1. Background
Alcohol is a major contributor to mortality and morbidity in South Asian region (1). It is generally believed that a large number of people suffering from alcohol use disorders either do not seek treatment or do so very late in the course of their illness. Moreover, those consulting may not receive adequate treatment or appropriate referrals to higher centers.
There is limited literature that has explored pathways to care among individuals with substance dependence globally (2). Majority of such studies have had rather heterogeneous samples. While majority failed to include individuals with alcohol dependence, others have included individuals with alcohol dependence as a small proportion of the overall sample. The proportion of subjects with alcohol dependence in such studies has varied from 0% - 16% (3, 4).
We could come across only one study that has reported pathways to care exclusively among individuals with alcohol use disorder (5). Commander et al. (5) studied the pathways to psychiatric care for alcohol use disorders using the Goldberg-Huxley model (6) as the framework in a district in England. They assessed the help seeking and referral patterns across five levels viz. community (level 1); primary care: total morbidity (level 2); at primary care: conspicuous morbidity (level 3), specialist service use (levels 4); and in-patient care (level 5). On analyzing the ratios of patients moving upwards to a higher level (in other words, the function of filters), it turned out that about half progress at the first two filters and about one-tenth progress at the last two filters each. The study demonstrated that even in developed countries, only half of those with alcohol use problems ever seek even primary care help. The figures given above demonstrated that only a miniscule proportion of these patients receive specialist attention.
2. Objectives
Need to study pathway to care in Indian settings among patients with mental disorders has been expressed by researchers earlier as well (7). However, there is no published literature that has specifically explored pathway to care among individuals with alcohol use disorder in India. In the present study, the authors explored pathways to care traversed by patients with alcohol use disorders seeking help at a tertiary care substance use disorder treatment center.
3. Patients and Methods
It was a cross-sectional, observational study. Patients fulfilling DSM-IV-TR criteria for alcohol dependence were recruited from a tertiary care de-addiction center. Patients in age range of 18 - 60 years, seeking treatment at the substance use disorder treatment center, willing to provide a written informed consent were recruited. While those with any other comorbid substance use fulfilling DSM-IV-TR criteria for dependence or abuse (other than nicotine), in state of intoxication and those refusing to provide informed consent were excluded from the study.
3.1. Study Questionnaires
3.1.1. Semi-Structured Proforma
Information on socio-demographic profile of the patients was collected using a semi-structured proforma.
3.1.2. World Health Organization Encounter Form
Data on pathways to care were collected using the encounter form used in WHO Pathway Study and thereafter extensively used in ‘pathway to care’ studies across different settings and countries (3, 8). It is a culture neutral questionnaire designed to systematically assess sources of care used by patients before consulting mental health professional. The items included in the questionnaire gather information on profession of each previous carer, length of time since the patient was first seen and the main problem, source of referral, main treatment offered and duration of the patient's journey to see the carer.
3.2. Data Analysis
The data obtained were analyzed using SPSS version 21 (IBM SPSS Statistics for Windows, Version 21.0. Armonk, NY: IBM Corp.). Categorical data were compared using the chi-squared test. The Kolmogorov-Smirnov test (Lilliefors Significance Criterion) was used to determine the normality of the data. The t-test was used to compare continuous data with normal distribution whereas the Mann-Whitney test was used where the distribution was found to be nonnormal. The level of statistical significance was kept at P <0.05 for all the tests.
The ethical clearance for the study was obtained from the institutional ethics committee.
4. Results
4.1. Socio-Demographic Profile and Substance Use Characteristics
The socio-demographic characteristics of the patients are shown in Table 1. The patients were mostly young, married and more often than not from joint families. There were no statistically significant differences between those seeking help from the tertiary level substance use disorder treatment center directly for the first time ever in their lives when compared to those who have had multiple previous help seeking attempts from other treatment facilities except for the travelling time (from their homes) to our center. Those seeking help for the first time lived closer to the tertiary care de-addiction center with a median travelling time of 0.5 hours (IQR = 1.77) whereas those with prior help seeking attempts from other health services lived farther with a median travelling time of 1.5 hours (IQR = 2.75) from the center.
