1. Background
According to the World Health Organization (WHO), more than 700 000 people commit suicide each year, with 10 to 20 times as many attempting suicide (1). Suicide accounts for approximately 8.5% of mortality among adolescents and young adults, making it the second leading cause of death in the age group of 15 to 29 years old (2). Suicide patterns in some provinces of Iran show that the number of adolescents committing suicide has been increasing since 1990, which has garnered significant attention in recent years (3). Suicide rates among adolescents have increased fourfold over the past 40 years, now making it the second leading cause of death in this age group, after events such as accidents. It is estimated that 10 - 15% of adolescents experience suicidal ideation (4). This phenomenon can have various consequences, such as disability and physical impairment, which increases the cost of treatment for this age group, leads to higher crime rates, and limits access to education, thus exacerbating existing societal problems (5).
While the focus on suicide risk factors has not significantly improved our understanding of suicide or its prevention, a greater focus on protective factors may be an appropriate and important direction for the development and reevaluation of psychological interventions (6). One area that has received less attention in adolescent research is resilience to suicide (7). Suicide resilience is defined as the capacity and dynamic process of maintaining mental and physical health when the risk of suicide is high (8). The concept of suicide resilience, proposed by Osman et al. (9), refers to an individual's perceived ability to cope with suicidal thoughts, the availability of external resources, and the ability to manage negative events. This concept was primarily derived from observations of people at risk of suicide, particularly those suffering from depression (10) or suicidal ideation (11), who did not engage in suicidal behavior. Most current research on suicide resilience is based on the buffering hypothesis (12), which is used to identify psychological constructs that moderate the relationship between suicide risk and suicidal behavior (13). However, this approach is often limited by relatively small effect sizes for interaction effects (2 - 5%) and shows inconsistent findings across studies. In contrast, a person-centered approach (identifying resilient individuals) demonstrates the constancy of resilience over time (14).
Positive deviance (PD) is a person-centered research approach that holds great promise in unraveling the relationship between suicide risk and suicidal behaviors. This approach has proven useful in identifying and understanding the specific behaviors of individuals with complex health conditions (15). The PD approach is based on the evidence that in every society, there are certain individuals whose abnormal behaviors and strategies allow them to find better solutions to similar problems than their peers (7). In this study on suicide resilience, we followed a common process to first define the problem. As theorized (16) and supported by empirical literature, the transition from suicidal ideation to suicidal behavior is increasingly recognized as an important predictor of death by suicide. Our goal is to understand the factors that increase resilience to suicidal behavior in adolescents (7). Thus, according to the literature, this research is the first to attempt to understand resilience to suicide in adolescents, using a descriptive approach based on a model of vulnerability and subsequent growth, in line with the differential activation theory (17) and Shneidman’s model of psychological pain (18).
Psychological pain, also called "psychache" (18), is severe acute psychological pain associated with the negative cognitive and emotional aspects of oneself. It is accompanied by feelings of helplessness, incompetence, sadness, guilt, fear, panic, anger, loneliness, and hopelessness, along with the perception of separation from oneself (19). Thus, although the severity of psychological pain seems to be associated with worsening psychological distress and suicide, results indicate that tolerance and resilience to psychological pain act as protective factors. The findings of this study, therefore, increase our understanding of protective factors that can be used to improve suicide prevention interventions and promote suicide intervention approaches that are developed based on evidence-based strategies.
One area that requires further investigation regarding the path from suicidal ideation to suicidal behavior is cognitive (20) and emotional (21) reactivity. Cognitive reactivity refers to the degree of arousal of ineffective thoughts and attitudes that produce negative and depressive moods (20). The differential activation model of cognitive reactivity suggests that hopelessness and suicidal ideation first emerge as negative thought features in the early stages of depression. During these periods, links are formed between depressed mood and hopelessness/suicidal ideation, leading to the activation of these thought patterns whenever depressive moods occur again (22). In this way, hopelessness/suicide becomes part of the “configuration” of associations and feedback loops in the information processing system. In fact, this pattern enters the “rehearsal pool,” which is activated with each subsequent depressive episode. After several episodes, the recurrence of mood serves as a “relapse” (reinstatement), similar to the process observed in the development of CS- cognitive reactivity (CR) associations in animal conditioning studies (23). In summary, the differential activation model indicates that it is not the resting level of hopelessness/suicidal cognitions that is important in predisposing a person to a future suicidal crisis; rather, what matters is the susceptibility to the activation of these thought patterns (20).
