1. Background
Suicide is a significant public health issue and one of the leading causes of death worldwide (1). It is the second leading cause of death globally for young people aged 10 to 24, the third leading cause of death among male adolescents aged 10 to 24, and the most common cause of death among girls aged 15 to 19 (2). The prevalence of suicide planning, attempts, and ideation among adolescents aged 13 to 17 in 59 middle- and low-income nations was 17%, 17%, and 16.9%, respectively (3). Additionally, 88% of adolescent deaths due to suicide occurred in middle- and low-income nations (4). Given the widespread harmful effects of suicide on individuals, families, and communities, advancing suicide prevention is crucial.
Current research on suicide prevention primarily focuses on risk factors that increase vulnerability to suicide, such as psychiatric disorders, suicidal thoughts, and previous suicide attempts (5, 6). These investigations have enhanced our understanding of suicide and enabled timely identification of vulnerable individuals. However, some scholars have noted the limited predictive validity of these risk factors and reported that focusing solely on them is insufficient for effective suicide prevention strategies (7). Tools like the Beck Scale for Suicidal Ideation are commonly used to assess individuals at risk. This scale has been validated in Iranian samples and is recognized for use in various research contexts (8). However, most tools focus on current suicidal thoughts and cannot assess the potential for suicide in individuals without such thoughts. Existing tools emphasize risk factors, with less focus on identifying protective factors.
Life satisfaction and problem-solving questionnaires are used to measure protective factors against self-destructive behaviors, but they lack content validity due to the absence of suicide-related questions (9). Recently, studies have focused on protective factors like suicide resilience, which play a crucial role in prevention (10). Suicide resilience emerged from the increasing focus on psychological resilience, defined as a personal trait that helps individuals cope well despite adversity. It involves maintaining mental health despite significant stress or adapting to unfavorable situations (11, 12). In the context of suicide, resilience significantly impacts the concept of suicide resilience. Osman et al. defined suicide resilience as a perceived resource, competency, and capability to regulate suicidal feelings, attitudes, and thoughts (9). He identified three categories of protective factors: External protection, emotional stability, and internal protection (9).
Research indicates that individuals more resilient to suicide when facing adversity are more likely to experience positive outcomes, such as preventing suicidal thoughts. Conversely, individuals may become trapped in a cycle of suicide (13). Fortunately, further research suggests that suicide resilience is not a fixed state but a dynamic process (13). Measuring suicide resilience is essential in vulnerable groups, such as adolescents, the elderly, psychiatric patients, and substance users, especially those who have attempted suicide. Protective factors against suicidal behaviors may vary based on the phase of suicide (ideation or action) and cultural context (14). Effective empirical resources are crucial for preventing suicide risk by enhancing resilience. These tools can identify individuals at risk and facilitate the design of early intervention programs.
However, only six scales for measuring suicide resilience exist in the literature, none of which are widely used (9, 15-19). One of these is the Suicide Resiliency Scale by Osman et al. (9), which includes 25 questions and three subscales: External protector, emotional stability, and internal protector. This scale is more comprehensive than others, emphasizing four of the five concepts associated with suicide resilience: Coping strategies, social support, meaning of life, sense of responsibility, and psychological capital. Its validity and reliability have been confirmed in African-American and Chinese-American samples (20, 21), as well as in adolescents admitted to psychiatric wards (22). Despite the importance of measuring suicide resilience, only one study has explored the psychometric properties of this tool in adult samples, limited to exploratory analysis (23).
Given the high prevalence of ideation and suicide attempts among adolescents, few studies have focused on suicide resilience in this population, particularly among those with a history of suicide attempts. Research on protective factors, emphasizing differences between adolescents with and without suicide attempts in both nonclinical and clinical populations, is limited. Therefore, the present investigation aims to study the psychometric characteristics of the Suicide Resilience Scale in a sample of Iranian adolescents.
2. Objectives
The present study aimed to validate the Suicide Resilience Questionnaire among Iranian adolescents, both with and without suicidal ideation.