| Patients Visiting Tertiary Care Center Directly (n = 33) | Patients Visiting Tertiary Care Center Indirectly (n = 25) | P Value | |
|---|---|---|---|
| Age, y (Mean ± SD) | 33.7 ± 9.70 | 35.08 ± 8.01 | 0.57 |
| Distance from center (in hours) [Median(IQR)] | 0.50 (1.77) | 1.50 (2.75) | 0.05 |
| Marital status | |||
| Unmarried | 18.18% | 24% | |
| Married | 78.78% | 72% | 0.55 |
| Widower/separated | 3.03% | 4% | |
| Education | 0.76 | ||
| Illiterate | 3.03% | 8% | |
| Up to primary | 24.24% | 12% | |
| Middle school | 24.24% | 28% | |
| Intermediate | 27.27% | 24% | |
| Graduation and above | 21.21% | 28% | |
| Employment | |||
| Never employed | 0 | 4% | |
| Presently Unemployed | 18.18% | 24% | |
| Full time employed | 27.27% | 28% | 0.50 |
| Others | 54.54% | 36% | |
| Living arrangement | |||
| Joint family | 60.60% | 48% | 0.43 |
| Nuclear family | 39.39% | 52% |
Socio-Demographic Profile of the Study Subjects
The substance use characteristics of the patients are shown in Table 2. There were no significant differences in the substance use characteristics between those seeking help at a tertiary care center at first level of contact and those seeking tertiary care at second or subsequent contacts.
| Patients Visiting Tertiary Center Directly (n = 33) [Median(IQR)] | Patients Visiting Tertiary Center Indirectly (n = 25) [Median(IQR)] | P value | |
|---|---|---|---|
| Median age of onset of alcohol use (in years) | 20.00 (11) | 20.00 (8) | 0.99 |
| Median duration of alcohol use (in years) | 9.00 (13) | 14.00 (8) | 0.16 |
| Median age of onset of tobacco use (in years) | 18.00 (7) | 20.00 (4) | 0.57 |
| Mean duration of tobacco use (in years) | 13.84 ± 8.03 | 17.25 ± 8.10 | 0.13 |
Substance Use Characteristics of the Study Subjects
4.2. Pathways to Care
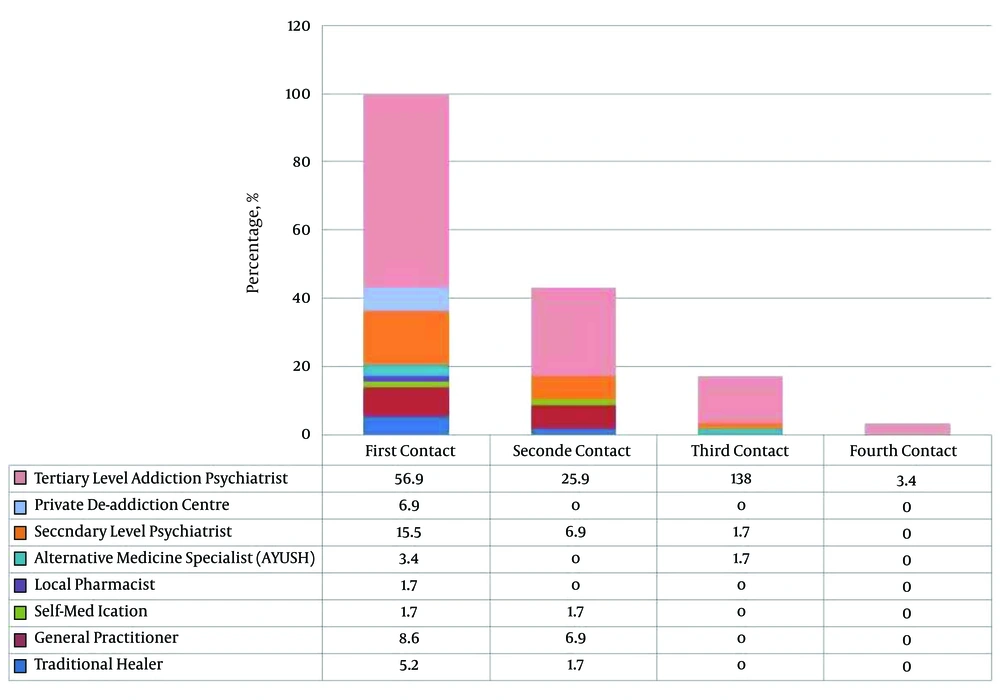
The patients consulted a number of care providers with several consulting more than one provider. The details are as shown in Figure 1. For 56.9% of the subjects, first point of contact was with a tertiary care addiction psychiatrist, 15.5% with a secondary level psychiatrist and 8.6% with a general practitioner. Traditional healers were consulted by about 5.2% of the patients seeking help for the first time. At all levels of contact with health services, the largest group comprised those consulting a tertiary care addiction psychiatrist, followed by a secondary care psychiatrist with some exceptions.
