1. Background
The term “deliberate self-harm” (DSH) is used to refer both to intentional self-harm without suicidal intent [i.e., non-suicidal self-injury (NSSI), such as superficial cutting of the skin] and concurrently to all intentional self-harm behaviors, regardless of suicidal intent (1). Reports indicate an increase in self-harm in recent years (2). A meta-analysis suggests a lifetime prevalence of 28.2% worldwide (3). Although evidence indicates a decrease in the prevalence of self-harm during the transition from adolescence to adulthood, it can still reach 18.7% in young adults (4). Self-harm has been recorded as the third leading cause of disability-adjusted life years (DALYs) among 10- to 24-year-old individuals globally (5). More importantly, self-harm is a significant predictor of subsequent suicide attempts (6, 7). Additionally, these behaviors may be associated with substantial disability and psychosocial impairment (8).
Studies have consistently identified early adverse childhood experiences (ACEs), particularly childhood abuse, as one of the most significant risk factors for NSSI (9-11). Any form of child abuse significantly increases the risk of self-harm (12). A meta-analysis of the long-term health consequences of ACEs in adulthood (13) revealed that individuals with four or more ACEs were nine times more likely to engage in suicidal or self-harm behaviors compared to those without ACEs. Child abuse can be categorized into the following areas (14): Physical abuse, emotional abuse, sexual abuse, emotional neglect, and physical neglect. Although the link between exposure to abuse and self-harm is well-established, the mechanisms connecting childhood abuse experiences to self-harm remain unclear (15, 16).
Shame is one of the most significant emotions associated with various forms of childhood abuse (17). Individuals with multiple ACEs often present with a personality characterized by feelings of shame, helplessness, and a lack of agency (18). Shame can be understood as an affective-cognitive construct, comprising negative self-judgments (19) that are general, unfavorable, and characterized by a self-evaluation as inherently flawed, inadequate, or “bad” (20). Those who have experienced ACEs not only feel shame in specific situations but may also experience this feeling in response to intrusive thoughts, images, or memories related to these experiences (21). Among students who have experienced childhood abuse, feelings of shame can increase the likelihood of self-harm (22). In fact, recent research suggests that self-harm behaviors serve, in part, as a way to regulate shame experiences specifically, as well as a form of self-punishment in response to shame-based cognitions and affect (23). Only a systematic review has investigated the connection between shame and self-harm in adults, indicating that individuals with a history of self-harm report higher levels of shame (24).
However, the significance of feeling of disgust in reactions to traumatic events has been well-documented (25). Self-disgust is a conscious emotion that has been the subject of numerous studies in recent years. Self-disgust refers to a long-term or recurrent aversion to specific aspects of oneself, culminating in a series of negative reactions and rejection (26). Additionally, it has been shown that low distress tolerance, low self-compassion, high self-disgust, and consequently difficulty in emotion regulation, mediate the indirect effect of emotional neglect on NSSI (27). Individuals who engage in DSH, compared to both clinical and healthy individuals, experience higher rates of childhood abuse and have more negative self-concept content. Self-disgust demonstrated a significant mediating effect between childhood abuse and the presence of DSH (28). Although ACEs are recognized as risk factors for self-harm, the underlying mechanisms of this relationship remain unclear. Identifying risk factors for self-harm is crucial for understanding its mechanisms and for providing early prevention and treatment. The current study aims to investigate whether shame and self-disgust mediate the relationship between ACEs and the severity of self-harm. Our findings underscore the importance of screening for and treating the psychological effects of childhood abuse in adults engaged in self-harm behaviors, as well as the need for supportive interventions for those who have previously experienced ACEs. Focusing on the regulation and treatment of shame and self-disgust in individuals with a history of ACEs may play a crucial role in preventing self-harm. For mental health professionals, these findings emphasize the importance of addressing trauma-related shame and self-harm behaviors in clients who have encountered ACEs. Furthermore, if shame is a contributing factor to the development and persistence of self-harm, intervention and prevention strategies targeting shame-related emotions could prove particularly effective. Also, this study may contribute to the development of a model of ACEs and the etiology of DSH.