Thus, according to this model, the traits that increase the likelihood of suicidal behavior include aggression, impulsivity, pessimism, hopelessness, impaired cognitive functioning, and emotional dysregulation (24). The results of the study by Akpinar Aslan et al. (25) indicate that the suicide attempts of students can be predicted based on cognitive styles, hopelessness, cognitive reactivity, rumination, self-esteem, and personality traits. Higher scores on ruminative response, hopelessness, and cognitive style, as well as lower scores on the ten-item personality inventory and Rosenberg self-esteem scale, were significantly associated with a previous suicide attempt. Negative cognitive style, hopelessness, and rumination were significant correlates of a previous suicide attempt.
Although the association between cognitive reactivity and suicidality in depression (26) and suicide (25) has been studied, its relationship with protective factors has been overlooked in the research literature. Therefore, identifying the psychological, social, and behavioral profiles of adolescents through elements of cognitive reactivity may be crucial for formulating treatment goals and developing strategies for the prevention and intervention of suicidal ideation. The novelty of this study lies in addressing this research gap, aiming to demonstrate the theoretical foundations and apply them in clinical settings for assessment, prevention, and intervention.
The stress-diathesis model posits that stressors interact with neurological and psychological predispositions to cause suicidal behavior, resulting in a maladaptive stress response (27). Chronic and acute stress situations, such as deprivation, isolation, family adversity, sexual abuse, and educational, occupational, and economic problems, as well as experiences of loss and death, can increase the likelihood of suicidal behavior (28). Data show that early negative life experiences are more traumatic and increase the rate of impulsive and suicidal behaviors by 2 - 5 times (29). Bagian Kulehmarzi et al. demonstrated that early life experiences, temperament and personality dimensions, and psychological pain are the strongest predictors of suicide attempts (30). Furthermore, in a study by Rajabi et al., it was found that psychological pain, psychological vulnerability, and childhood experiences explained 81% of the variance in suicide attempts during the COVID-19 pandemic (31).
In general, the development of a structural model in adolescent populations—considering distal factors such as age, gender, early negative experiences, and one’s and their families’past behavioral history, along with proximal factors like psychological pain and cognitive reactivity—can provide a clear psychological understanding of the antecedents and mediators of resilience to suicide. Thus, suicide resilience moderates the relationship between these factors and suicidal ideation. Therefore, this study was conducted to model a structural equation involving cognitive reactivity and early life experiences with resilience to suicide, while considering the mediating role of psychological pain.
2. Objectives
In general, an important step in preventing suicide attempts is the study of protective factors and suicide risk in adolescents, as well as the use of theory-based structural models in these populations. Given the biological, cognitive, and emotional changes that are typical for their age, alongside the increasing prevalence of suicidal ideation and attempts, it is crucial to identify both protective and risk factors. This study aimed to develop a structural model distinct from other research models conducted in Iran and, particularly, in Western countries with higher suicide rates. This model could help experts in applying and adapting preventive programs, interventions, and treatments. Therefore, this study seeks to answer the following questions:
(1) Does cognitive reactivity have a negative and direct effect on resilience against suicide?
(2) Do early life experiences have a negative and direct effect on resilience against suicide?
(3) Does psychological pain have a negative and direct effect on resilience against suicide?
(4) Does cognitive reactivity, through psychological pain, have a negative and indirect effect on resilience against suicide?
(5) Do early life experiences, through psychological pain, have a negative and indirect effect on resilience against suicide?
Given that suicide is the second leading cause of death among adolescents aged 10 to 24 years, this study focused on at-risk groups, including adolescents who may be struggling with maturation experiences, school-related issues, family conflicts, peer pressure, and other challenges. While previous research has primarily focused on adulthood, investigating risk and protective factors in this age group will contribute to a deeper understanding of both theoretical and empirical evidence in the field of adolescent suicide.
3. Materials and Methods
3.1. Participants and Procedures
This cross-sectional study was conducted using an analytical correlational method with structural equation modeling. The statistical population of this study consisted of all high school students in Lorestan province during the academic year 2023. A total of 300 first- and second-grade students in Lorestan province were selected using a multistage cluster sampling method. Initially, each city was considered a cluster. From the 11 cities in the province, four cities were randomly selected: Khorramabad, Nourabad, Kohdasht, and Aleshatar. Afterward, two schools from each city were chosen, and two classes (20 students per class) from each school were selected. A link to the online questionnaire was provided to the students (20 students × 16 classes = 320 total students).
