1. Background
Addiction is a common problem in different nations and in 2010, there was 30,000 opioid-addicted pregnant mothers in Europe (1), and 2.3% of pregnant mothers in America were reported to be addicted (2). Cesarean section (C/S) is one of the most common operations in obstetric surgeries. Currently, spinal anesthesia is the method of choice due to lower adverse effects, faster development of relationship between the mother and the infant, and faster breastfeeding (3). Also, pain control improves breastfeeding mothers' satisfaction. Hence, many compounds are added to local anesthetics, with one of the most common being narcotic compounds. Among narcotics, fentanyl is used more due to its effect on C nerve fibers (4). In addicts, due to the decrease in the available receptors, the need for perioperative narcotic analgesic has increased (5-7).
In spinal anesthesia, lidocaine is used less due to the incidence of neurological complications, such as transient neurologic symptoms (TNS), and now the most common local anesthetic is bupivacaine, which is injected at 12 to 15 mg. High dose bupivacaine increases the level of anesthesia, hypotension, immobility duration, and patient discomfort from the lower limbs immobility and delayed walking. Hence, for reducing bupivacaine dosage and improving the quality of analgesia, opioids, especially fentanyl, are used to the extent of 10 to 25 µg. In many recent studies, the use of small amounts of local anesthetics with fentanyl is suggested (8-10).
In this study, lower dose of bupivacaine is used to reduce adverse effects and improve the patient’s movement, yet due to the greater need of opioid-addicted mothers for analgesic drugs, fentanyl at 50 µg is used.
2. Objectives
This study aimed to evaluate the quality and comparison of this method with high-dose bupivacaine and low-dose fentanyl in analgesia of opioid-addicted patients, considering Apgar score and movement time, incidence of nausea and vomiting, and hemodynamic changes during surgery.
3. Patients and Methods
After the confirmation of the research deputy of medical sciences University and local ethics committee and obtaining consent from the mothers, this study was performed on 62 opioid-addicted pregnant females with no comorbid disease (ASA I). The patients with cardiac, pulmonary, renal diseases and local anesthetics sensitivity, as well as the patients with contraindications to spinal anesthesia, and non-opioid addiction, were excluded.
For the patients, a 20-G catheter was embedded in brachial large vein, and then 150 to 200 mL of saline was injected. The patients were divided randomly with random numbers table and a sealed envelope to 2 equal groups. In the high-dose bupivacaine low-dose fentanyl (HBLF) group, 10 mg of 0.5% bupivacaine with 25 µg fentanyl (total 2.5 mL), and in the low-dose bupivacaine high-dose fentanyl (LBHF) group, 6 mg of 0.5% bupivacaine with 50 µg fentanyl and saline (total of 2.5 mL) were used. The compounds were numbered in 3-mL syringes and given to the anesthesiologists in 2.5 mL equal volumes. The anesthesiologist, who performed the spinal anesthesia and personnel, who evaluated the hemodynamic changes, adverse effects and other parameters, and the patients were not aware of the groups. The spinal anesthesia was performed in all the patients in a sitting position, L4-L5 space, and midline path with 25 gauge Quincke needle. After spinal fluid drainage, the prepared solution was injected. Then, the patients were located in supine position and when the block level reached T5, the operation was allowed. The sensory block was assessed by the pinprick test. After delivery, 1 mg of midazolam and oxytocin 20u were infused slowly.
The blood pressure and heart rate was measured before and after induction, and every 5 minutes up to 20 minutes. Nausea and vomiting were evaluated with 4 scores (0 = no nausea, 1 = mild nausea, 2 = severe nausea, and 3 = vomiting), as well as anti-vomiting drugs. For hypotension (systolic blood pressure < 80 mmHg or more than 30% decrease in blood pressure) 5 to of 10 mg ephedrine, and for vomiting or severe nausea, 0.5 mg of atropine with 4 mg of ondansetron was used after placenta delivery. The patient and surgeon’s satisfaction was measured with a Likert scale (0 to 10). The Apgar score was measured at 1 and 5 minutes. The level of spinal anesthesia was assessed after the surgery and every 5 minutes for the duration of sensory blockade to T12. The incisional pain score was evaluated with verbal analog scale (VAS = 0 - 10). The analgesic time was measured from the beginning of anesthesia until the incisional pain site required analgesic (VAS > 4), and then 5 mg of morphine was injected.
3.1. Statistical Studies
Considering the prevalence of hypotension as 75% in the study of Sivevski (11) and decreased amount of hypotension by 40% with 90% power and 0.05 alpha error factors with sigmaplot software, the number of patients was estimated as 61, with 31 patients allocated to each group. After data collection with the SPSS v16 software, the study results were analyzed. Quantitative data, such as age, weight, blood pressure, heart rate, anesthesia onset time, and duration of anesthesia, were evaluated by the student’s t-test and paired t-test statistical method. Qualitative data, such as Apgar score, nausea and vomiting, patient and surgeon satisfaction were also analyzed by the X2 test and Fisher’s exact test. P < 0.05 was meaningful.