2. Objectives
The present study aimed to investigate the relationship between ACEs and self-harm through the mediating roles of shame and self-disgust.
3. Patients and Methods
3.1. Participants
The current descriptive-correlational, cross-sectional study employed a structural equation modeling (SEM) approach. All ethical principles, including voluntary sampling, informed consent, confidentiality of information, full explanation of research objectives and results to participants, and participants' freedom to withdraw from the research at any time during implementation, were observed in this study. The research was therefore performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
A sample size of 274 participants was determined using Free Statistics Calculators version 4.0, based on an effect size of 0.04, a power of 0.80, 3 predictor variables, and an alpha level of 0.05 (29, 30). To account for potential attrition, 300 questionnaires were completed. However, after assessment, 269 participants meeting the inclusion criteria were included in the final analysis. Inclusion criteria included providing informed consent, having basic literacy, not taking psychotropic medication during the study, reporting at least one self-harm behavior in the past six months (according to the questionnaire), aged 18 or older, and consent to the online research conditions. Exclusion criteria included incomplete questionnaires, a diagnosis of autism spectrum disorder, or a history of psychotic disorders (by asking individuals). In order to achieve research objectives, questionnaires were distributed among participants online to be completed, along with necessary explanations. The sample included all of the Iranian over 18 years old who had engaged in self-harm within the past six months who used social media (e.g., Instagram, Telegram, and WhatsApp) in 2024.
3.2. Measurements
3.2.1. The Deliberate Self-harm Inventory
This questionnaire is a 17-item self-report tool designed by Gratz to assess the lifetime history of self-harm behaviors. It includes the frequency, duration, and types of self-harm behaviors, such as cutting, burning, tattooing, breaking bones, etc. When participants indicated that they engaged in a particular form of self-harm, a series of additional open text questions was displayed asking for details of age at first occurrence, number of instances, and last occurrence of the particular behavior. These details were used to code whether a participant had engaged in any of the forms of self-harm in the past month. Participants respond with yes/no. Gratz reported a Cronbach's alpha coefficient of 0.82 and a test-retest reliability of 0.68 after two weeks (31). The higher scores indicating greater engaged in self-harm behavior. In Iran, Paivastegar, in a preliminary study on 40 female students, obtained a Cronbach's alpha of 0.71 (32).
3.2.2. The Childhood Trauma Questionnaire
The Childhood Trauma Questionnaire (CTQ), developed by Bernstein et al., (33) is a standardized, retrospective 28-item self-report inventory that measures the severity of different types of childhood trauma, producing five clinical subscales each comprised of five items: Emotional abuse, physical abuse, sexual abuse, emotional neglect, physical neglect. The measure also includes a three-item minimization/denial scale indicating the potential underreporting of maltreatment. If the total number of answers given to these questions was higher than 12, there was a high probability that the person’s answers are invalid. Participants respond to each item in the context of “when you were growing up” and answer according to a five-point Likert Scale ranging from “never” = 1 to “very often” = 5, producing scores of 5 to 25 for each trauma subscale. High scores in the questionnaire indicate more trauma or injury. The three items comprising the minimization/denial scale are dichotomized (“never” = 0, all other responses = 1) and summed; a total of one (1) or greater “suggests the possible underreporting of maltreatment (false negatives)”. In scoring, items 2, 5, 7, 13, 19, 26, and 28 are scored in reverse order. In Bernstein et al.’s research, the Cronbach's alpha coefficients for the questionnaire on a group of adolescents were 0.87 for emotional abuse, 0.86 for physical abuse, 0.95 for sexual abuse, 0.89 for emotional neglect, and 0.78 for physical neglect. Moreover, the concurrent validity of the questionnaire with therapists’ ratings of the level of childhood trauma was reported to be in the range of 0.59 - 0.78 (33). In Iran, Chegeni et al. reported the Cronbach alpha of this questionnaire from 0.81 to 0.98 for its five components (34).