3. Materials and Methods
3.1. Participants and Procedures
This study was conducted in three stages. In the first stage, to identify students with suicidal ideation, a sample of 12,000 students aged 13 to 18 years in Lorestan province was selected through random cluster sampling. Each county in Lorestan province was considered a cluster, and five counties — Nurabad, Kuhdasht, Aleshtar, Borujerd, and District 1 of Khorramabad Education — were randomly selected as clusters for inclusion. The Suicide Probability Scale (SPS; Call and Gill, 1982) was administered to these students. To determine inclusion for the interview phase, a cut-off point was applied: Students scoring at or above the 90th percentile of the SPS total score distribution within the sample (i.e., the top 10% of scorers) were considered at elevated suicide risk and selected for further assessment. This percentile-based threshold is consistent with prior Iranian validation studies and ensures the selection of students most likely to be at risk. Among the 12,000 students, those who answered all questions of the SPS and obtained high scores (at or above this 90th percentile cut-off) were identified. A total of 923 students were then selected using purposive sampling and interviewed by school counselors, ensuring no item was left unanswered. In the first study [exploratory factor analysis (EFA)], research was conducted on 300 students; in the second study [confirmatory factor analysis (CFA)], 618 students participated. Ethics approval (IR.ALZAHRA.REC.1401.121) was obtained at the outset, and informed consent was obtained from both parents and students prior to participation.
Despite the rigorous random cluster sampling and standardized procedures applied, potential sources of bias exist. Non-response bias may arise if students with more severe psychological distress or suicidal ideation declined to participate or did not complete the questionnaire, potentially resulting in underrepresentation of high-risk individuals. Additionally, the purposive selection method, limited to those with complete responses and high SPS scores, may introduce selection bias, as students who may be at risk but did not fully complete the questionnaire were excluded.
3.1.1. Suicidal Ideation
The SPS subscale was used to evaluate suicidal ideation (SI). This subscale measures self-reported traits associated with suicide risk and has been reported to prospectively anticipate suicide attempts (24). The internal consistency for this study was very good (α = 0.86).
3.1.2. Anxiety and Depression
The Hospital Anxiety and Depression Scale (HADS) was employed to measure anxiety and depression. This scale includes 14 items, with seven items related to depression (e.g., "I have lost interest in my appearance") and seven items related to anxiety (e.g., "Worrying thoughts go through my mind"). Items are rated on a 0 - 3 scale, with agreement strength increasing by number. The HADS is a reliable, valid, and well-established measure of affect (25), evaluating depression and anxiety in primary care, general populations, and the psychiatric field. For the studied sample, Cronbach’s alpha was 0.80 (26).
3.1.3. Hopelessness
Hopelessness was measured using the Beck Hopelessness Scale (27), a reliable and valid tool shown to predict eventual suicide (28). The internal consistency in this study was very good (Kuder-Richardson Formula 20 = 0.92).
3.1.4. Suicide Resilience Inventory-25
As the main measure in the present study, the Suicide Resilience Inventory-25 (SRI-25) evaluated three dimensions of the suicide resilience construct: External protective, emotional stability, and internal protective. This scale is designed for a 7th- to 8th-grade reading level, with responses ranging from 1 (strongly disagree) to 6 (strongly agree) to indicate resilience levels. The mean item score reflects the overall score. According to Osman et al. (9), this inventory has moderate to high internal consistency reliability estimates and an established factor structure. Gutierrez et al. (22) reported good reliability and validity estimates for Afro-American college students, and it showed concurrent validity and good internal consistency (α = 0.96; AIC = 0.49) in adolescent inpatient subjects (21).
3.2. Data Analysis
Data analyses were performed using SPSS version 26 and Mplus version 8.3. Exploratory factor analysis was performed using principal axis factoring with varimax rotation to assess the underlying structure of the SRI-25. Factor retention was based on eigenvalues > 1, and factor loadings ≥ 0.40 were deemed acceptable. The CFA was conducted to evaluate the factorial validity of the SRI-25. Several fit indices were used to assess model adequacy, including the chi-square statistic (χ2), the ratio of chi-square to degrees of freedom (CMIN/DF), Comparative Fit Index (CFI), Tucker-Lewis Index (TLI), root mean square error of approximation (RMSEA) with its 95% confidence interval (CI), and standardized root mean square residual (SRMR). Acceptable model fit was considered: The CMIN/DF values < 3, CFI and TLI values > 0.90, RMSEA values < 0.08, and SRMR values < 0.08 (29). Convergent and discriminant validity were examined using average variance extracted (AVE) and composite reliability (CR). Concurrent validity was assessed by correlating SRI-25 scores with measures of anxiety, depression, and hopelessness. Logistic regression analyses examined associations between SRI-25 (or its subscales) and binary outcomes, reporting odds ratios (ORs) and 95% confidence intervals. Reliability was evaluated using Cronbach’s alpha and McDonald’s omega.