The inclusion criteria were: (1) Signed consent forms from both students and their parents; (2) age between 15 and 19 years; and (3) no physical disabilities or chronic illnesses requiring medications for physical or mental conditions. All inclusion criteria were verified based on students' consultation files and the forms filled out at the beginning of the survey. The exclusion criteria included: (1) Unwillingness to participate in the study; (2) hospitalization within the past 6 months due to mental or physical conditions; and (3) incomplete or inconsistent responses to the survey.
Data collection occurred only after obtaining informed consent from both parents and students. Students were given a clear and concise explanation of the study's purpose, potential risks, and the accessibility of results. The necessary information was provided during the information session. Participation in the study was entirely voluntary, and the confidentiality of information and anonymity of identities were assured.
According to Soper's formula (32) for structural equation modeling with an effect size of 0.20, a power of 0.80, 4 latent variables, 16 observable variables, and an error rate of 0.05, the minimum sample size was estimated to be 100, with a maximum of 342. In this study, 300 valid data sets were included in the final analysis.
3.1.1. Leiden Index of Depression Sensitivity-Revised
The Leiden Index of depression sensitivity-revised (LEIDS-R) consists of 34 items and is an effective tool for therapists and researchers to assess CR to sad moods. This self-report scale includes six subscales, with higher scores indicating higher levels of CR to depression (33). Each item is rated on a five-point Likert scale ranging from 0 = ‘not at all’ to 4 = ‘very strongly,’ with higher scores reflecting a stronger CR to sad moods. The subscales are as follows:
- Aggression/hostility (AGG): Items 7, 8, 21, 22, 26, and 29
- Acceptance/coping (COP): Items 4, 10, 15, 24, and 28
- Hopelessness/suicidality (HOP): Items 5, 9, 17, 30, and 34
- Risk aversion (RAV): Items 1, 2, 11, 14, 23, and 34
- Control/perfectionism (CON): Items 3, 6, 12, 16, 19, 31
- Rumination (RUM): Items 13, 20, 25, 27, 32, and 33
All subscales are considered psychological vulnerability factors for depression. The LEIDS-R total score is derived by summing the scores from each subscale, with total scores ranging from 0 to 136. Internal consistency for the LEIDS total score is 0.89, and the subscales range from 0.62 (acceptance/coping) to 0.84 (34). The Iranian version of the LEIDS-R was used in this study, and its Cronbach’s α was 0.90 (35).
An example of a question from this questionnaire is: "I can only think positively when I am in a good mood."
3.1.2. Early Life Experiences Scale (ELES)
Gilbert et al. developed a 15-item tool in 2003 to assess early traumatic experiences. This questionnaire includes subscales such as threat (Items 4, 8, 11, 13, 14, and 15), submissiveness (Items 1, 2, 3, 5, 10, and 15), and unvalued (Items 6, 7, and 9). The response measure consists of a Likert-type Scale, with participants required to rate how frequently and how true each statement was for them in their childhood: (1 = completely untrue, 2 = very occasionally true, 3 = sometimes true, 4 = fairly true, 5 = very true). Gilbert et al. found good reliability with Cronbach’s alphas: Submissiveness 0.85, threat 0.89, (un) valued 0.71, and 0.92 for the total score (36). Its three-factor structure is suitable for Iranians, with Cronbach's alpha values for the subscales submissiveness, feeling unvalued/valued, and feeling threatened being 0.74, 0.85, 0.66, and 0.80, respectively (37). An example item for the perceived threat subscale is: "In order to avoid getting hurt, I used to try to avoid my parents."
3.1.3. Suicide Resilience Inventory-25
The Suicide Resilience Inventory-25 (SRI-25) was developed by Osman et al. and was used in a study to investigate types of resilience to suicide (9). In our study, we measured its three subscales: Internal protective (IP) (items 1 - 10), emotional stability (ES) (items 11 - 19), and external protective (EP) (items 20 - 25), with higher scores indicating higher levels of resilience. The questionnaire uses a 6-point Likert Scale (1 = strongly disagree to 6 = strongly agree). The literacy level required to answer the questionnaire is at least 7th or 8th grade.