3.2.3. The Experience of Shame Scale
The Experience of Shame Scale (ESS), developed by Andrews and Hunter (35), is a 25-item questionnaire that measures eight domains related to shame, including four domains of personality shame, three domains of behavioral shame (shame of doing something wrong, saying something stupid, and failing in a competitive situation), and physical shame. Participants respond based on their feelings over the past year, and each item is rated on a 4-point scale from 1 (not at all) to 4 (very much), resulting in a total score ranging from 25 to 100 with higher scores indicating greater shame. The total scale has demonstrated high internal consistency (Cronbach's alpha = 0.92) and a test-retest reliability of 0.83 over 11 weeks (35). In Iran, Tahmasibizadeh reported a Cronbach's alpha of 0.85 and a test-retest reliability of 0.76 over 3 months (36).
3.2.4. The Self-disgust Scale
This 18-item self-report questionnaire was developed by Overton et al. (37) to measure individuals’ thoughts and feelings about themselves. The questionnaire consists of three subscales, including appearance, general self-concept, and behavior/ability, and six neutral items to balance the negative aspects of the scale. The scale items are rated on a 7-point Likert Scale (1 = strongly agree, 7 = strongly disagree). Items 1, 3, 4, 7, 10, 12, 15, 17, and 18 are reverse-scored. The maximum score is 84, and the minimum score is 12, with higher scores indicating greater self-disgust. Cronbach's alpha for the 12 items measuring self-disgust was very high (0.91), indicating excellent internal consistency of the scale. The test-retest reliability of this questionnaire over a two-week interval has been reported as satisfactory (P < 0.001, r = 0.94) (37). In this study, the questionnaire was used for the first time in an Iranian population, and Cronbach's alpha for the total questionnaire was obtained to be 0.86.
3.3. Data Analysis
Statistical description indices of frequency and percentage were used for demographic information, and means, standard deviation, skewness, and kurtosis were employed for research variables. Prior to conceptual model analysis based on the collected data, statistical presumptions associated with SEM, such as adequate sampling size, normal distribution of scores of research variables (using skewness-kurtosis, normality distribution plots, and multivariate normality with Mahalanobis distance test), non-collinearity among predictors, independence of errors, and correlation of variables, and data reliability were examined. After establishing presumptions, SEM, comprising confirmatory factor analysis (CFA) and path analysis, was employed to test the research hypotheses and describe the proposed model. Data analysis was conducted using SPSS-25 and AMOS-24.
4. Results
The participants in this study consisted of 269 individuals (240 women and 69 men). Of them, 179 were single, 76 were married, and 14 were divorced. The majority of participants aged 19 - 26 years (42%). Participants with a high school diploma (40%) constituted the largest group in this study. The demographic characteristics of the participants are presented in Table 1.
| Variables | No. (%) |
|---|---|
| Gender | |
| Female | 240 (89.2) |
| Male | 29 (10.8) |
| Total | 269 (100.0) |
| Marital status | |
| Single | 179 (66.5) |
| Married | 76 (28.3) |
| Divorced | 14 (5.2) |
| Total | 269 (100.0) |
| Education level | |
| Under diploma | 50 (18.6) |
| Diploma | 109 (40.5) |
| Associate | 39 (14.5) |
| Bachelor | 50 (18.6) |
| Master | 14 (5.2) |
| PhD | 7 (2.6) |
| Total | 269 (100.0) |
The means, standard deviations, skewness, and kurtosis of the study variables are reported in Table 2. The results indicate that the skewness and kurtosis indices of the main study variables were within the range of -1 to +1, thus fulfilling the condition of univariate normal distribution. The maximum Mahalanobis distance was 30.76, which is smaller than the critical value of the chi-square tests equal to 31.264 with 11 degrees of freedom (number of subscales), indicating multivariate normality at the 0.001 level of significance.