4. Results
The demographic data, such as age, weight, previous births and cesareans, as well as pre-induction blood pressure, and heart rate are shown in Table 1. There was no significant difference between the groups regarding these parameters.
| Parameters | HBLF Group (n = 31) | LBHF Group (n = 31) | P Value |
|---|---|---|---|
| Age, y | 26.7 ± 7.1 | 30.3 ± 7.3 | 0.11 |
| Weight, kg | 78.4 ± 9.6 | 74.9 ± 10.2 | 0.24 |
| Previous births | 23 (74.2) | 22 (70.9) | 0.81 |
| Previous cesarean | 14 (45.2) | 11 (35.5) | 0.06 |
| Blood pressure, mmHg | 122.5 ± 11.9 | 131.6 ± 7.6 | 0.25 |
| Heart rate, beats/min | 97.4 ± 13.8 | 88.3 ± 10.4 | 0.33 |
aValues are expressed as Mean ± SD or No. (%).
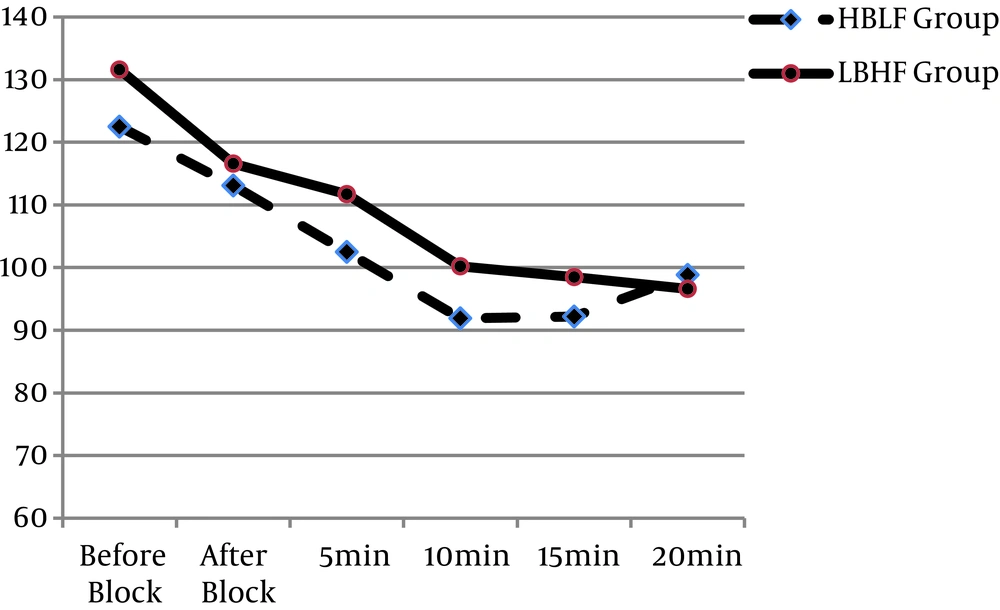
Hemodynamic changes: The systolic blood pressure of patients was measured after anesthesia, and then every 5 minutes up to 20 minutes. During this period, no significant difference was observed between the 2 groups (P value after anesthesia and at 5, 10, 15 and 20 minutes was 0.63, 0.31, 0.20, 0.28, and 0.42, respectively). In both groups, at the beginning of the study, the blood pressure reduction was significant (P = 0.019), while the difference was not significant (Figure 1).