Osman et al. reported that this inventory has moderate to high internal consistency reliability estimates and an established factor structure (9). Studies conducted using this tool have shown it has good validity and reliability in different populations, such as African American students and inpatient adolescents (α = 0.96; average interitem correlation (AIC) = 0.49) (38). Additionally, the alpha estimates for the Internal Protective, Emotional Stability, and External Protective Scales were 0.94 (mean interitem correlation = 0.63), 0.93 (mean interitem correlation = .62), and 0.90 (mean interitem correlation = 0.57), respectively (9). An example question from this scale is: "People close to me would find the time to listen if I were to talk seriously about killing myself."
3.1.4. Orbach & Mikulincer Mental Pain Scale (OMMP)
We used a questionnaire developed by Orbach et al. to assess the severity of mental pain (39). The factors include the experience of irreversibility (nine items; e.g., "The pain will never go away"), loss of control (ten items; e.g., "I have no control over the situation"), narcissistic wounds (five items; e.g., "I am rejected by everybody"), emotional flooding (four items; e.g., "There are strong ups and downs in my feelings"), freezing (three items; e.g., "I feel paralyzed"), estrangement (three items; e.g., "I am a stranger to myself"), confusion (three items; e.g., "I have difficulties in thinking"), social distancing (four items; e.g., "I don’t feel like talking to other people"), and emptiness (three items; e.g., "I can’t find meaning in my life"). Participants rated each statement on a 5-point Likert scale (1 = strongly disagree, 2 = disagree, 3 = agree to some extent, 4 = agree, 5 = strongly agree).
The lowest test-retest coefficient for the nine subscales was 0.79, and the highest was 0.94. Good convergent validity has been reported for this questionnaire, as all its subscales showed significant relationships with depressive and anxious cognitions (r’s ranged between 0.26 and 0.64 for depression and between 0.27 and 0.50 for anxiety). However, this relationship was not reported for the social distancing subscale (39). In the study by Karami et al., Cronbach’s alpha for the scale as a whole and for its subscales ranged between 0.61 (the lowest for freezing) and 0.96 (the highest for the total score). Its convergent validity was reported as 0.43 (40). In our study, Cronbach’s alpha was 0.96.
3.2. Statistical Analysis
In this study, SPSS 26 for Social Sciences was used for data analysis. Before analyzing the data, it was first checked for accuracy. The assumption of normality was then tested using skewness and kurtosis statistics. Based on the absolute values of -3 and +3, the normality assumption of the research data was confirmed. The assumption of linearity for the research variables was examined using scatter plots. The independence of residuals in the regression model was verified using Durbin-Watson statistics, and since the independence of residual errors was within the range of -2 to +2, the assumption was met. Outlier data were analyzed using box plots, and final analyses were conducted on 300 data points after removing the top and bottom 20 data points. Multicollinearity was assessed using variance inflation factors and tolerance statistics. The assumption was met, as the values ranged from 0.1 to 5. Additionally, for confirmatory factor analysis, AMOS software was used with the maximum likelihood method, and a P-value of < 0.05 was considered significant. The study data were analyzed in two parts: Descriptive analysis (prevalence, percentages, mean, standard deviation, minimum and maximum values, skewness, and kurtosis) and inferential analysis (correlation coefficients and structural equation modeling).
4. Results
Table 1 presents the participants' demographic characteristics.
| Variables | Values a |
|---|---|
| Sex | |
| Male | 145 (48.3) |
| Female | 155 (51.7) |
| Age (y) | |
| 15 | 70 (23.3) |
| 16 | 80 (26.7) |
| 17 | 80 (26.7) |
| 18 | 50 (16.7) |
| 19 | 20 (6.7) |
| Mean age (y) | 17.01 ± 2.89 |
| Grade point average | 16.69 ± 3.48 |
a Values are expressed as mean ± SD or No. (%).
The mean age of the participants was 17.01 ± 2.89 years, with 48.3% male and 51.7% female. Among the students, 70 (23.3%) were 15 years old, 80 (26.7%) were 16 years old, 80 (26.7%) were 17 years old, 50 (16.7%) were 18 years old, and 20 (6.66%) were 19 years old. The mean score of the students was 16.69 (± 3.48) (Table 1).
