1. Background
Opioid dependence is a complicated disorder, in which multiple factors interact to influence initiation of use, repeated use, addiction, and relapse (1). Relapse rate after opioid detoxification ranges from 72% to 88% after 12 to 36 months, despite multidisciplinary endeavors, although a 6-month controlled study showed lower relapse rate (32% to 70%) (1, 2).
Opioids induce long-lasting alterations in the nervous system. Some of these changes are responsible for the physical dependence that causes an aversive withdrawal syndrome when the central nervous system opioid levels decline. Other drug-induced changes that may persist for some time after withdrawal include a hyper responsiveness to stress, a reduced response for ordinary pleasurable events (hypophoria) and a persistent memory for conditions under which opioids were used. It is not yet clear whether these changes should be considered part of protracted withdrawal syndrome or whether they represent a distinct phenomenon (1). Chronic opioid addiction may lead to opposing opioid receptor responses in the Nucleus Accumbens during withdrawal, which may produce dysregulation in brain stress hormones (3). Persistent alterations in stress hormone systems, and receptor and/or neurotransmitter activity may represent a compensatory mechanism, involving neuro-adaptations aimed at restoring homoeostatic function in response to the presence of the drug. As such, these changes could contribute significantly to negative emotional states of acute drug withdrawal, as well as enhanced sensitivity to stressful stimuli, both of which could result in greater vulnerability to relapse during abstinence in humans (3-5).
Mood disorders, including bipolar disorders and depression, are amongst the most common psychiatric comorbidities in patients with substance use disorders; a portion of high rates of comorbid mood disorders and substance use disorders may be due to confounding of mood disorders and transient symptoms related to acute abuse and withdrawal. Chronic use of drugs, such as central nervous system depressants may lead to depressive symptoms while withdrawal from some drugs like benzodiazepines could lead to agitation and anxiety. Thus, before making a definitive diagnosis, it is best to wait until the patient has had a reasonable period of abstinence (6). A study found a 30% to 50% decrease in depression rating score from day one of abstinence to the end of the second week (7). Furthermore, the pathological effects of substance use disorder or mood disorder may increase risk of the other, for instance mood disorders may motivate individuals to resort to drugs and alcohol to cope with their negative affective states (6). Negative emotional states, such as anger, anxiety, depression, frustration, and boredom are associated with the highest rate of relapse (8).
Depression could be a significant risk factor for relapse as it may lead to self medication. Furthermore, major depressive disorder may become a conditional cue for drug use during abstinence (9).
2. Objectives
The researchers of the current study propose that depression is a significant risk factor for relapse after inpatient detoxification, for which they conducted this 1-year follow-up study to compare the relapsed with non-relapsed patient group with respect to their depressive symptoms.
3. Patients and Methods
The researchers conducted this study at the Department of Psychiatry (De-addiction unit), Sri Guru Ram Das institute of medical sciences and research, Vallah, Amritsar, Punjab, India over a 2-year time period (1st of January 2014 to 31st December 2015), after gaining permission from the institutional ethics committee. The inclusion criteria were a diagnosis of opioid dependence (as per ICD -10 criteria), admission for detoxification in the de-addiction unit from 1st of January 2014 to 31st of December 2015 and consenting to participate in the study. The exclusion criteria included refusal to consent, co-morbid other drug addictions (except tobacco), co-morbid other psychiatric or significant medical ailment, age of < 18 years, and known history of any adverse reaction to Naltrexone.
A total of 581 patients were admitted from 1st of January 2014 to 31st of December 2014, out of which 115 subjects met the defined exclusion criteria or did not meet the inclusion criteria. The remaining 466 patients were considered for the study. A detailed history was taken and socio-demographic Performa, including the 24-item Ham D scale (10) was completed for every patient. Average stay of subjects for detoxification varied from 2 to 4 weeks depending on withdrawal signs and symptoms. Inpatient detoxification was done as per the standard protocol and medications were gradually tapered off to stop after 1 to 3 weeks, except Quetiapine. Tab Quetiapine was used for affective symptoms as needed. After being abstinent from opioids for a minimum of 5 to 7 days, all patients were discharged on Tab Naltrexone 50 mg o.d. with or without Tab Quetiapine 50 - 200 mg/d, with regular weekly visits to the outpatient unit, for the next 1 year.
All the patients were interviewed with the 24-item Ham D Scale every 2 weeks for the next 1 year, by another psychiatrist, who was blind to the patient history, socio-demography, and ongoing medication. At least one attendant/caregiver was identified for every patient during inpatient stay, which was mostly a close family member and would stay with the patient. They were made responsible for supervising daily medication at home and were advised to make notes if they suspect their patient for any substance abuse. Urine test for drug abuse was done randomly to monitor relapse. A total of 2512 random samples were taken, out of which 103 were positive for opioids and they were considered as relapse cases. None of the patients were positive for any other substance abuse (except tobacco). Patients and their attendants were interviewed regarding relapse, which was defined as abuse of any substance, except tobacco. Alcohol abuse was also not reported by any patient or his attendant.
