1. Background
Erectile dysfunction refers to men’s failure to achieve or maintain full erection to the end of coitus (1). Sexual dysfunction is difficulty experienced by an individual or a couple throughout any phase of normal sexual activity, including physical pleasure, desire, preference, arousal, or orgasm (2). Sexual dysfunction can have a profound impact on a person’s perceived quality of sexual life (3).
Opiate abuse has increased in prevalence in recent years throughout the world, especially in Iran (4, 5). Opium and its derivatives have a long history in Iranian tradition, so that pharmacological, psychotropic effects found in people with difficulties (6). Research indicates that opium was the first drug used by 46.4% of the subjects (7). Although opium use has been reported in Iran for centuries, it has evolved into a complex matter involving widespread psychosocial, familial, and economic consequences. There is no clear evidence of the actual number of drug abusers in Iran. However, some reports estimate a probable presence of two to four million people. In addition, the current, formally announced number of drug abusers in Iran is about two million (8, 9).
Methadone maintenance therapy (MMT) is a well-known method of treating dependence on opioid raw materials and, in particular, is used to decrease the damage caused by these substances (10). Methadone has two enantiomeric forms: the racemic formula is used more regularly (11). MMT has been the foundation of pharmacologic management of opiate dependence (12-15). Methadone, a synthetic sedative drug used for the treatment of opium addiction, is also used instead of morphine and hydromorphone for patients suffering from severe pain (16).
Sexual dysfunction is a common and clinical side effect of heroin misuse and opiate-substitute treatment, because opium can cause atrophy and declining libido (17). Chronic opiate addicts experience sexual dysfunction including reduced libido and sexual performance in males and females, erectile dysfunction and delayed ejaculation in males (18), and amenorrhea and reduced fertility in females (19-24). These side-effects are often neglected and, therefore, unexplored in the routine clinical care of opiate addicts. Yet, they are highly clinically related, as they could lead to non-adherence to treatment (25).
Research indicates that heroin and methadone cause a drop in testosterone levels in males. Plasma testosterone levels have been revealed to be lower in opiate addicts, as compared with controls (26). Patients on lower doses of heroin and methadone have been found to have higher testosterone levels (27). In addition, various studies have shown the effect of heroin and methadone on testosterone levels in males. Other explanations offered to clarify opiate-induced sexual dysfunction include the a-adrenergic blocking activity of opiates, which may directly influence the functioning of accessory sex organs, and psychological factors, such as sedation, euphoria, and a chaotic lifestyle in addicts that inhibits sexual desire and performance. These patients may prefer drug-procuring behaviors to opportunities for sexual encounters (20, 28).
Sexual dysfunction is a common problem among addicted Iranian opiate users who undergo MMT, but only a few studies on sexual dysfunction of methadone-treated patients have been undertaken in Iran and other countries. As a result, the importance of sexual dysfunction has been underestimated. Research studies in other countries have found that up to 87% of women and 85% of men who enter MMT have reported sexual difficulty while using opium.
However, many patients with sexual dysfunction do not report this issue to clinicians and many clinicians sense discomfort among patients about dealing with sexual problems. Of the few Iranian studies conducted on sexual dysfunction, Tatari et al. (2013) (29), in their study of 157 drug-dependent subjects, found the prevalence of erectile function to be 60.5% and sexual desire to be 70.7%. A study on the prevalence of erectile function among 201 Italian patients at seven methadone and buprenorphine maintenance treatment centers revealed that 24% of patients reported mild to moderate erectile dysfunction, and 18% reported severe erectile dysfunction (30).
The paucity of research on sexual dysfunction among patients on MMT in Iran and in other countries is a crucial concern. Assessment of sexual dysfunction in these patients is important, because identification and management of sexual dysfunction can increase compliance with the treatment procedure, the effectiveness of which is associated with more doses and a longer duration of treatment (31). The present study is designed to examine the prevalence of sexual dysfunction and to investigate whether there is a change in sexual dysfunction following six months of MMT, compared with baseline.
Previous studies reported the prevalence and kinds of sexual dysfunction in men on MMT for opioid dependence and described factors that may contribute to sexual dysfunction. While ED is not life-threatening, it may result in withdrawal from sexual intimacy and reduced quality of life (26).
Among the side-effects of heroin misuse and opiate-substitute treatment, sexual dysfunction is common and clinically significant. This is often ignored and, therefore, unknown in the routine clinical care of opiate addicts. Yet, it is yet highly clinically relevant, as it could lead to lack of adherence to treatment. Sexual dysfunctions noted in chronic opiate addicts include reduced libido and sexual performance in males (32), erectile dysfunction and delayed ejaculation (18), and amenorrhea and reduced fertility in females (20, 33).