| Variables and Components | Mean ± SD | SK | KU |
|---|---|---|---|
| 1. Self-harm | 3.96 ± 2.45 | 0.53 | -0.52 |
| 2. ACEs | 57.78 ± 18.67 | 0.30 | -0.51 |
| 3. Emotional abuse | 14.04 ± 5.94 | 0.23 | -0.95 |
| 4. Physical abuse | 8.22 ± 3.1 | 0.86 | 0.03 |
| 5. Sexual abuse | 8.48 ± 4.33 | 0.97 | 0.17 |
| 6. Emotional neglect | 15.51 ± 5.77 | -0.17 | -0.97 |
| 7. Physical neglect | 10.47 ± 4.4 | 0.67 | -0.27 |
| 8. Shame | 75.15 ± 16.27 | -0.55 | -0.35 |
| 9. Personality shame | 9.23 ± 9.4 | -0.44 | -0.74 |
| 10. Behavioral shame | 34.7 ± 6.09 | -0.77 | -0.25 |
| 11. Physical shame | 11.7 ± 3.51 | -0.58 | -0.75 |
| 12. Self-disgust | 51.18 ± 16.46 | -0.02 | -0.72 |
| 13. Disgust with appearance | 16.33 ± 6.26 | -0.02 | -0.72 |
| 14. Disgust with public perception of self | 17.87 ± 6.71 | -0.19 | -0.90 |
| 15. Disgust with the behavior | 17.04 ± 5.74 | -0.15 | -0.3 |
Abbreviations: SK, skewness; KU, kurtosis; ACEs, adverse childhood experiences.
In order to assess the presumption of non-multicollinearity among the predictor variables, the tolerance coefficient and variance inflation factor (VIF) indices were used. The tolerance values ranged from 0.63 to 0.87, and the VIF values ranged from 1.14 to 1.56, indicating non-multicollinearity among the predictor variables. The calculated value of the Durbin-Watson statistic was 2.2. Since this value falls within the range of 1.5 to 2.5, it suggests that the error values are independent.
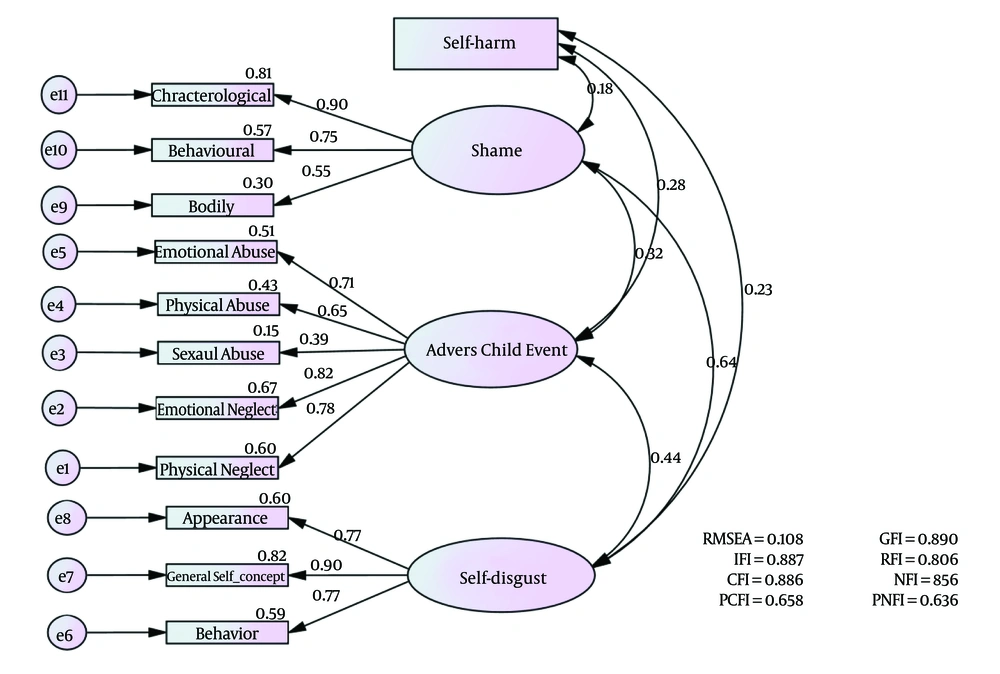
Based on Table 3, in the research conceptual model, the Goodness-of-Fit Index (GFI), root mean square error of approximation (RMSEA), Comparative Fit Index (CFI), Normed Fit Index (NFI), Incremental Fit Index (IFI), Relative Fit Index (RFI), Parsimonious Comparative Fit Index (PCFI), and Parsimonious Normed Fit Index (PNFI) were evaluated. The obtained values for the fit indices in both the first and second stages (modified model) were confirmed based on the mentioned standards. The research conceptual model is presented in Figure 1, and Tables 4 and 5.
| Indices | RMESA | GFI | IFI | RFI | CFI | NFI | PCFI | PNFI |
|---|---|---|---|---|---|---|---|---|