The mean, standard deviation, and normality assumptions (skewness and kurtosis tests) for the research variables are presented in Table 2.
| Variables | Mean ± SD | Skewness | Kurtosis | Min - Max |
|---|---|---|---|---|
| HS | 14.23 ± 4.63 | -0.68 | -0.34 | 3 - 20 |
| Rumination | 14.30 ± 4.07 | -0.34 | -0.14 | 4 - 24 |
| Risk aversion | 12.04 ± 3.17 | -0.64 | 0.14 | 3 - 19 |
| Aggression/hostility | 15.23 ± 3.52 | -0.54 | 0.34 | 2 - 21 |
| CR | 55.82 ± 13.35 | -0.74 | 0.35 | 13 - 80 |
| Threat | 19.97 ± 5.47 | -0.39 | -0.50 | 6 - 30 |
| Unvalued | 11.27 ± 2.77 | -0.87 | 0.42 | 3 - 15 |
| Submissiveness | 19.62 ± 5.12 | -0.83 | 0.07 | 6 - 30 |
| ELE | 50.87 ± 11.62 | -0.77 | 0.05 | 19 - 71 |
| Emptiness | 47.24 ± 11.69 | -0.956 | 0.73 | 14 - 68 |
| Emotional flooding | 24.76 ± 5.64 | -1.05 | 1.06 | 7 - 35 |
| Loss of control | 20.51 ± 5.13 | -0.971 | 0.73 | 6 - 29 |
| Irreversibility | 24.37 ± 5.80 | -1.01 | 0.62 | 7 - 33 |
| SD | 20.29 ± 4.74 | -1.03 | 1.34 | 6 - 29 |
| Freezing | 12.49 ± 3.01 | 0.18 | 0.04 | 4 - 20 |
| PP | 149.53 ± 32.02 | -1.22 | 1.61 | 44 - 205 |
| Internal protective | 23.95 ± 9.17 | 1.35 | 2.62 | 10 - 60 |
| Emotional stability | 21.96 ± 9.29 | 1.35 | 2.67 | 9 - 54 |
| External protective | 15.41 ± 5.76 | 1.20 | 2.08 | 6 - 36 |
| SRI | 60.66 ± 21.86 | 1.53 | 3.12 | 25 - 150 |
Abbreviations: HS, hopelessness/suicidality; ELE, early life experiences; CR, cognitive reactivity; SD, social distancing; PP, psychological pain; SRI, Suicide Resilience Inventory.
As seen in Table 2, the means and standard deviations (mean ± SD) of the CR variables were 55.82 ± 13.35, early life experiences (ELE) were 50.87 ± 11.62, psychological pain was 149.53 ± 32.02, and resilience to suicide attempts (SRI) was 60.66 ± 21.86, respectively. All bivariate associations were either positive or negative in direction, with moderate to large effect sizes. A simple correlation analysis revealed that CR was positively associated with psychological pain (r = 0.70, P < 0.01) and negatively associated with SRI (r = -0.50, P < 0.01). Early life experiences was positively associated with psychological pain (r = 0.77, P < 0.01) and negatively associated with SRI (r = -0.72, P < 0.01). Additionally, psychological pain was negatively associated with SRI (r = -0.78, P < 0.01) (Table 3).
| Variables | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 17 | 18 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| HS | - | ||||||||||||||||||
| Rumination | 0.78 a | - | |||||||||||||||||
| Risk aversion | 0.60 a | 0.60 a | - | ||||||||||||||||
| Aggression/hostility | 0.66 a | 0.69 a | 0.64 a | - | |||||||||||||||