Adherence therapy was done at every visit by a trained psychologist, who was blind to Ham-D scores. Relapsed patients were compared with non-relapsed patients with respect to their socio-demographic variables as per performa and Ham D score. Patients, who were lost to follow up, were considered as relapse cases. Their last observations were carried forward to calculate the final data, rather than considering only the completed subjects, to avoid bias. The researchers tried to contact the cases by telephone to ask about their reason for loss to follow up.
Relapsed and non-relapsed groups were compared across the variables using chi square and independent t test and P values of < 0.05 were considered statistically significant.
4. Results
Socio-demographic profile All patients were male. As shown in Table 1, the majority of the patients was in the age range of 20 to 40 years and had a rural background. Most were married, and employed with low-income. Education level was predominantly above matriculation. No significant difference was found between relapsed and non-relapsed patients.
| Relapsed (N = 147) | Non Relapsed (N = 319) | Chi Square Value | Significant Level | |
|---|---|---|---|---|
| Age, y | 4.70 | Ns | ||
| Below 20 | 45 (30.61) | 70 (21.94) | ||
| 20 - 40 | 80 (54.42) | 195 (61.13) | ||
| Above 40 | 22 (14.50) | 54 (16.93) | ||
| Resid. Status | 0.01 | Ns | ||
| Rural | 102 (69.39) | 223 (69.90) | ||
| Urban | 45 (30.61) | 96 (30.09) | ||
| Marital Status | 0.25 | Ns | ||
| Single | 41 (27.89) | 82 (25.71) | ||
| Married | 85 (57.82) | 190 (59.56) | ||
| Divor./Separated | 21 (14.29) | 47 (14.73) | ||
| Empl. Status | 3.20 | Ns | ||
| Employed | 61 (41.50) | 148 (46.39) | ||
| Unemployed | 56 (38.10) | 95 (29.78) | ||
| Prev. employed | 30 (20.40) | 76 (23.82) | ||
| Income, INR pm | 0.78 | Ns | ||
| 0 - < 10000 | 77 (52.38) | 165(51.72) | ||
| 10,000 - < 20,000 | 37(25.17) | 91 (28.52) | ||
| 20,000 -Above | 33 (22.45) | 63 (19.74) | ||
| Education | 3.06 | NS | ||
| Illiterate | 28 (19.05) | 45 (14.11) | ||
| Up to Matric. | 39 (26.53) | 79 (24.76) | ||
| Above Matric. | 80 (54.42) | 195(61.13) |
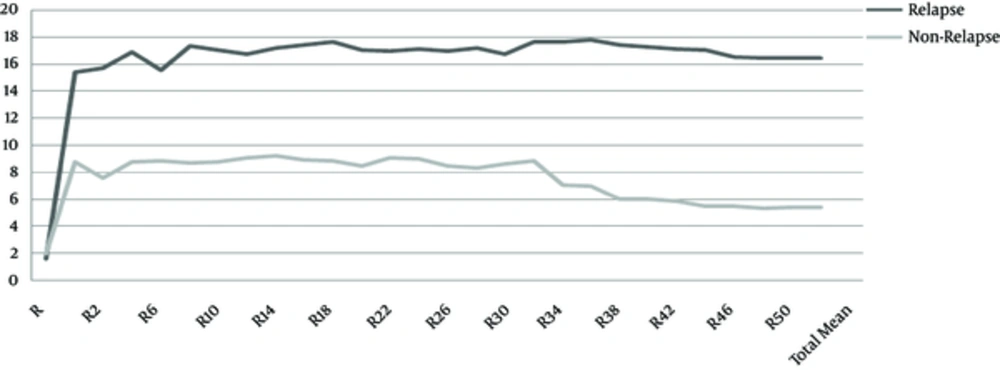
As depicted in graph I, none of the patients had depression at baseline as it was one of the exclusion criteria of this study. T value at baseline (t = 3.28 and p < 0.01), week 14 (t = 17.75 and P < 0.01), week 28 (t = 20.09 and P < 0.01), week 42 (t = 23.13 and P < 0.01), and week 52 (t = 22.42 and P < 0.01) were all significant.
In a comparison to relapsed and non-relapsed group, though both groups showed high mean depression score throughout 1-year follow up, the relapsed group had a much higher score, almost double that of the other group. It was also shown that mean depressive score was high in patients after inpatient detoxification, whether relapsed or not. After 30 weeks, mean depression score improved in non-relapsed patients but not in the relapsed group.