4. Results
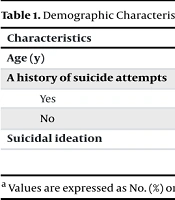
Among 9,000 students, 918 exhibited suicidal ideation, and 121 had a history of suicide attempts. The demographic characteristics of the study samples are listed in Table 1. This table presents the demographic data of adolescents who attempted suicide, with a total sample size of 121 participants. The mean age for both males (15.57 years, SD = 1.72) and females (15.56 years, SD = 1.65) is similar, indicating no significant age difference between genders.
| Characteristics | Male | Female | Total |
|---|---|---|---|
| Age (y) | 15.57 ± 1.72 | 15.56 ± 1.65 | 15.59 ± 1.58 |
| A history of suicide attempts | |||
| Yes | 56 (46.3) | 65 (53.7) | 121 |
| No | 5400 (49.2) | 5556 (50.8) | 10956 |
| Suicidal ideation | 475 (51.7) | 443 (48.3) | 918 |
a Values are expressed as No. (%) or mean ± SD.
4.1. Exploratory Factor Analysis-Suicide Resilience Inventory-25
The statistical values of the Kaiser-Meyer-Olkin (KMO) test (KMO = 0.935) and Bartlett’s test of sphericity (χ2 = 4824.787, df = 300, P < 0.001) confirmed the adequacy of the sample for EFA. Table 2 displays the eigenvalues and the proportion of variance explained by each factor, as identified through EFA. The SRI-25 demonstrated a three-factor structure with eigenvalues greater than 1, collectively accounting for 60.223% of the total variance. The first factor comprised 10 items (items 1 - 10), the second factor included 9 items (items 11 - 19), and the third factor consisted of 7 items (items 19 - 25).
| Components | Extraction Sums of Squared Loadings | Rotation Sums of Squared Loadings | α (CR) | ||||
|---|---|---|---|---|---|---|---|
| Total | % of Variance | Cumulative % | Total | % of Variance | Cumulative % | ||
| IP | 10.830 | 43.318 | 43.318 | 5.546 | 22.184 | 22.184 | 0.90 (0.91) |
| ES | 2.491 | 9.966 | 53.284 | 5.298 | 21.190 | 43.375 | 0.93 (0.88) |
| EP | 1.735 | 6.939 | 60.223 | 4.212 | 16.849 | 60.223 | 0.87 (0.85) |
Abbreviations: IP, internal protection; ES, emotional stability; EP, external protection.
As shown in Table 2, based on the total rotated factor loadings, the first factor — with an eigenvalue of 5.546 — explained 22.184% of the total variance in the SRI-25. The second factor, with an eigenvalue of 5.298, accounted for 21.190% of the variance, and the third factor, with an eigenvalue of 4.212, explained 16.849% of the variance. Together, these three factors explained 60.223% of the total variance in the questionnaire. As shown in Table 3, since the factor loadings for all items exceeded 0.30, it can be concluded that the items effectively measure their respective constructs within each factor.
| SRI-25 | Internal Protection | Emotional Stability | External Protection |
|---|---|---|---|
| Item 1 | 0.64 | - | - |
| Item 2 | 0.62 | - | - |
| Item 3 | 0.75 | - | - |
| Item 4 | 0.52 | - | - |
| Item 5 | 0.61 | - | - |
| Item 6 | 0.73 | - | - |
| Item 7 | 0.57 | - | - |
| Item 8 | 0.54 | - | - |
| Item 9 | 0.58 | - | - |
| Item 10 | 0.69 | - | - |
| Item 11 | - | 0.63 | - |
| Item 12 | - | 0.67 | - |
| Item 13 | - | 0.79 | - |
| Item 14 | - | 0.81 | - |
| Item 15 | - | 0.80 | - |
| Item 16 | - | 0.61 | - |
| Item 17 | - | 0.75 | - |
| Item 18 | - | 0.71 | - |
| Item 19 | - | 0.67 | - |
| Item 20 | - | - | 0.69 |
| Item 21 | - | - | 0.78 |
| Item 22 | - | - | 0.78 |
| Item 23 | - | - | 0.56 |
| Item 24 | - | - | 0.67 |
| Item 25 | - | - | 0.50 |
| Reliability | (α = 0.90 and ω = 0.90) | (α = 0.94 and ω = 0.93) | (α = 0.87 and ω = 0.87) |
Abbreviation: SRI-25, Suicide Resilience Inventory-25.
