1. Background
Opioids are narcotic substances extracted from the poppy plant, and their misuse due to sedative effects dates back to 4000 B.C. (1). Currently, their prevalence is rising in certain parts of the world, including Iran (2), with a reported prevalence of 13.6% among adults in Babol (3). Recent studies indicate significant societal and health impacts due to increased opioid use, contributing to various health burdens across demographics. Opioids can affect different systems of the body, including the central nervous, respiratory, and cardiovascular systems (4). Coronary artery disease (CAD) is the most common cause of mortality worldwide (5), with many individuals having at least one cardiovascular risk factor such as hypertension, smoking, dyslipidemia, obesity, and diabetes mellitus (DM). Research consistently highlights that adverse cardiovascular events can occur even in individuals with a normal lipid profile, emphasizing the need for comprehensive evaluations beyond traditional risk factors (6, 7). Therefore, new indices such as atherogenic indices have been proposed. These indices, calculated using simple mathematical formulas, can indicate the severity of atherosclerosis and are useful in predicting the likelihood of CAD (8-12). The Atherogenic Index, also known as Castelli’s Risk Index I and II (CRI I and CRI II), is derived from dividing total cholesterol (TC) or low-density lipoprotein (LDL) by high-density lipoprotein (HDL) (Table 1). This index has a direct relationship with cardiovascular events and is correlated with the thickness of the intima and media of the carotid artery, a sign of subclinical atherosclerosis (8, 9). Another index introduced for predicting the likelihood of atherosclerosis in coronary arteries is the Atherogenic Index of plasma (AIP) (10). High-density lipoprotein is recognized as a protective lipoprotein against CAD, while LDL is considered an atherogenic factor. Emerging evidence suggests that non-HDL may provide a more accurate measure for predicting atherosclerosis, as it encompasses all lipoproteins containing Apo B, which are implicated in atherogenesis (11). The Triglyceride-Glucose Index (TyG) is also an Alternative Index that indicates insulin resistance. This index is closely associated with the onset of non-communicable diseases such as hypertension, diabetes, CAD, stroke, obesity-related cancers, and even cardiovascular outcomes in diabetic patients (12). Statistics indicate that 36% of CAD patients in Iran consume opium (6). Various articles report different effects on the cardiovascular system and lipid profiles depending on the duration and amount of opium consumption. For instance, some studies indicate that prolonged opium use is associated with an increased risk for acute myocardial infarction and cardiovascular-related mortality (13). Conversely, other studies, such as that by Marmor et al., reported that opium consumption might confer a protective effect against cardiovascular diseases (14). There is also variability in the results regarding opium's effects on lipid profiles, with studies reporting significant lipid reductions, increases, or no impact compared to non-consumers (15-17).
| Lipid Indices | Formula | Normal Values a |
|---|---|---|
| CRI-I | TC/HDL | ≥ 4 |
| CRI-II | LDL/HDL | ≥ 3 |
| Non-HDL cholesterol (NHC) | TC - HDL | ≥ 130 |
| Atherogenic coefficient (AC) | Non-HDL/HDL | ≥ 2 |
| AIP | Log (TG/HDL) | ≥ 0.1 |
| TyG Index | Ln [TG × FBS/2] | ≥ 9.04 |
Definitions and Formulas for Lipid Indices
2. Objectives
Therefore, considering the rising trend of addiction in society and the increasing prevalence of CVD and their risk factors, particularly dyslipidemia, along with the conflicting reports regarding the effects of opium on lipid profiles and risk factors for cardiovascular diseases, this study aims to clarify the relationship between opium use and cardiovascular risk factors. It hypothesizes that opium consumers may exhibit distinct lipid profile changes and cardiovascular risk factor patterns compared to non-consumers.
3. Patients and Methods
3.1. Setting
The statistical population for this study comprised all eligible patients undergoing coronary angiography at Razi Hospital in Birjand, Iran, from March 2018 to March 2021. All patients who underwent coronary angiography during this time frame were included in the study, ensuring a comprehensive sample for analysis. Recruitment occurred during this period, with data collection following the angiography procedures. The study was conducted in compliance with ethical standards, and approval was obtained from the Ethics Committee of Birjand University of Medical Sciences (approval code: IR.BUMS.REC.1401.171).