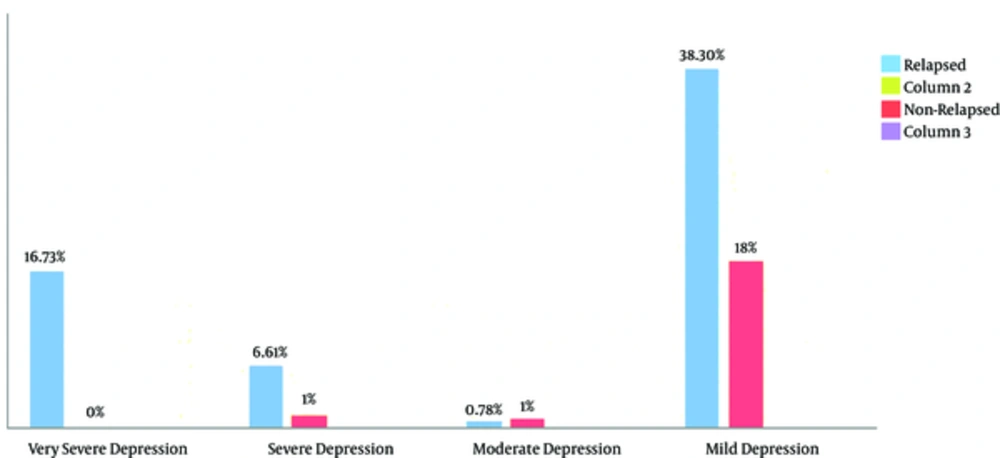
Graph 2 shows comparison of both groups with respect to depression intensity. Cut off for mild, moderate, severe, and very severe was taken as 8 to 13, 14 to 18, 19 to 22, and 23 and above, respectively. As indicated, more than 55% of relapsed patients had depression, with the majority having mild severity. Very severe depression was found in more than 16% of relapsed patients, which was absent in non-relapsed patients (Figures 1 and 2).
5. Discussion
The current study compared profiles of relapsed and non-relapsed patients after inpatient detoxification, and compared HAM-D scores during a 1-year follow up period. A high number of young males in both groups represented a pattern of drug abuse in the population, in general. The was no female admitted for detoxification in the current study, which might be due to high stigma associated with substance abuse; however, females have been reported at a significant number depending on city and geographical location, in other studies (11). Young age has been found to be associated with a high risk of relapse after inpatient detoxification (12, 13), yet the current study did not show any relationship between age and relapse. High rural percentage in the entire sample showed local area representation, as the tertiary care institute of this study was located in a rural area and mostly catered surrounding rural populations. The majority of patients in both groups were married and employed, which envisages the need to involve family members in the treatment process. However, low economic status of patients despite high cost of substances of abuse may suggest downward economic drift of substance abusers as well as alternate source of money being used for buying substances. Education does not appear to act as a deterrent factor for substance abuse or relapse prevention; however, economic literacy awareness might be more helpful. The current findings were similar to another study done at a tertiary center in India, to assess predictors for treatment retention, in which all subjects were males and the majority of the sample was married, educated up to matriculation, employed, belonged to a nuclear family and urban background. Higher socioeconomic status and having a family member with substance use was associated with higher chances of treatment retention (14).
Depression persisting after detoxification has also been reported earlier. Depression has mostly been reported to be part of withdrawal/protracted withdrawal or drug induced disorders, which alleviates gradually. Persistence of depressive symptoms beyond 6 months of abstinence is considered as a separate entity. In an 18-month follow up study of 279 different substance abusers, in which subjects were followed up at 6 monthly interval, abstinence of major depressive disorder was found to increase the risk of relapse to dependence by a factor of about 3 (9). In the current study the authors found that mean depression score in the relapsed group was twice that of the non-relapsed group. The current study also found persistent high mean depression scores after inpatient detoxification in both groups. This envisages the need for screening of all patients during follow up, which would help in decreasing relapse rate, thereby decreasing the financial burden on hospitals.
Assessing severity of depression would also be significant as it may be a significant risk factor for relapse. Mild depression was common in both groups, though more in the relapsed group. As compared to the non-relapsed groups, the relapsed group had a higher percentage (23.34%) of very severe and severe depression cases. This could be a significant reason for relapse. In another study, which investigated the ability of 4 hypnotically-induced mood states (euphoria, depression, anxiety, and anger) to trigger craving and other drug-related conditioned responses in detoxified opiate abuse patients, hypnotically induced depression was found to produce significant increases in drug craving for opiates. Depression also tended to increase global self-rating of opiate withdrawal (15). Being mindful of the severity of depression, it may be advantageous to start antidepressants as supported in a review of mood disorders and substance use disorders (6).
To conclude, regular screening for depression is needed during post detoxification follow up period as timely intervention may prevent relapse. Furthermore, counseling sessions during the maintenance phase may be focused accordingly so as to manage depressive symptoms also along with adherence therapy. Early start of antidepressants may also be helpful. More research is needed to further explore the relationship between depression and relapse.