Various assumptions have been used to explain sexual dysfunction in male opiate abusers. Cushman and Kreek (1972) (28) reported a negative correlation between high-dose methadone and low plasma testosterone levels. Apart from the effect of heroin and methadone on reducing testosterone levels in males, other causes used to explain opiate-induced sexual dysfunction include the a-adrenergic blocking activity of opiates, which may directly influence the functioning of accessory sex organs.
Psychological factors, such as sedation, euphoria, and the chaotic lifestyle of addicts can impair sexual desire and performance, and these patients often prefer drug-procuring behaviors to opportunities for sexual encounters. Several studies have identified a range of sexual dysfunctions in male patients addicted to heroin and those treated with methadone (34).
2. Objectives
In this study, we assessed the sexual functioning of male heroin users undergoing MMT.
3. Patients and Methods
3.1. Patients and Procedures
Patients were recruited from outpatient attendees at several MMT centers between June 2015 and February 2016. Male patients aged between 25 and 50 years, with a DSM-5 diagnosis of opiate dependence syndrome, who were dependent on heroin or were being prescribed methadone, were included in the study. Patients on methadone were required to have been using it for at least six months. The target was a sample size of 150 methadone users, and all serial attendees at the clinic were interviewed until this number was reached.
Patients were excluded from the study if they had any of the following: comorbid alcohol dependence, a chronic physical disorder, such as diabetes mellitus, hypertension, chronic pain, endocrine or urologic disorders, or rheumatoid arthritis. Participants were asked not to use antidepressants, neuroleptics, antipsychotics, sedatives, anxiolytics, or antiandrogens during the study, because of the negative effects of these medications on sexual function and the possibility of interference with the study process and goals. Participants in whom comorbidities were detected, including drug or alcohol use, severe hypertension or stress, hormonal problems due to medical or surgical conditions such as testicular surgery, or who suffered from neurological or metabolic problems or diabetes were excluded, because of the negative effects of these problems on the study procedure.
The interviews were conducted in quiet, comfortable settings. Each interview lasted approximately one hour. All eligible patients (on the basis of self-reports of drug use) were then subjected to a urinalysis for psychoactive substances to confirm their use of heroin and methadone and to exclude concurrent use of other psychoactive substances. A final number of 150 patients participated in the study.
3.2. Interview and Administrative Tools
A semi-structured interview was administered, which included questions on socio-demographics, drug use details, and sexual behavior. Next, the International Index of Erectile Function (IIEF-15) was administered upon admission to MMT (35).
The IIEF-15 is a reliable, multidimensional scale test that explores various aspects of sexual dysfunction (36). The test is self-administered and has 15 questions that examine 5 scales of erectile function, orgasmic function, sexual desire, intercourse satisfaction, and overall satisfaction. Maximum mean scores for the IIEF-15 are 75, and the maximum mean score for each scale is as follows: erectile function [30], orgasmic function [10], sexual desire [10], intercourse satisfaction [15], and overall satisfaction [10]. On the erectile function sub-scale, lower scores show worse erectile dysfunction, and higher scores indicate less dysfunction. The reliability and validity of IIEF-15 were standard in Iran in the study on the Farsi international index of erectile dysfunction and doppler ultrasonography, which evaluated male impotence (37).
The sexual self-efficacy scale–erectile functioning (SSES-E) is a short self-report measure of the cognitive aspect of erectile functioning and adjustment in men. It evaluates a man’s attitudes about his sexual and erectile competence in a variety of conditions. The scale may be fulfilled by a man to obtain self-ratings or by his partner to obtain verification. Self-efficacy refers to confidence in the belief that one can perform a certain task or behave adequately in a given situation (38). Sexual self-efficacy is of great concern to most men and a topic of increasing interest within an aging population.
The SSES-E yields a self-efficacy strength score obtained by summing the values in the Confidence column and dividing by 25 (the number of activities rated). Any activity not checked in the Can Do column is presumed to have a 0 confidence (i.e., strength) rating. Some are reluctant to use the 10-point interval, so any continuous number recorded may be used in the Confidence column. Higher scores indicate greater confidence in the man’s erectile competence (39).
3.3. Statistical Analysis
The statistical method used to analyze the data was the Mann-Whitney U test to reveal the changes that participants reported in their SD at admission to MMT (baseline), compared with six months of methadone treatment (post-assessment).