| Acceptable range | < 0.08 | > 0.90 | > 0.90 | > 0.90 | > 0.90 | > 0.90 | > 0.50 | > 0.50 |
| Desired model | 0.10 | 0.89 | 0.89 | 0.81 | 0.89 | 0.86 | 0.66 | 0.63 |
| Model fit | Non-fit | Non-fit | Non-fit | Non-fit | Non-fit | Non-fit | Fit | Fit |
| Modified model | 0.08 | 0.92 | 0.92 | 0.85 | 0.92 | 0.90 | 0.66 | 0.64 |
| Model fit | Fit | Fit | Fit | Non-fit | Fit | Fit | Fit | Fit |
Abbreviations: RMSEA, root mean square error of approximation; GFI, Goodness-of-Fit Index; IFI, Incremental Fit Index; RFI, Relative Fit Index; CFI, Comparative Fit Index; NFI, Normed Fit Index; PCFI, Parsimonious Comparative Fit Index; PNFI, Parsimonious Normed Fit Index.
| Variables | R (Multiple Correlation) | R2 (Determination Coefficient) | Adjusted R2 | F | P-Value |
|---|---|---|---|---|---|
| Values | 0.30 | 0.09 | 0.08 | 9.21 | 0.001 |
| Path | Standard Coefficient | Standard Error | C.R | P-Value |
|---|---|---|---|---|
| ACEs → self-harm | 0.16 | 0.05 | 2.12 | 0.033 |
| ACEs → shame | 0.35 | 0.04 | 4.03 | 0.001 |
| ACEs → self-disgust | 0.45 | 0.09 | 5.92 | 0.001 |
| Shame → self-harm | 0.07 | 0.10 | 0.95 | 0.342 |
| Self-disgust → self-harm | 0.10 | 0.04 | 1.17 | 0.240 |
Abbreviations: C.R, critical rate; ACEs, adverse childhood experiences.
According to Figure 1 and Table 4, ACEs, shame, and self-disgust accounted for approximately 10% of the variance in self-harm.
Based on the data presented in Table 5, the path coefficient from ACEs to self-harm was found to be 0.16. Given that the critical ratio (C.R) exceeded ± 1.96 and the P-value was less than 0.05 (C.R = 12.2, P = 0.033), this relationship was statistically significant. Similarly, the path coefficients from ACEs to shame (0.35) and self-disgust (0.45) were also significant, with C.R values exceeding ± 1.96 and P-values less than 0.01 (shame: C.R = 4.03, P = 0.001; self-disgust: C.R = 5.92, P = 0.001). Considering the C.R values below ± 1.96, and the P-values greater than 0.05 for both paths, the path coefficients from shame to self-harm (0.35) and from self-disgust to self-harm (0.35) were not statistically significant (shame to self-harm: C.R = 0.95, P = 0.243; self-disgust to self-harm: C.R = 1.17, P = 0.240).