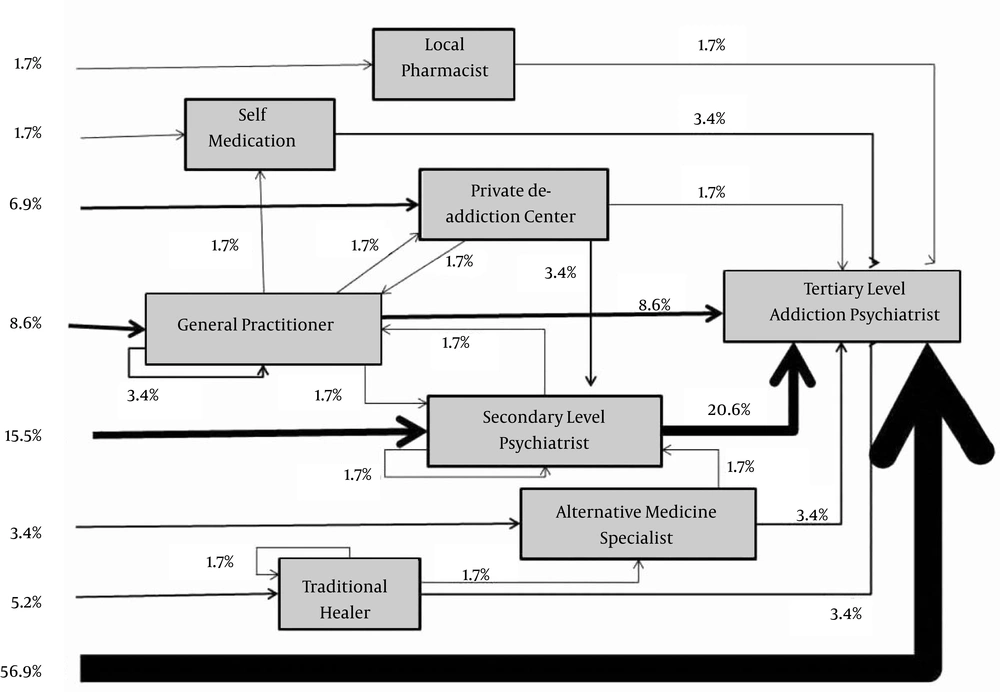
The pathway to care followed by the study subjects has been represented in Figure 2.
The mean duration of main problem due to alcohol use was 5.82 ± 4.95 years. The temporal pattern and travel time for various help seeking attempts are shown in Table 3. The first contact tended to be at place nearer to the patient’s residence while further contacts tended to be farther away. A comparison of the travelling times of those seeking tertiary care de-addiction service consultation at first level of contact (median = 0.5 hours, IQR = 1.68) vis-a-vis consultations from other health services at first level of contact (median = 1.00 hours, IQR = 1.75) revealed no statistically significant differences (P = 0.22). There were no differences between above two groups on any socio-demographic or clinical parameters.
| Time lapse between treatment contacts (in years) (Mean ± SD) | Duration of journey to health services (in hours) (Mean ± SD) | |
|---|---|---|
| First contact | 0.93 ± 1.46 | 1.55 ± 2.21 |
| Second contact | 0.50 ± 0.92 | 3.27 ± 5.39 |
| Third contact | 1.10 ± 3.14 | 3.00 ± 4.70 |
Temporal Pattern and Travel Duration of Help Seeking Attempts by the Study Subjects
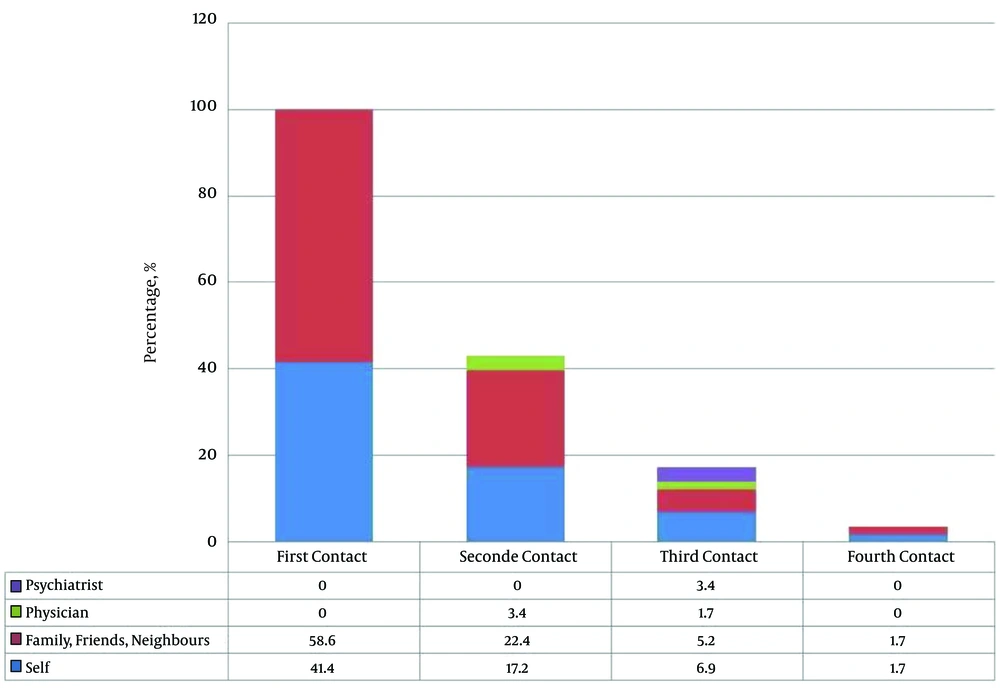
The source of referral for study subjects is shown in Figure 3.