4. Results
The study included 150 married males who were between 25 and 50 years old (mean: 35.48; SD = 7.91). The majority of participants was employed and had education levels of diploma (n = 68; 45.3%) or bachelor’s degree (n = 50; 33.3%). Participants were on methadone, with the dose gradually increasing. Results showed that age, education, employment, and methadone treatment duration were not associated with sexual dysfunction prevalence (P > 0.05).
| Variables | N | Mean ± SD | Frequency (%) |
|---|---|---|---|
| Age | 35.48 ± 7.91 | ||
| 25 - 30 | 54 | 36 | |
| 31 - 40 | 55 | 36.66 | |
| 41 - 50 | 41 | 27.33 | |
| Occupation | |||
| Employed | 101 | 67.3 | |
| Unemployed | 49 | 32.7 | |
| Education | |||
| Secondary School | 34 | 16 | |
| Diploma | 68 | 45.3 | |
| Bachelor’s | 50 | 33.3 | |
| Post Graduate | 8 | 5.3 | |
| Marital status | |||
| Married | 83 | 55.3 | |
| Single | 67 | 44.7 | |
| History of Drug Use | |||
| Age of First Opioid Use | 19.28 ± 3.53 | ||
| Duration of Addiction | 16.19 ± 8.80 | ||
| Duration of Methadone Treatment (Month) | 3.28 ± 1.17 |
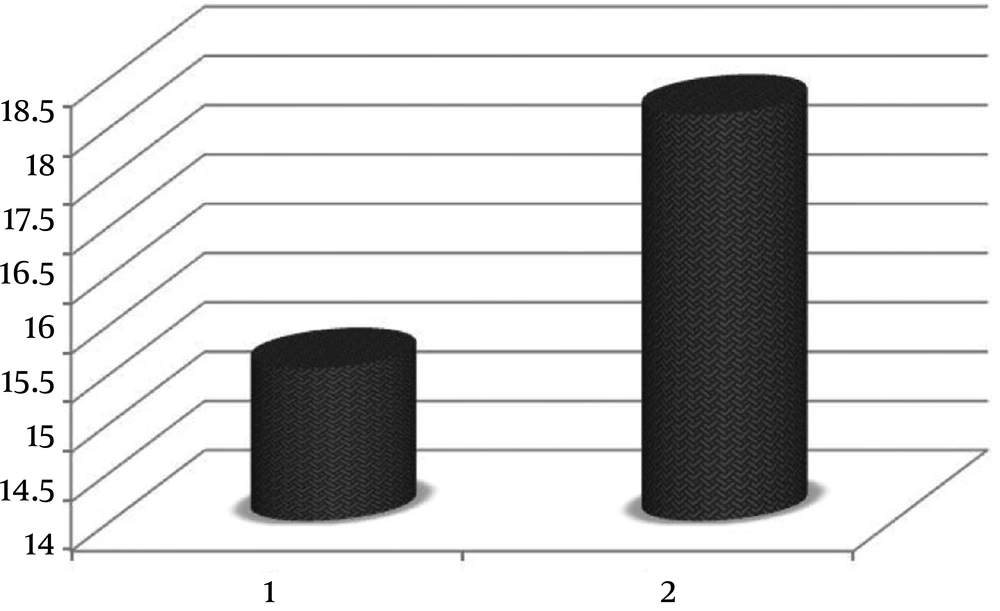