As shown in Table 6, the indirect path from ACEs to self-harm, mediated by shame (0.03), was statistically significant, as the P-value was less than 0.05 and the 95% confidence interval did not include zero between the lower limit value (0.002) and the upper limit value (0.103) (P < 0.05). Similarly, the indirect path from ACEs to self-harm, mediated by self-disgust (0.06), was also statistically significant due to the p-value less than 0.05 and a 95% confidence interval that did not include zero between the lower limit value (0.011) and the upper limit value (0.130) (P < 0.05).
| Paths | Standard Coefficient | P-Value | 95% Confidence Interval | |
|---|---|---|---|---|
| Lower Bound | Upper Bound | |||
| ACEs → shame → self-harm | 0.03 | 0.034 | 0.002 | 0.103 |
| ACEs → self-disgust → self-harm | 0.06 | 0.018 | 0.011 | 0.130 |
Abbreviation: ACEs, adverse childhood experiences.
According to Table 7, the relationship between ACEs and self-harm (0.28) was found to be positive and statistically significant at the 0.01 level. Similarly, both shame (0.18) and self-disgust (0.20) were positively and significantly correlated with self-harm at the 0.01 level. Furthermore, ACEs were positively and significantly correlated with both shame (0.28) and self-disgust (0.40) at the 0.01 level.
| Variables | 1. Self-harm | 2. Shame (Total Score) | 3. Personal Shame | 4. Behavioral Shame | 5. Physical Shame | 6. Self-disgust (Total Score) | 7. Disgust with Appearance | 8. Disgust with Public Perception of Self | 9. Disgust with the Behavior | 10. ACEs (Total Score) | 11. Emotional Abuse | 12. Physical Abuse | 13. Sexual Abuse | 14. Emotional Neglect | 15. Physical Neglect |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 1 | ||||||||||||||
| 2 | 0.18 a | 1 | |||||||||||||
| 3 | 0.16 b | 0.93 a | 1 | ||||||||||||
| 4 | 0.10 | 0.85 a | 0.69 a | 1 | |||||||||||
| 5 | 0.23 a | 0.63 a | 0.48a | 0.38 a | 1 | ||||||||||
| 6 | 0.20 a | 0.57 a | 0.53 a | 0.41 a | 0.51 a | 1 | |||||||||
| 7 | 0.18 a | 0.52 a | 0.44 a | 0.38 a | 0.57 a | 0.86 a | 1 | ||||||||
| 8 | 0.19 a | 0.50 a | 0.49 a | 0.36 a | 0.41 a | 0.91 a | 0.70 a | 1 | |||||||
| 9 | 0.14 b | 0.74 a | 0.46 a | 0.33 a | 0.36 a | 0.85 a | 0.56 a | 0.70 a | 1 | ||||||
| 10 | 0.28 a | 0.28 a | 0.24 a | 0.20 a | 0.30 a | 0.40 a | 0.29 a | 0.33 a | 0.26 a | 1 | |||||
| 11 | 0.25 a | 0.30 a | 0.27 a | 0.19 a | 0.33 a | 0.37 a | 0.29 a | 0.35 a | 0.32 a | 0.77 a | 1 | ||||
| 12 | 0.13 b | 0.22 b | 0.18 a | 0.17 a | 0.22 a | 0.19 a | 0.17 a | 0.20a | 0.13 b | 0.66 a | 0.51 a | 1 | |||
| 13 | 0.26 a | 0.12 b | 0.12 b | 0.07 | 0.09 | 0.01 | 0.02 | 0.02 | 0.03 | 0.49 a | 0.24 a | 0.38 a | 1 | ||
| 14 | 0.19 a | 0.23 a | 0.21 a | 0.16 b | 0.26 a | 0.35 a | 0.29 a | 0.37 a | 0.27 a | 0.79 a | 0.54 a | 0.42 a | 0.23 a | 1 | |
| 15 | 0.07 | 0.16 b | 0.13 b | 0.11 | 0.18 a | 0.23 a | 0.20 a | 0.24 a | 0.15 b | 0.74 a | 0.48 a | 0.39 a | 0.24 a | 0.72 a | 1 |
a P < 0.01.