3.2. Study Design
This cross-sectional study targeted patients diagnosed with significant coronary artery stenosis (greater than 50%) who underwent angiography. Patients were categorized into two groups: Opium consumers and non-consumers, based on self-reported opium usage at the time of angiography.
3.2.1. Inclusion Criteria
Eligible participants included adults aged 18 years or older with at least one coronary artery exhibiting stenosis greater than 50%, as confirmed through angiographic evaluation.
3.2.2. Exclusion Criteria
Individuals with significant comorbid conditions, such as advanced-stage heart failure or terminal illnesses, and those with cognitive impairments that could affect the reliability of self-reported consumption status were excluded from the study.
3.3. Variables
Outcomes of interest included lipid profiles, demographic information (age, gender), medical history, and Body Mass Index (BMI). The exposures were defined as opium consumption status (users vs. non-users). Potential confounders, such as age, gender, and comorbidities, were recorded to control for their effects in the analysis. Lipid profiles were measured through standard laboratory blood tests, assessing levels of TC, triglycerides (TG), LDL, and HDL. Demographic information was obtained through patient interviews and medical records, ensuring accurate reporting of age and gender. Medical history was collected via structured questionnaires detailing any previous diagnoses of cardiovascular diseases, hypertension, diabetes, and dyslipidemia. The BMI was calculated using the formula: Weight (kg)/height (m2), based on measured weight and height.
Please ensure that all references are correctly formatted according to the AMA style, as indicated by the numbers in parentheses if applicable.
3.4. Data Sources and Measurement
Data were systematically gathered from patient records using a structured checklist that included demographic details, medical history, BMI, and lipid profiles, including TC, TG, LDL, and HDL. Additionally, relevant angiographic data were extracted from the national online registry system for cardiovascular diseases (18). New lipid indices were calculated using established formulas outlined in Table 1 (8-12).
3.5. Handling Quantitative Variables
Quantitative variables were reported as mean ± standard deviation. Analyses included comparative statistics using appropriate methods, utilizing SPSS statistical software, version 22. For normally distributed data, parametric tests were applied; for non-normally distributed data, non-parametric tests were utilized.
3.6. Statistical Analysis
Statistical analyses were conducted to compare qualitative variables using the chi-square test (or Fisher's exact test). The Kolmogorov-Smirnov test was employed to assess the normality of quantitative variables. Departures from normality prompted the use of the Mann-Whitney U test. A significance level of P ≤ 0.05 was considered statistically significant. The specific statistical methods employed reflect an effort to control for confounding variables and enhance the robustness of the findings.
4. Results
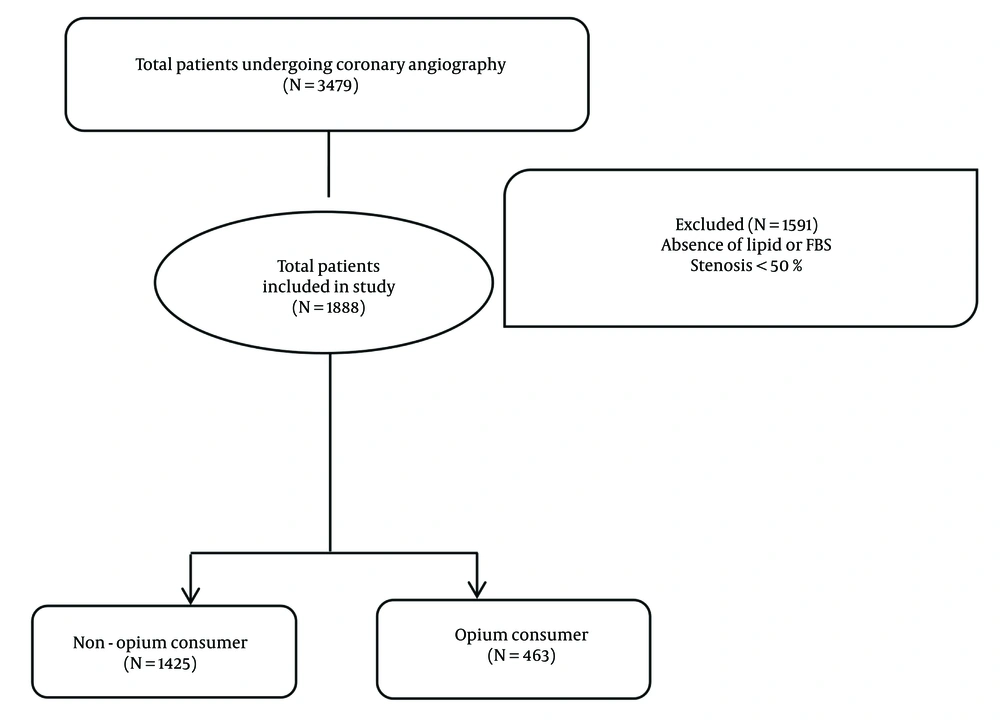