| CR | 0.66 a | 0.78 a | 0.60 a | 0.89 a | - | ||||||||||||||
| Threat | 0.70 a | 0.53 a | 0.47 a | 0.47 a | 0.64 a | - | |||||||||||||
| Unvalued | 0.48 a | 0.31 a | 0.14 b | 0.12 b | 0.31 a | 0.48 a | - | ||||||||||||
| Submissiveness | 0.67 a | 0.53 a | 0.45 a | 0.34 a | 0.58 a | 0.75 a | 0.51 a | - | |||||||||||
| ELE | 0.74 a | 0.55 a | 0.46 a | 0.40 a | 0.63 a | 0.91 a | 0.69 a | 0.91 a | - | ||||||||||
| Emptiness | 0.75 a | 0.56 a | 0.49 a | 0.49 a | 0.67 a | 0.72 a | 0.62 a | 0.69 a | 0.79 a | - | |||||||||
| Emotional flooding | 0.68 a | 0.54 a | 0.51 a | 0.54 a | 0.66 a | 0.63 a | 0.52 a | 0.53 a | 0.65 a | 0.81 a | - | ||||||||
| Loss of control | 0.62 a | 0.48 a | 0.44 a | 0.39 a | 0.57 a | 0.61 a | 0.57 a | 0.64 a | 0.70 a | 0.81 a | 0.80 a | - | |||||||
| Irreversibility | 0.65 a | 0.53 a | 0.47 a | 0.46 a | 0.62 a | 0.63 a | 0.54 a | 0.60 a | 0.69 a | 0.84 a | 0.85 a | 0.82 a | - | ||||||
| SD | 0.62 a | 0.48 a | 0.40 a | 0.41 a | 0.56 a | 0.62 a | 0.51 a | 0.58 a | 0.67 a | 0.81 a | 0.73 a | 0.76 a | 0.77 a | - | |||||
| Freezing | 0.44 a | 0.44 a | 0.53 a | 0.56 a | 0.57 a | 0.41 a | NS | 0.31 a | 0.34 a | 0.39 a | 0.52 a | 0.40 a | 0.48 a | 0.43 a | - | ||||
| PP | 0.74 a | 0.59 a | 0.54 a | 0.53 a | 0.70 a | 0.72 a | 0.59 a | 0.67 a | 0.77 a | 0.94 a | 0.91 a | 0.89 a | 0.93 a | 0.88 a | 0.54 a | - | |||
| Internal protective | -0.58 a | -0.32 a | -0.23 a | -0.21 a | -0.41 a | -0.49 a | -0.63 a | -0.57 a | -0.63 a | -0.73 a | -0.62 a | -0.73 a | -0.65 a | -0.62 a | -0.12 b | -0.71 a | - | ||
| Emotional stability | -0.66 a | -0.44 a | -0.37 a | -0.31 a | -0.53 a | -0.64 a | -0.61 a | -0.63 a | -0.73 a | -0.78 a | -0.68 a | -0.71 a | -0.70 a | -0.71 a | -0.33 a | -0.78 a | 0.78 a | - | |
| External protective | -0.52 a | -0.31 a | -0.26 a | -0.24 a | -0.40 a | -0.45 a | -0.49 a | -0.52 a | -0.56 a | -0.57 a | -0.46 a | -0.62 a | -0.55 a | -0.49 a | -0.25 a | -0.59 a | 0.63 a | 0.68 a | - |
| SRI | -0.66 a | -0.41 a | -0.32 a | -0.29 a | -0.50 a | -0.60 a | -0.65 a | -0.65 a | -0.72 a | -0.79 a | -0.67 a | -0.77 a | -0.72 a | -0.69 a | -0.26 a | -0.78 a | 0.92 a | 0.93 a | 0.82 a |
Abbreviations: HS, hopelessness/suicidality; ELE, early life experiences; CR, cognitive reactivity; SD, social distancing; PP, psychological pain; SRI, Suicide Resilience Inventory; NS, not significant.
a P < 0.01.
b P < 0.05.
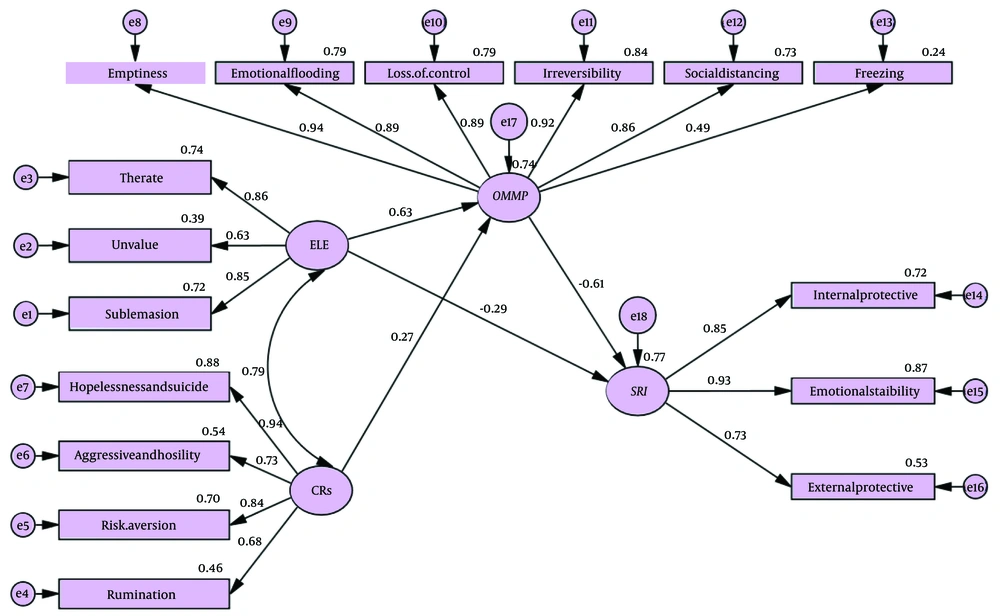
In Figure 1, the direct and standardized path coefficients of the cognitive reactivity variables and early life experiences, with resilience to suicide attempts mediated by psychological pain, are displayed.