b P < 0.05.
5. Discussion
This study aimed to investigate the relationship between ACEs and DSH through the mediating roles of shame and self-disgust. Prior to examining the mediating roles of shame and self-disgust, we investigated the direct relationship between ACEs and self-harm. As shown by our findings, ACEs can be directly linked to self-harm. This finding aligns with previous research. For instance, Hu et al.’s study revealed that the greater the number, duration, and types of maltreatment a child experiences, the higher the future risk of hospitalization due to these DSH behaviors (38). Research has demonstrated that growing up in environments characterized by poverty, violence, substance abuse, and multiple ACEs is strongly associated with an increased risk of dual harm (self-harm and harm to others) (39). A study conducted on forensic psychiatric patients reported a widespread prevalence of childhood maltreatment among this group; only 5% (5.7%) of participants reported no emotional abuse in childhood. According to the files, 57.2% of participants reported physical abuse and 20% reported sexual abuse during childhood. Each additional ACE significantly predicted an increased likelihood of NSSI (40). In a recent meta-analysis conducted by Liu et al., evidence clearly indicates that multiple forms of childhood maltreatment independently and collectively predict NSSI. However, emotional abuse has potentially larger negative effects compared to other types of abuse (9). In support of these findings, childhood traumas impair children’s ability to develop positive adaptations and, in turn, lead them to adopt defective alternative regulatory and relational strategies such as self-harm (41). Childhood trauma and various forms of early neglect can produce neurobiological effects that may impair the brain’s ability to control and regulate emotions, making traumatized individuals more prone to impulsivity (42). A very recent study found that resting-state functional connectivity between the amygdala and the dorsolateral and orbitofrontal cortices is altered in bipolar disorder adolescents with a history of self-harm (43).
Structural equation modeling results indicated that ACEs had a direct effect on self-harm and an indirect effect on self-harm mediated by shame. This finding is consistent with previous research. Studies have indicated that the childhood environment is significantly associated with feelings of shame. High levels of abuse, in all its forms, accompany more intense feelings of shame (44). Experiences of poor care during childhood are associated with emotional difficulties, such as shame and self-disgust. In other words, negative family environments that provide little support and positive feedback may enhance the risk of experiencing shame (45). The results of a meta-analysis in 2019 revealed that feelings of shame following childhood sexual abuse (CSA) significantly impacted psychological effects and trauma symptoms. Overall, studies provide evidence that shame can hinder psychological adjustment after CSA (46). To explain this finding, it can be argued that children who do not receive affection from their parents may develop the belief that they do not deserve such feelings. This can lead to feelings of inadequacy and defectiveness. Ultimately, these negative emotions can manifest as feeling of shame (47). In fact, recent research suggests that NSSI behaviors serve, in part, as a way to regulate the experience of shame specifically, as well as a form of self-punishment in response to shame-based cognitions and affect (23). Evidence suggests that childhood trauma and various forms of early neglect can induce neurobiological effects that may disrupt the brain’s ability to regulate emotions, which may make these individuals more prone to impulsivity (42). Since these individuals are deprived of opportunities to learn emotion regulation strategies due to early traumatic experiences, they tend to engage in behaviors such as NSSI as a temporary diversion from negative emotions (48). According to the traumagenic dynamic model of child sexual abuse, negative messages sent to the child regarding the abuse by the perpetrator, the child’s environment, and society often become part of the child’s self-concept, leading to negative self-perceptions and blame and shame. For example, a victim who internalizes such messages may think that they are bad or deserve what happened to them. Blame and shame can increase the risk of adverse life outcomes and suicidal thoughts (49).