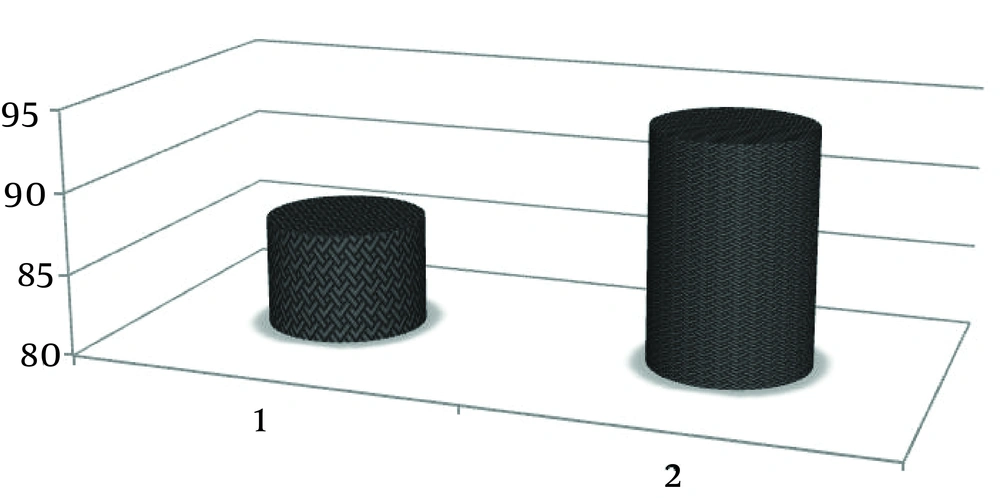
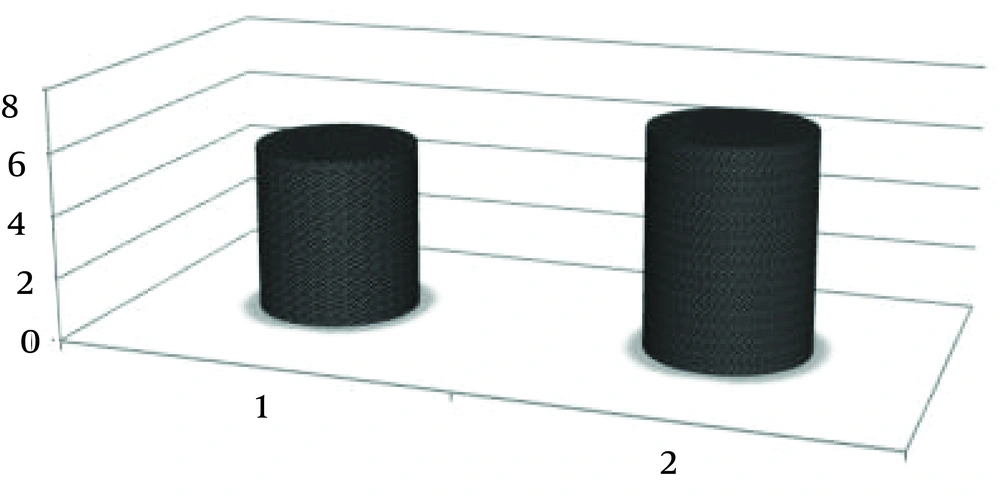
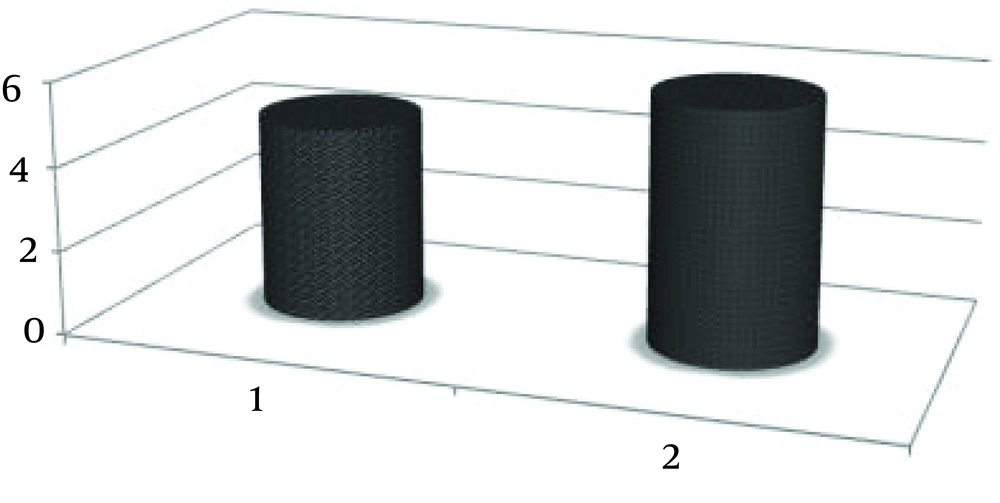
The baseline erectile dysfunction mean score on the IIEF was 15.55, which showed a moderate prevalence for erectile dysfunction among participants after taking methadone that positively increased to 18.12 in the post-assessment. Further analysis showed that the baseline orgasmic function score was 5.42, which increased moderately to 6.98 in the post-assessment (Table 2). The baseline sexual desire score was 4.66, which increased moderately to 5.90 in the post-assessment. Further analysis revealed a slight improvement in sexual desire among participants after taking methadone, compared with baseline (Table 2). The baseline overall satisfaction score was 4.79, which increased moderately to 5.85 in the post-assessment. The baseline erectile functioning (SSES-E) score was 86.71, which increased moderately to 94.34 in the post-assessment. Further analysis revealed overall sexual satisfaction and erectile functioning (SSES-E) among participants slightly improved after taking methadone, compared with baseline.