The structural model results indicated an adequate model fit (CMIN/DF = 6.062, CFI = 0.90, RMSEA = 0.08, TLI = 0.89, GFI = 0.88, IFI = 0.90, RMR = 0.88, NFI = 0.89, RFI = 0.87) (Figure 1). Cognitive reactivity negatively predicted SRI-25 (β = -0.28, P < 0.001), ELE negatively predicted SRI-25 (β = -0.33, P < 0.001), and psychological pain negatively predicted SRI (β = -0.80, P < .001). The results indicated that both CR and ELE positively predicted psychological pain. According to Figure 1, 74% of the variance in psychological pain is explained by cognitive reactivity and early life experiences. Additionally, 79% of the variance in resilience to suicide is explained by cognitive reactivity, early life experiences, and negative psychological pain (Figure 1). In Table 4, the direct, indirect, and total variables of the research are presented.
| Direct effect | Effect (β) | Unstandardized | SE | CR | Lower Bounds | Upper Bounds | P-Value |
|---|---|---|---|---|---|---|---|
| CR → MP | 0.263 | 1.241 | 0.351 | 3.535 | 0.134 | 0.419 | 0.001 |
| CR → SRI | -0.174 | 0.688 | 0.272 | 2.530 | -0.123 | -0.445 | 0.019 |
| ELE → MP | 0.639 | 1.564 | 0.205 | 7.637 | 0.464 | 0.768 | 0.001 |
| ELE → SRI | -0.410 | -0.502 | 0.175 | -2.877 | -0.524 | -0.156 | 0.004 |
| MP → SRI | -0.650 | -0.551 | 0.061 | -9.039 | -0.969 | -0.646 | 0.001 |
Abbreviations: ELE, early life experiences; CR, cognitive reactivity; SRI, Suicide Resilience Inventory; MP, mental Pain.
As shown in Table 4, the coefficient for the direct path from cognitive reactivity to psychological pain is β = 0.263, P < 0.05, and to suicide resilience is β = -0.174, P < 0.05. The coefficient for the direct path from early life experiences to psychological pain is β = 0.639, P < 0.05, and to suicide resilience is β = -0.410, P < 0.05. Additionally, the coefficient for the direct path from psychological pain to suicide resilience is β = -0.650, P < 0.05.
| Variables | Effect (β) | SE | Lower Bounds | Upper Bounds | P-Value |
|---|---|---|---|---|---|
| Indirect effect | |||||
| CR → MP→ SRI | -0.164 | 0.056 | -0.261 | -0.080 | 0.003 |
| ELE → MP → SRI | -0.390 | 0.084 | -0.555 | -0.277 | 0.001 |
| Total effect | |||||
| CR→ MP | 0.266 | 0.085 | 0.133 | 0.408 | 0.003 |
| CR→ SRI | -0.164 | 0.056 | -0.261 | -0.080 | 0.003 |
| ELE→ MP | 0.634 | 0.089 | 0.475 | 0.771 | 0.002 |
| ELE → SRI | -0.681 | 0.066 | -0.786 | -.569 | 0.001 |
| MP → SRI | -0.615 | 0.089 | -0.759 | -0.467 | 0.001 |
Abbreviations: ELE, early life experiences; CR, cognitive reactivity.
In Table 5, the indirect effects are reported along with the lower and upper bounds of standard errors and significance levels. The results indicate that early life experiences and cognitive reactivity have significant indirect relationships with suicide resilience via psychological pain.