The SEM results also indicated that ACEs have a direct effect on self-disgust and an indirect effect on self-harm, mediated by self-disgust. This finding aligns with previous research. Individuals who have experienced repeated physical or emotional abuse may come to believe they possess hateful qualities and develop self-disgust (50). In a study in 2010, Rachman demonstrated that post-traumatic cognitive appraisal regarding one’s role in a traumatic event can culminate in the emergence of self-disgust. For instance, an individual may describe experiencing sexual arousal during rape as unpleasant and morally reprehensible and feel repulsed by it. These interpretations can give rise to persistent and maladaptive self-disgust as a result of generalized distorted beliefs (51). According to Nilsson et al., individuals who engage in self-harm have experienced more childhood maltreatment and possess more negative self-concept content. In this research, emotional abuse was most strongly associated with DSH. Self-disgust showed a significant mediating effect between emotional abuse and the presence of DSH (28). To explain this finding, it can be argued that childhood abuse can distort a child’s perception of themselves. The child may even believe that they are to blame for being abused, making it difficult to let go of internal guilt and leading to feelings of self-disgust (52). Similarly, individuals who are abused during childhood may develop negative and pessimistic cognitive views of themselves, the world, and the future. They may believe they were abused because they are bad, guilty, and worthless, leading to self-disgust (53). In addition to the explanations, individuals with self-disgust report physical sensations such as nausea or illness, avoidance or self-injurious behaviors, and specific beliefs, such as the belief that they have unchangeable repulsive traits or the belief that they can infect others. In situations where they cannot easily forget repulsive aspects such as perceived traits about themselves or traumatic memories, self-disgust may lead them to punish themselves or even attempt to eliminate themselves (54).
Our findings emphasize the importance of screening for and treating the psychological effects of childhood maltreatment in adults who engage in self-harm, as well as the need for supportive interventions for those who have previously experienced childhood adversity.
5.1. Conclusions
The findings of the present study have important implications for child protection, prevention of DSH and suicide, as well as caregiving practices in emotion regulation, particularly shame and self-loathing. Early identification and intervention are crucial for the early prevention of ACEs. Early intervention as possible for children exposed to childhood trauma may lead to reduced future self-harm. Despite its complexities, this remains an area in which further research is warranted. Furthermore, further research is needed to further confirm the impact of childhood trauma not only on DSH across the lifespan, but also on other mental health outcomes, suicide attempts, and suicide deaths. These findings also highlight the importance of trauma care for individuals seeking treatment for DSH. Trauma-related shame and self-disgust following ACEs could increase DSH. As emotions of shame and disgust may not be openly expressed, interventions addressing DSH by alleviating the negative impacts of these emotions are likely to foster the development of more adaptive coping strategies.
5.2. Limitations
Data collection was conducted online and was accessible. This study relied solely on self-report questionnaires, which may have led to participants withholding accurate responses, and issues such as bias and social approval may have influenced responses. Information regarding childhood trauma was collected retrospectively, and the passage of time may have distorted participants’ memories of these events. The study was conducted cross-sectional, preventing causal inferences. Given that the majority of participants (89%) were female, caution should be exercised when generalizing the findings to the male population. It is suggested that more precise sampling methods be used in the future and that samples be collected in person, if possible. The severity and duration of involvement with self-harm should be considered and examined in data analysis. Further longitudinal research is needed to disentangle the mechanisms that cause DSH. Given the cultural diversity of Iranian society, it is suggested that this research be repeated in different ethnic-cultural samples to increase the generalizability of the results.