| Variable | Pre-Assessment, Mean ± SD | Post-Assessment, Mean ± SD | U | Z | P Value |
|---|---|---|---|---|---|
| Erectile function | 15.55 ± 2.08 | 18.12 ± 2.06 | 289.000 | 2.44 | 0.009 |
| Orgasmic function | 5.42 ± 3.89 | 6.98 ± 2.67 | 263.000 | 3.57 | 0.015 |
| Sexual desire | 4.66 ± 3.12 | 5.90 ± 2.40 | 245.000 | 2.39 | 0.017 |
| Overall satisfaction | 4.79 ± 2.76 | 5.85 ± 3.22 | 236.000 | 3.17 | 0.001 |
| Sexual self-efficacy (SSE) | 86.71 ± 10.09 | 94.34 ± 10.50 | 267.000 | 2.50 | 0.009 |
5. Discussion
This study showed that erectile dysfunction and other sexual dysfunctions have a very high prevalence in opioid-dependent males. Among men on MMT, 65% had erectile dysfunction (ED) and 27% had moderate to severe ED, 72.66% of whom were men younger than 40 and 27.34% of whom were aged 40+. The frequency of erectile dysfunction in the overall population is about 16.1% (40, 41).
One of the reasons for non-adherence to treatment with agonists useful in MMT relates to concerns about its sexual side-effects. We have found that sexual dysfunction is a common problem among opiate-dependent patients who are referred for treatment (30, 42). In the current study, the severity of some aspects of sexual dysfunction among participants decreased moderately after six months of extensive methadone treatment. Results indicated that orgasmic dysfunction was moderately prevalent. The research of Palha and Esteves (2002) (43, 44), who studied sexual dysfunction among 101 heroin addicts, found that 60% of men in their study had problems achieving orgasm. They also found that 75% of men in their study complained of low libido, 71% reported altered sexual arousal, and 72% had reduced sexual satisfaction. Additional treatment, such as androgen replacement therapy, might be necessary. In addition, these difficulties might have been the result of a variety of psychological and interpersonal factors not reported by participants.
Drug addiction is a nearly universal problem and crisis. This phenomenon has crossed geographical borders and destroyed many lives (45). Some scholars believe that addiction is the result of urban development, such as in the first and third regions in central Isfahan city (46). Public participation plays an important role in reducing this problem (23, 47, 48). Within Isfahan city, there are three urban social factors that can help reduce drug addiction (49): urban spirit assessment and its value to the city center (50), artistic and musical activities and creating a happy environment (51), and encouraging youth to know the history and traditions of their country and to feel proud of their culture (52).
5.1. Conclusion
In the present study, sexual problems slightly improved after participants took methadone. The long-term side-effects of opioid dependence on decreased libido were likely to be related to the core features of sexual desire and overall satisfaction. These possibly required additional therapies or could have been attributable to the disrupted affective and sexual relationship of participants with their spouses, requiring psycho-intervention, sex therapy, or marital therapy.
Several limitations existed in this study. This was cross-sectional research, without a control group, hormone assay, or monthly evaluation by IIEF-15. We used baseline sexual status to compare with post-assessment results of sexual function among participants. It was methadone use and improvement in sexual dysfunction from our observations in this pilot study. Additional studies with larger samples and lower dropout rates are necessary. Furthermore, our data was based on self-reporting, which lacked objective evidence. However, we administered the IIEF-15, which is recognized as the gold standard for evaluating sexual dysfunction (53). We evaluated sexual dysfunction at an appropriate time, in the sixth month, when our extensive interviews with patients showed they frequently reported having adjusted to both the methadone dose and treatment conditions in the MMT program.
The present study found no relationship between demographics, drug use history, and duration of MMT to improvement in sexual dysfunction. Nevertheless, a higher methadone dose and longer duration of MMT, in comparison with a low dose and shorter treatment duration in experimental and control groups, are subjects for future studies on sexual dysfunction in male patients, particularly given that some well-known studies have claimed the reverse effects of methadone treatment on certain aspects of sexual function, such as libido and orgasmic function (26).
Sexual dysfunction is an important concern for many patients undergoing MMT, and a good opiate use treatment program must address this issue. Androgen replacement (54) and pharmacological treatment may be effective approaches for these patients, while psycho-intervention for patients and counseling programs for couples may be useful (55-57).
This study showed that erectile dysfunction and other sexual dysfunctions have a very high prevalence in opioid-dependent males. This subject has drawn insufficient attention and is still unknown as a public health issue. In turn, this problem has its own effects on patients’ health and damages the prognosis for recovery from drug abuse. Moreover, addiction withdrawal centers are linked to this facet of patients’ health. Therefore, they should be forewarned about the side-effects and dysfunctions caused by opioids. In addition, explaining to addicts that methadone causes fewer complications than using illegal drugs can help prevent premature exit from MMT. Moreover, this matter should be recognized as a means of preventing addiction in the future.