5. Discussion
The aim of this research was to develop a structural model of cognitive reactivity and early life experiences in relation to resilience to suicide attempts, with psychological pain as a mediator. The results of SEM showed that early life experiences had a direct and indirect negative and significant effect on resilience to suicide, through psychological pain. These findings are consistent with studies by Bagian Kolehmarzi et al. (30) and Rajabi et al. (31). In their research, they concluded that childhood experiences and psychological pain were significant predictors of suicide attempts and the motivations behind them (31). The study empirically emphasizes that suicide resilience plays a crucial role in regulating suicidal ideation and attempts in adolescents. Individuals' passive responses to the psychological pain resulting from early life experiences, their reduced ability to cope with and tolerate the pain caused by early trauma, and their attempts to suppress these experiences may lead to feelings of hatred and rumination. These emotional challenges, along with impairments in daily activities, can reduce resilience when faced with life stressors (30).
The results of the SEM showed that cognitive reactivity, indirectly through psychological pain, has a negative and significant effect on resilience against suicide. These findings are consistent with the study by Akpinar Aslan et al. (25). In fact, individuals with high cognitive reactivity initially struggle to tolerate emotions and cope with stress and psychological distress. When these individuals experience pain caused by unmet psychological needs, they become stressed and unable to manage the stressor. A lack of emotion regulation skills forms the basis of psychological burden as the third component of pain. Thus, the experience of pain, distress, and perceived pressure creates a situation that becomes intolerable and uncontrollable. These individuals also have difficulty identifying, recognizing, and expressing their emotions. Without the appropriate skills and ability to manage their emotions, they are likely to feel embarrassed and distressed when reacting to any stimulus or event. Since cognition and emotion are two sides of the same coin, such individuals will exhibit both emotional and cognitive reactions (internal and external) to even the smallest disturbing stimuli, such as anger, aggression, hostility, despair, and rumination (24). Therefore, cognitive reactions to negative emotional experiences may contribute to intolerance to pain, distress, and diminished resilience.
When designing prevention and clinical intervention programs for adolescents, it is important to consider their psychological profiles, including their early life experiences, cognitive reactivity, and psychological distress, to better understand the likelihood of suicide attempts. A systematic assessment of cognitive reactivity, early life experiences, and psychological pain can enhance our understanding of the underlying mechanisms of suicidal ideation and suicide attempts. This can facilitate the development of appropriate treatment approaches, such as cognitive-behavioral therapy. Finally, this study has significant clinical implications. Since this is a cross-sectional study on the antecedents of resilience to suicide, the students' current cognitive profiles may offer insights into some of their personality traits, rather than reflecting changes in their affect. Thus, targeting rumination, hopelessness, hostility, aggression, threats, and devaluation may have a protective effect against suicide attempts, even in students who do not have a mental illness.
This study has several strengths and weaknesses. One strength is that our data included a large sample of adolescents aged 15 to 19 years. By focusing on psychological constructs and evaluating a structural model for adolescents, this study contributes to a better understanding of the pathology of their suicidal behavior. However, a limitation of our study is that it relied solely on a self-assessment tool, a questionnaire, which may introduce bias. It would have been beneficial to incorporate interviews and behavioral scales as additional methods. Furthermore, the multi-part nature of this study and its focus on multiple theories may have introduced bias, making it challenging to establish causal relationships. Since our study is cross-sectional, we cannot infer causal relationships in this field. Additionally, all participants were selected from adolescents aged 15 - 19 in Lorestan province, limiting the generalizability of the results to the entire country. Future studies are recommended to include other factors and to examine this model in more detail. This model was conducted for the first time in Iran, and further research is needed to explore it more comprehensively. Future studies could also replicate this investigation on a larger scale and across different population groups.
5.1. Conclusions
Identifying risk and protective factors for suicide in adolescents can help in the development of prevention and intervention programs for at-risk individuals. Based on the results of this study, which considered several theoretical models in the fields of suicide, resilience to suicide (9), psychological pain (18), and early life experiences, new insights are provided into suicidal ideation in adolescents, particularly from the perspective of the stress-diathesis model. According to various constructs from the ideation-to-action theory, it can be concluded that when adolescents' psychological reactivity and distress are recognized by families, educational centers, and professionals, intervention should occur, even if the individuals only report related feelings. Early life experiences, psychological pain, and cognitive and emotional reactions should not become motivations for suicide. At this stage, individuals may cry out for help, and if they do not find a way to save themselves, suicidal thoughts and actions may follow. Therefore, professionals are expected to intervene in response to these cries for help and prevent the progression from motivation to ideation, planning, and ultimately suicidal actions.