Family, friends and neighbours together constituted the single largest group suggesting care to be sought (or referring) by the patients except at the third contact, where a marginally larger number of patients referred themselves.
5. Discussion
This is the first study from India to systematically assess the pathways to care among patients diagnosed with alcohol dependence syndrome. In spite of the experts’ opinions on need for pathway to care study in Indian setting for individuals with mental disorders, none has yet been conducted among alcohol dependent individuals (7). The current study found that the help-seeking attempt at a tertiary care center varied from a median of 9 years (direct contact) to a median of 14 years (indirect contact) after the onset of alcohol use. These findings reiterate the point raised by Commander et al. (5) regarding the unsatisfactory help seeking behaviour as well as the abysmally small number of patients availing appropriate health services. Interestingly though, in the current study, well over half the sample had consulted a tertiary level addiction psychiatrist at first level of contact with health services and a sizeable number had consulted a secondary level psychiatrist. About one-fourth of the sample had consulted a tertiary level addiction psychiatrist at second contact. The number of patients consulting general practitioners, traditional healers and pharmacists was pretty low in the current study. Even prior to the contact at our center, a sizeable number had consulted a psychiatrist. These findings, in a sense, appear to contradict those of Commander et al. (5) This discrepancy could possibly be partly attributed to the fact that this sample was recruited from a tertiary care center and may have preferably picked those patients, who, for various reasons, may have had an inclination to consult a specialist. However, a closer scrutiny of previous literature suggests alternative explanation as discussed subsequently.
Although no previous studies from India have explored pathways to care exclusively among individuals with alcohol use disorder, there are a few that have focused on other psychiatric disorders (9-11). A multi-national study (12) with one center in India also included subjects with substance use disorders (18% of sample). All these studies have been conducted among clinical populations in tertiary care teaching hospitals from India. Lahariya et al. (10) reported that only around nine percent of the patients in their study sought help directly from a psychiatrist. Agrawal et al. (9) also observed that only a small fraction of the patients with mental disorders sought help directly from a psychiatrist. On the contrary, more than seventy percent of the subjects sought help directly from a psychiatrist in the current study. The findings of these previous studies which were also recruited from tertiary care centers indicate that the nature of the sample alone cannot explain the discrepant findings of the current study. Thus, the observation in the current study is contrary to the earlier expressed views highlighting limited direct access to psychiatric services after the onset of illness in India (7). This observation from the current study possibly implies that in case of substance use disorders (alcohol dependence), the rate of nonspecialist help seeking may actually be much less than that observed for other psychiatric disorders. Interestingly around two-third (6/9) of the subjects with substance use disorders as compared to only 27% of subjects with other psychiatric disorders from the Indian site in the multinational study by Hashimoto et al. (12) also sought help directly form a psychiatrist. This observation also adds support to aforementioned hypothesis. A possible explanation could be the lack of service providers who are willing to treat substance use problems, which might have forced these patients to seek help at a specialized center such as ours.
Possibility of difference in pathways to care based on the psychiatric diagnosis has been expressed earlier as well. A study from northern part of the country reported psychiatrist to be the first doctor consulted by 58% of the patients (13). Additionally, almost one-third of them sought help from faith healers at first contact. About 90% of the sample in the study was constituted by psychotic and mood disorders explaining the nature of help-seeking. Another study from a tertiary care setting (that did not include patients with substance use disorders) reported a high rate (44%) of first contact with a nonpsychiatrist physician (11). Around 43% of the sample (constituting the largest subset) had a diagnosis of somatoform disorder explaining this help-seeking pattern. The authors argued that the difference in psychiatric diagnoses across these studies and the earlier studies from the country could explain the difference in the preferred first point of contact in help seeking pathway. Hence, it is important to study pathway to care separately for individuals diagnosed with different psychiatric disorders including substance use disorders.
