigated in that study (10). In Wang et al.'s study in the USA, 15.63% of the participants had substance use disorders (SUD). Among those patients, 52% were male. In our study, all tobacco smokers were male, and among opioid user patients, 89.7% were male. The study found that 1.75% of participants had opioid use disorders (OUD) and 12.22% had tobacco use disorder (TUD). In our study, the prevalence of OUD was 3.2% and TUD was 1.9%, which is higher for OUD but much lower for TUD compared to Wang et al.'s study (22). This difference in the percentage of opium use can be attributed to the different patterns of common substance consumption between Iranian and American consumers. The higher smoking rates in the USA are also justified by the fact that in Iran, female consumers are very few compared to men (23), or if they do smoke, they hide their consumption due to cultural characteristics.
In Wang et al.'s study, the use of opium and tobacco was stated in general (22), and the subgroups that were examined in our study were not examined in their study. Wang et al.'s patients with a recent diagnosis of SUD (within the last year) were at significant risk for COVID-19, with a higher risk observed in OUD patients than in other patients, followed by those with TUD. Additionally, patients with SUD had a significantly higher prevalence of chronic kidney disease, chronic liver disease, lung disease, cardiovascular disease, type 2 diabetes, obesity, and cancer than patients without SUD. However, in our study, only cardiovascular disease, airway disease, and multiple coexisting diseases were significantly higher in opioid patients than in other patients, and none of the coexisting diseases were significantly different between tobacco smokers and non-smokers. Furthermore, COVID-19 patients with SUD had significantly worse outcomes than general COVID-19 patients (22). In our study, the death rate was higher among smokers.
The effect of tobacco smoking on the incidence of COVID-19 and its comparison with non-smokers was examined in a review study by Ghoshooni et al. They concluded that people who smoke are much more likely to experience harmful respiratory effects or even death from COVID-19 (24). Cigarette smoking increases the expression of the ACE2 receptor, the entry point for the coronavirus, on the surface of the respiratory epithelium, such as the epithelium covering the airways and air sacs. Therefore, the entry of the coronavirus may intensify the stimulating effects of the immune system, leading to a more severe cytokine storm and greater destruction of epithelial cells, which eventually exacerbates the infection by disrupting the body's homeostasis-stabilizing mechanisms.
In that review article, it was stated that about 1.4% to 18% of hospitalizations for COVID-19 were tobacco smokers (24). In our study, the percentage of tobacco smokers was 1.9%, which is consistent with the findings mentioned in that study.
Clift et al., in their study on tobacco smokers, reported that recent smoking status based on primary care records and UK Biobank questionnaire data was 70.8% and 29.2%, respectively. The mean age of the participants was 68.6 years, and most of them were female (55.1%), which did not match our results in terms of gender. The researchers found that current tobacco smoking was associated with higher risks of hospitalization and mortality associated with COVID-19. This finding was not consistent with our study. In addition, the number of cigarettes smoked per day was associated with higher risks for all outcomes (infection, hospitalization, and death). One of the strengths of their study was that, like ours, they distinguished between different types of smokers (never smoking, former smoker, light smoker, medium smoker, and heavy smoker) (25).
In the study by Sohrabi et al. (26) in Tehran province, Iran, 1.5% of patients had a history of tobacco smoking, and 86.7% were male. This prevalence was consistent with our study (1.9%). However, in our study, all tobacco smokers were male, which may be explained by differences in the statistical community. Sociocultural and economic issues in different provinces of the country may account for the finding of more women smokers in that study. Of the 0.9% of patients with a history of opioid use, 84% were male. These results are inconsistent with our study, which found a prevalence of 3.2% opioid use, 89.7% of whom were male. Social, cultural, and economic issues may also have influenced this results.
There were 1522 (48.2%) patients with oxygen saturation (SpO2) ≤ 93% and 1634 (51.8%) patients with SpO2 > 93%, with 10% deaths in patients with a positive history of tobacco smoking. None of these differences were significantly related to tobacco smoking. In our study, the mean SpO2 in the tobacco smokers was 93.00 ± 4.61, and in the non-tobacco smokers, it was 93.50 ± 7.11, which was not significantly related to tobacco smoking in line with that study. However, the findings regarding the outcome of tobacco smoking were not consistent with our study; the relationship between smoking and the outcome of the disease was statistically significant in our study.
56.5% of patients with SpO2 ≤ 93% and 43.5% of patients with SpO2 > 93%, and 14.5% of deaths and 85.5% of survivors in patients were significantly seen in patients with a positive history of opioid use. These findings are completely inconsistent with our study, where no significant relationship was found in the mean SpO2 and death in the two groups of opioid users and non-opioid users. Contrary to our study, Sohrabi et al.'s study did not distinguish between different types of tobacco smoking and opium consumption (26).
Due to the lack of registration of all patients’ information in the registry system, the required information was completed by phone call. Despite providing a full explanation of the study's purpose, some patients were reluctant to respond accurately for various reasons, such as lack of trust in phone calls, dissatisfaction with their treatment, or grief over their patient's death. Consequently, they may not have given completely correct answers, or they were unaware of the consumption type and amount of opioid and tobacco use in their deceased patient. If the information about opioid and tobacco use had been obtained during hospitalization, a face-to-face visit with the patients and their companions, compliance with laboratory data, and the patient's clinical condition would have made the information more reliable.
The main limitation of the study, which diverted us from our main goal, was the limited number of subtypes of tobacco and opium use.
5.1. Conclusions
Although death and comorbidities were more common in tobacco and opium users with COVID-19, these outcomes were not related to the amount of substance consumption. Therefore, in a situation where the world is exposed to different mutations of COVID-19, the use of any amount of tobacco and opium should be considered a risk factor.