Out of 3,479 individuals who underwent coronary angiography at Razi Hospital during the years 2018 - 2020, 1,888 patients had stenosis greater than 50% in at least one coronary artery. Additionally, 1,591 individuals with stenosis less than 50% in coronary arteries or lacking lipid profile or fasting blood sugar data were excluded from the study. Therefore, our study sample consisted of 1,888 individuals (Figure 1).
Out of the 1,888 patients included in the study, the majority were male (68.5%). Of these, 463 (24.5%) were opium consumers, and 1,425 (75.5%) were non-consumers. A comparison of demographic characteristics and medical history is presented in Table 2. The mean age of participants in the study was 63.46 ± 11.43 years. Opium consumers were approximately 4 years younger (60.14 ± 11.64 years) than non-consumers (64.38 ± 11.74 years, P < 0.001). Additionally, non-opium consumers exhibited a significantly higher prevalence of hypertension (55.0%), DM (31.0%), and dyslipidemia (28.8%). In contrast, a history of previous percutaneous coronary intervention (PCI) and smoking was significantly higher among opium consumers. Laboratory factors in both groups are examined in Table 3. As shown, TG were significantly lower in opium consumers. The levels of fasting blood sugar, cholesterol, HDL, and LDL showed no significant differences between the two groups. Among the new indices, the AIP, TyG Index, and non-HDL were significantly lower in the opium-consuming group compared to the non-consumers. Other lipid indices did not show statistically significant differences between the groups.
| Variables | Total (N = 1888) | Non-opium (N = 1425) | Opium (N = 463) | P-Value |
|---|---|---|---|---|
| Age (y) | 63.46 ± 11.43 | 64.38 ± 11.74 | 60.14 ± 11.64 | 0.001 c |
| BMI | 25.12 ± 4.73 | 25.46 ± 4.77 | 24.67 ± 4.04 | 0.001 c |
| Gender | 0.001 c | |||
| Male | 1293 (68.5) | 928 (65.1) | 365 (78.8) | |
| Female | 595 (31.5) | 497 (34.9) | 98 (21.2) | |
| Risk factors | ||||
| Hypertension | 977 (52.0) | 780 (55.0) | 197 (42.8) | 0.001 c |
| DM | 532 (28.3) | 441 (31.0) | 91 (19.6) | 0.001 c |
| Dyslipidemia | 515 (27.5) | 410 (28.8) | 105 (22.9) | 0.009 c |
| Family history of CAD | 352 (18.8) | 267 (18.9) | 85 (18.4) | 0.822 |
| History of CABG | 92 (4.8) | 69 (4.8) | 23 (4.9) | 0.974 |
| History of PCI | 271 (14.3) | 191 (13.4) | 80 (17.3) | 0.049 c |
| Smoking status | 0.001 c | |||
| No smoker | 1605 (85.3) | 1303 (91.7) | 302 (65.5) | |
| Current smoker | 204 (10.8) | 83 (5.8) | 121 (26.2) | |
| Recent smoker | 73 (3.9) | 35 (2.5) | 38 (8.2) |
| Variables | Total | Non-opium | Opium | P-Value |
|---|---|---|---|---|
| TG | 127.57 ± 83.56 | 131.53 ± 86.75 | 115.71 ± 59.37 | 0.001c |
| Cholesterol | 165.36 ± 36.81 | 166.14 ± 14.81 | 162.95 ± 100.83 | 0.09 |
| LDL | 100.15 ± 28.42 | 101.14 ± 41.73 | 97.33 ± 10.97 | 0.06 |
| HDL | 43.20 ± 12.31 | 43.38 ± 12.80 | 42.63 ± 10.67 | 0.51 |
| Fasting blood sugar | 129.35 ± 62.19 | 130.65 ± 94.73 | 125.56 ± 36.34 | 0.12 |
| CRI-I | 3.99 ± 1.46 | 4.00 ± 1.28 | 2.97 ± 1.87 | 0.26 |
| CRI-II | 2.45 ± 1.44 | 2.45 ± 1.41 | 2.97 ± 2.39 | 0.35 |
| AIP | 0.41 ± 0.28 | 0.43 ± 0.28 | 0.38 ± 0.20 | 0.02c |
| TyG Index | 8.78 ± 0.72 | 8.81 ± 0.73 | 8.66 ± 0.66 | 0.001c |
| Non-HDL cholesterol | 122.16 ± 62.95 | 122.76 ± 44.97 | 120.73 ± 31.99 | 0.02c |
5. Discussion