Another common observation across previous Indian studies has been a high rate of help seeking from faith healers and religious healers. Lahariya et al. (10) reported that 68.5% of the cases first consulted faith healers. Agrawal et al. (9) also observed that there was a very high rate of help seeking from faith healers, traditional medicine practitioners and quacks for mental disorders other than substance use disorders. However, as mentioned earlier, these studies did not include patients with substance use disorders. Direct help seeking from faith healer in the current study was low at five percent. Interestingly, a similar low rate of 11% among patients with substance use disorders (as compared to 19% for other psychiatric disorders) was observed at the Indian site of the study by Hashimoto et al. (12) This observation also lends support to possibility of different pathways to care among patients with different psychiatric disorder including substance use disorders.
Only a small proportion of subjects (5%) visited a practitioner of alternate system of medicine in the current study. This is comparable to the low rates observed in the earlier studies (9, 10). It seems that most of the patients with psychiatric disorders (including substance use disorders) do not seek treatment from alternate systems of medicine in these regions of the country. This observation has important policy implication as over the past few years there has been a growing emphasis on promotion of alternate systems of medicine across the country.
Contradiction between findings of the current study and that by Commander et al. (5) could be explained by the vast differences in the health care system of India and England. It is possible that the treatment provided by nonspecialists for substance use disorders in India may have been perceived as unattractive or ineffective by patients; or that nonspecialists might prefer treating other disorders rather than substance use disorders. For instance, in case of psychotic disorders, the various socio-cultural beliefs regarding its causation make consulting a faith healer an obvious choice for a large number of people but the same is not true for substance use disorders. Yet another possibility could be that there may have been underreporting of prior help seeking attempts in this population.
Another important finding of the current study was that the only significant difference between patients visiting tertiary care center directly and those visiting indirectly was the distance from the center. All other parameters including the age at onset and duration of substance use (and therefore possibly the severity) were not significantly different. This finding has major implications from a public health perspective. It is likely that the utilization of specialized services is likely to be high if such services are made available closer to the place of stay. The fact that the mean travel duration even for the first contact was about 1.55 hours reflects limited availability and poor accessibility of treatment services for substance use disorders. Although developing more centers for treatment of substance use disorders (and thereby decreasing distance to the center) seems like a logical option, building of such stand-alone services may not be cost effective. Therefore, integration of substance use disorder treatment to primary health care services seems to be a better option. Effectiveness and feasibility of community-based service delivery for substance use disorder has been documented in the Indian setting previously (14-16).
Family, friends and neighbours suggested referral in an overwhelming majority of cases, far outnumbering those by doctors or patients themselves. Similar observation was also reported by earlier Indian study as well (10). This probably reflects the strong familial and societal ties seen in Indian patients. However, the low number of referrals by doctors probably reflects a poor referral mechanism in our health system. A related implication of this observation is an underutilization of primary and secondary care centers and consequent overburdening of tertiary care centers. In the wake of these findings, one needs to revisit the validity of the Goldberg-Huxley model for Indian settings. This model draws heavily from the systematic referral system in place in developed countries. As has been seen, such systematic referral system is not functional in India, at least for alcohol use disorders.
The current study, besides being the first of its kind to be conducted in India, also replicates and confirms some of the findings from western studies in Indian setting. More importantly, it also questions some aspects that had been widely regarded to be true in India and demonstrated in western studies. Therefore, the current study also makes a larger point by reminding us of the need and importance of systematic data and also that the western data cannot be directly applied to Indian settings in all cases. Notwithstanding the stated need for future studies, it provides an evidence-based platform for addressing the lacunae in our health care delivery system.
The study reported findings from a single site that included a small sample of only male subjects. There is a need to replicate findings at other sites, with larger samples as well as to study female subjects before the results could be generalized. Future research should also aim at following up these subjects as well as to determine barriers to help seeking which would be of immense help in planning effective mental health interventions.
5.1. Conclusions
Pathways to care for patients diagnosed with alcohol use disorders represent a crucial link in the overall scheme of health care delivery for these disorders. In India, the situation appears to be less than satisfactory. There is a long time lag between the onset of alcohol use related problems and the first help seeking attempt, even if it was from a nonspecialist. The patients often have to travel long distances to avail treatment. However, of those who do decide to seek help, the proportion of those obtaining specialist help may be higher than believed. Referral by the health service providers is low and patients are mostly referred by family, friends and neighbours. Distance from treatment center is a crucial factor in treatment seeking and integration of substance use disorder treatment services into primary health care services will go a long way in improving help seeking patterns.