As shown in Table 3, all factor loadings for the questionnaire items in the EFA exceeded 0.40, supporting the construct validity of the instrument. In terms of reliability, Cronbach’s alpha and McDonald’s omega coefficients indicated excellent internal consistency for the subscales: Internal protection (α = 0.90, ω = 0.90), emotional stability (α = 0.93, ω = 0.94), and external protection (α = 0.87, ω = 0.87). For the total scale, Cronbach’s alpha and omega were 0.92 and 0.94, respectively.
4.2. Confirmatory Factor Analysis-Suicide Resilience Inventory-25
Both the three-factor and second-order CFA models showed acceptable fit (χ2 = 736.61, df = 270, P = 0.001, CMIN/DF = 2.73, RMSEA = 0.05, CFI = 0.927/0.925, TLI = 0.920/0.919, SRMR = 0.06), confirming the adequacy and stability of the model structure (Table 4).
| Variables | χ2 | df | CMIN/DF | P-Value | RMSEA (IC 95%) | CFI | TLI | SRMR | AIC | CR |
|---|---|---|---|---|---|---|---|---|---|---|
| Three-factor | 736.610 | 270 | 2.73 | 0.001 | 0.05 (0.04, 0.07) | 0.927 | 0.920 | 0.06 | 45751.7 | 0.94 |
| Second-order CFA | 736.610 | 270 | 2.73 | 0.001 | 0.05 (0.04, 0.057) | 0.925 | 0.919 | 0.06 | 45751.8 | 0.91 |
Abbreviations: χ², chi-square statistic; df, degrees of freedom; CMIN/DF, chi-square divided by degrees of freedom; RMSEA, root mean square error of approximation with 95% CI; CFI, Comparative Fit Index; TLI, Tucker-Lewis Index; SRMR, standardized root mean square residual; AIC, Akaike information criterion; CR, composite reliability.
The fit indices for both the three-factor and second-order CFA models indicate an acceptable model fit. The chi-square value was significant, which is expected with large sample sizes. The CMIN/DF values for both models were below 3, demonstrating an appropriate fit. The RMSEA values of 0.05 (with narrow confidence intervals) suggest a close approximation to the population covariance structure. Both CFI and TLI values exceeded 0.90, supporting satisfactory model fit, and the SRMR values (0.06) were comfortably below the recommended threshold of 0.08. The AIC values facilitate comparison between alternative models. Overall, these results confirm that the proposed factor structures adequately fit the data.
4.3. Convergent Validity
The AVE provided acceptable convergent validity for the internal protective factor (AVE = 0.69), emotional stability (AVE = 0.79), and external protective factor (AVE = 0.73). The CR for the entire questionnaire was 0.96, with CR values of 0.91 for internal protective, 0.88 for emotional stability, and 0.85 for external protective, all exceeding the threshold of 0.70 (CR > AVE). This indicates acceptable internal consistency for the items in the SRI-25 scale. The Cronbach’s alpha coefficient (α) for the entire scale was 0.94, demonstrating good internal consistency (30).
4.4. Concurrent Validity
As shown in Table 5, the results of the correlation analysis demonstrated significant negative associations between suicide resilience and its subscales with depression, anxiety, and hopelessness, further supporting the concurrent validity of the SRI-25 in adolescents.
Abbreviations: IP, internal protection; ES, emotional stability; EP, external protection; SRI-25, Suicide Resilience Inventory-25; DP, depression; AX, anxiety; HP, hopelessness; SI, suicidal ideation.
a P ≤ 0.01.
4.5. Discriminant Validity
Discriminant validity was examined through logistic regression analysis comparing the SRI-25 scores between adolescents with a history of suicide attempt (SA group) and normal controls (N = 121 per group). The findings are presented in Table 6.
| Step | Groups | SA | Normal | % | Variables | B (S.E) | Wald | P-Value | 95% CI For EXP (B) | ||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Exp (B) | Lower | Upper | |||||||||
| 1 | Suicide attempt | 106 | 15 | 87.6 | EP | -0.155 (.057) | 7.49 | 0.001 | 0.58 | 0.76 | 0.95 |
| Normal | 20 | 101 | 83.5 | ||||||||
| Overall percentage | - | - | 85.5 | SRI-25 | 0.109 (.016) | 44.69 | 0.001 | 1.11 | 1.08 | 1.15 | |
| 2 | Suicide attempt | 105 | 16 | 86.8 | |||||||
| Normal | 19 | 102 | 84.3 | Constant | -6.08 | 67.79 | 0.001 | .002 | - | - | |
| Overall percentage | - | - | 85.5 | ||||||||
Abbreviations: SA, suicide attempt; Exp(B), exponentiated coefficient; B, unstandardized coefficient; S.E, standard error; Wald, Wald test statistic; SRI-25, Suicide Resilience Inventory-25.