The overall prevalence of opium consumption among our CAD patients was 24.5%. In the study by Aghadavoudi et al. in Isfahan, which involved 325 patients undergoing coronary bypass surgery, the rate of opium consumption was reported to be 36%, and in the study by Davoodi et al., which explored 160 patients with acute myocardial infarction in Tehran, it was 28.1% (6, 19). In the context of our study objectives, it is evident that opium consumption among CAD patients is prevalent and varies across different regions. This underlines the necessity of addressing substance use in the management of cardiovascular risks.
In the current study, the history of DM in opium consumers was lower than in non-consumers. The findings align with studies by Sheikhy et al. (20), Hamrah et al. (1), and Liew et al. (21), which also reported lower DM rates among opium users. Nalini et al. conducted a study on 40,083 participants in the Golestan Cohort Study, which took place from 2004 to 2008 in the Gorgan and Golestan region and involved a 12-year follow-up. The aim was to investigate the long-term relationship between DM and opium; thus, researchers excluded individuals with DM at the beginning of the study and then compared the incidence of DM among opium users and non-users. Results showed that individuals who used opium for a long time (average use duration of about 10 years) had a lower BMI (23.5% vs. 27%) and a lower waist circumference (88.9 cm vs. 95.7 cm), which were statistically significant. Furthermore, the incidence of DM in these individuals was 17% lower than in non-consumers, primarily due to reduced body mass and smaller waist circumference. Researchers attributed the lower blood sugar levels in opium users to lower body mass and less abdominal obesity (22).
In our study, the history of hypertension was less frequent in the opium-consuming group. The blood pressure levels in the opium group were also lower, which was consistent with our study, but in the study by Hamrah et al. (1), elevated blood pressure was reported among opium addicts. This discrepancy may indicate the impact of dosage and duration of opium use on blood pressure regulation; thus, it reflects the complexity of interpreting cardiovascular outcomes among opium users. Low doses and short-term administration of opium typically lower blood pressure through vasodilation and reduced sympathetic tone, while long-term opium use can lead to increased plasma homocysteine, higher oxidative stress, decreased opioid receptor availability, and ultimately increased blood pressure (1).
In this study, triglyceride levels were significantly lower in opium consumers. Additionally, the studies by Asgary et al. (23) and Fatemi et al. (15) reported higher triglyceride levels in the non-opium group compared to the opium-consuming group. This finding underlines the relationship between opium consumption and lipid profiles, suggesting that lower BMI in opium users may contribute to their favorable triglyceride levels. However, it is important to consider potential confounding factors or selection biases that might influence these results. Factors such as dietary habits, levels of physical activity, and other lifestyle choices may have skewed our findings. Further investigation is necessary to determine the extent to which these factors impact lipid profiles in both opium consumers and non-consumers.