In the first step, emotional protection (EP) significantly predicted group membership [Wald = 7.49, P = 0.001, Exp(B) = 0.58, 95% CI: 0.76 - 0.95], indicating that higher EP scores were associated with lower odds of being in the suicide attempt group and demonstrating the scale’s ability to discriminate between groups. In the second step, the total SRI-25 score was a significant predictor of group membership [Wald = 44.69, P = 0.001, Exp(B) = 1.11, 95% CI: 1.08 - 1.15]. This suggests that higher resilience, as measured by the SRI-25, is significantly associated with a reduced likelihood of being in the suicide attempt group. Overall classification accuracy was high (85.5%), further supporting discriminant validity.
5. Discussion
The findings of the present study provide robust empirical support for the three-factor structure of the SRI-25, encompassing external protective factor, internal protective factor, and emotional stability dimensions. This factorial structure is consistent with prior psychometric research, including Fang et al., validating the instrument in other populations. Our confirmation of this model in the Persian version highlights the cross-cultural robustness of the SRI-25. Originally developed and validated in English, the SRI-25 has consistently demonstrated its efficacy as a multidimensional measure of suicide resilience in adolescent populations across diverse cultural contexts (9, 21).
Internal consistency indices were outstanding, with CR of 0.96 and Cronbach’s alpha coefficient (α = 0.94), both exceeding established psychometric benchmarks (31). The SRI-25 exhibited robust discriminant validity, evidenced by logistic regression analyses indicating that the scale significantly differentiated between the suicide attempt and non-attempt groups, with an overall classification accuracy of 85.5%. Concurrent validity was also confirmed by significant negative correlations with anxiety, depression, hopelessness, and suicidal ideation measures (all P < 0.001), supporting the instrument’s clinical relevance and convergent properties (9).
While the three-factor structure of the SRI-25 was psychometrically sound in this Iranian sample, we acknowledge that the initial assertion of suicide resilience as a wholly “culture-transcendent” phenomenon was an overgeneralization. The generalizability of suicide resilience-related protective mechanisms must be interpreted with caution, as sociocultural determinants exert substantial influence on the manifestation and development of resilience. For instance, in the Iranian context, previous studies highlight the centrality of familial support, religious faith, and collective social identity in shaping suicide resilience among adolescents (32). Therefore, while the core constructs assessed by the SRI-25 may remain stable across cultures, their sources, expression, and functional significance are inextricably tied to cultural, familial, and societal contexts (33).
Collectively, these results suggest that suicide resilience, as assessed by the SRI-25, is conceptually coherent across cultural settings, yet the mechanisms and contextual meaning of resilience-related resources are shaped by local norms, values, and support systems (34).
5.1. Conclusions
The present study demonstrated that the Persian version of the SRI-25 is a psychometrically sound instrument for assessing suicide resilience among Iranian adolescents. Its strong reliability and discriminant validity support its clinical utility for the identification of at-risk youth in real-world settings. Employing the SRI-25 enables clinicians to systematically detect protective factors and to design targeted, evidence-based, and culturally informed interventions for suicide prevention and treatment. Therefore, the SRI-25 can meaningfully enhance clinical assessment, early screening, and the effective management of adolescents at risk for suicidal behaviors.
5.2. Limitations and Future Directions
This study was conducted in a single province and exclusively among adolescents at high risk for suicide (SPS ≥ 27), which may limit the generalizability of the findings — particularly since all participants were drawn from a high-risk student group, and it remains unclear to what extent these results apply to populations with lower risk. The exclusive reliance on self-report data may also increase the risk of response bias; therefore, future studies are recommended to employ more diverse sampling and data collection methods. Furthermore, test-retest reliability and sensitivity to change were not assessed in this research, and future studies should evaluate these psychometric properties, especially in longitudinal and intervention designs. Finally, to more accurately assess potential cultural and linguistic biases, it is suggested that future research utilize structured clinical interviews with adolescents.