Regarding the suggestion that opium could be considered a significant management strategy for reducing cardiac risk factors, we must clarify that while our findings indicate a correlation between opium use and lower triglyceride levels, this does not imply causation or advocate for opium as a treatment modality. The complexities surrounding the consumption of opium, along with its associated health risks, necessitate a cautious interpretation of these results. To strengthen our manuscript, we acknowledge the need for a critical discussion addressing potential mechanisms, limitations, and alternative explanations for our findings. This would provide a more comprehensive understanding of the dynamics at play and ensure that the interpretation of our results is accurate and not misleading.
In our study, there were no significant differences in cholesterol and LDL levels between non-consumers and consumers of opium; however, in the studies by Hamrah et al. (1), Fatemi et al. (15), and Kazemi et al. (8), cholesterol levels were lower in the opium-consuming group compared to non-consumers. In the studies conducted by Aghadavoudi et al. (6), Fatemi et al. (15), and Liew et al. (21), LDL levels were higher in non-consumers compared to users. Dietary habits, socioeconomic status, and unhealthy lifestyle choices may influence lipid profiles and LDL levels in individuals. In the present study, HDL levels did not show significant statistical differences between non-opium users and opium users, which was similar to Liew's study (21).
In our study, the AIP, TyG, and non-HDL were significantly lower in the opium-consuming group compared to the non-consumers. We did not find any similar studies comparing these indices in opium users. This suggests a novel area for further research to comprehensively understand the implications of these indices in assessing cardiovascular risks associated with opium use. Given that in this study, the rate of smoking had a significant positive correlation with opium use (26.2% smokers in the opium group vs. 5.8% smokers in the non-opium group), we explored related studies concerning these new lipid indices among smokers. Baek et al. conducted a study in Korea comparing the TyG Index among the subjects. They found that in smokers or alcohol users, this index was higher compared to non-smokers or non-alcohol users, and those who consumed both (smoking and alcohol) showed significantly higher levels (24). Tobacco and cigarette smoke can produce pro-inflammatory toxic substances. Additionally, oxidative stress and mitochondrial dysfunction in smokers can reduce peripheral insulin and increase sensitivity to it. Direct dysfunction of β-cells has also been reported in smokers (24).
The molecular mechanism of opium in the pathogenesis of CAD remains unclear. Momeni-Moghaddam et al., in a case-control study, compared the expression of receptors CD36, CD68, CD9 as well as levels of inflammatory factors tumor necrosis factor alpha (TNF-α), interferon gamma (IFN-γ), and malondialdehyde (MDA) in three groups (30 addicted CAD patients, 30 non-addicted CAD, and 17 healthy opium users). The results showed that only inflammatory factors were elevated in addicted CAD patients. This finding suggests the need for further investigation into the inflammatory pathways linked to opium use and CAD, which might isolate opium as an independent risk factor despite lower levels of traditional cardiovascular risk factors (25).
5.1. Limitations
This study has several limitations. Firstly, the reliance on self-reported data regarding opium consumption may introduce recall bias. Secondly, the cross-sectional design limits the ability to establish causal relationships. Lastly, the study was conducted in a single center, which may affect the generalizability of the findings to other populations. Additionally, we were unable to assess confounders such as diet, alcohol consumption, and exercise, which may influence the results.
5.2. Conclusions
In conclusion, while the current study suggests that opium consumption may present a distinct profile regarding cardiovascular risk factors, caution should be exercised in the universal interpretation of these results. Further research, particularly mechanistic studies, is essential to confirm these findings and clarify opium's role as an independent risk factor for cardiovascular diseases across diverse populations and settings. Such investigations could significantly enhance our understanding of the complexities surrounding opium use and cardiovascular health. To improve the understanding and management of the intricate relationship between opium use and cardiovascular health, we advocate for interdisciplinary collaboration. Engaging with addiction specialists will provide a better context for our findings within the framework of addiction behaviors. Moreover, collaborating with public health experts can facilitate the development of comprehensive intervention strategies that address the multifaceted challenges associated with opium consumption and its health implications.