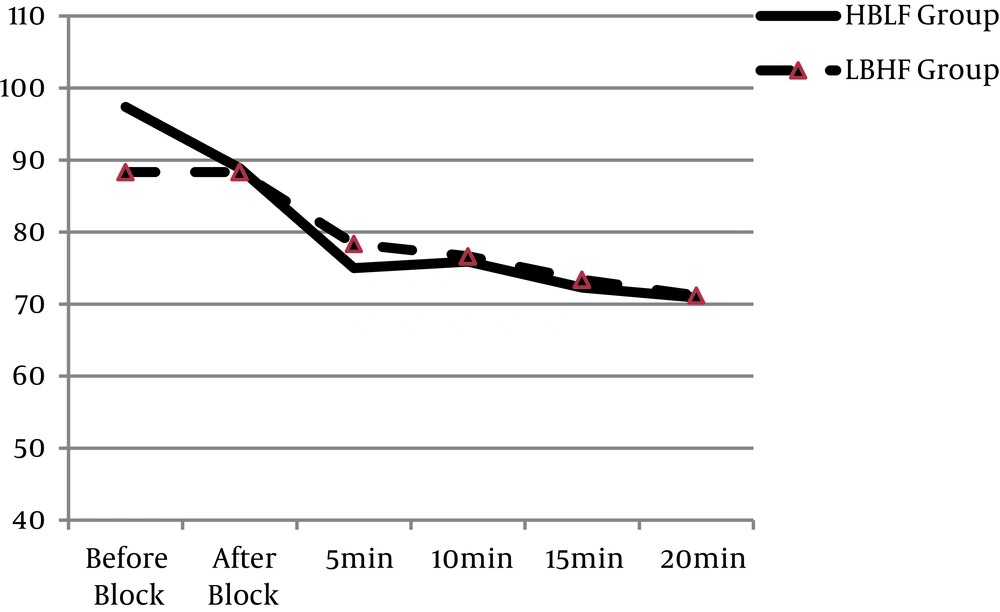
The heart rate of patients also showed a slight decrease during the study (Figure 2). There was no significant difference in heart rate changes between the 2 groups (P value after anesthesia at 5, 10, 15 and 20 minutes was 0.93, 0.15, 0.28, and 0.31, respectively). In the HBLF group, ephedrine was used in 7 patients (22.6%), and in the LBHF group, for 6 patients (19.3%), there was no statistical significant differences between the groups (P = 0.89).
Apgar score: The neonate Apgar score was measured at 1 and 5 minutes after delivery. In the HBLF group, the first minute Apgar was 6.76 ± 0.9, and in the LBHF group, it was 6.7 ± 1.2, and no statistical significant difference was observed between the 2 groups (P = 0.85). Also, the fifth minute-Apgar in the HBLF group was 8.67 ± 0.6, and in the LBHF group, it was 9.1 ± 0.6, yet no significant difference was found between the 2 groups (P = 0.86).
Adverse effects: In the HBLF group, 10 patients (32.3%) and in the LBHF group, 6 patients (19.3%) had nausea (P = 0.13) and only 1 patient in the HBLF group and 2 patients in the LBHF group had vomiting (P = 0.54), and no significant difference was observed between the groups. Sixteen patients (51.6%) in the HBLF group, and 17 patients (54.8%) in the LBHF group had pruritus, thus there was no significant difference between the 2 groups (P = 0.47).
Surgeon and patient satisfaction: During the surgery, level of satisfaction of the patient and surgeon was measured according to the Likert scale (0 - 10). The surgeon’s satisfaction in the HBLF group was 6.8 ± 1.5, and in the LBHF group, this was 6.8 ± 1.7, and no significant difference was observed between the groups regarding surgeon’s satisfaction (P = 0.92). The patient satisfaction was also evaluated during surgery. In the HBLF group, the level of satisfaction was 8.2 ± 1.5, and in the LBHF group, it was 7.4 ± 1.6, and no significant difference was observed (P = 0.09).
Onset time and duration of anesthesia and analgesia: The anesthesia onset time from the anesthetic injection to T5 block in the HBLF group was 4.42 ± 0.9 minutes, and in the LBHF group, this was 5.35 ± 0.9 minutes. There was a statistically significant difference between both groups (P = 0.002), and sensory block onset time to T5 in the LBHF group was longer. The sensory reversal of block to T12 in the HBLF group was 141.2 ± 28.9 minutes, and in the LBHF group, this was 122.3 ± 24.5 minutes, and a significant difference was observed between the groups (P = 0.03). Duration of anesthesia in the LBHF group was shorter. The time of patients’ request to inject the analgesic (VAS > 4) was compared between the 2 groups. In the HBLF group, this was 248.2 ± 31.4 minutes, and in the LBHF group, it was 282.1 ± 28.6 minutes. The LBHF group had a longer analgesia time, and demanded for analgesic with delay, and a statistical significant difference was observed (P = 0.02).
5. Discussion
In the opioid-addicted pregnant mothers, the need for analgesic was greater, hence, in order to control the pain in opioid-addicted patients, higher dose of the analgesic should be used in shorter intervals for longer periods. In 2012, in a study on pregnant and non-pregnant mothers on the need for narcotic and analgesic, a significant difference was observed regarding the need for narcotic and non-narcotic analgesic in the narcotic-dependent mothers (12). Due to hyperalgesia of opioid-addicted mothers, for improving pain control and decreasing the adverse effects of local anesthetics, in this study, bupivacaine consumption was decreased and 50 µg fentanyl was used.
In this study, no significant difference was observed between the patients regarding the hemodynamic effects, and hypotension in both groups was the same. Greater opioid dose had no effect on postoperative nausea and vomiting, pruritus, and also Apgar score at 1 and 5 minutes. In the HBLF group, with more bupivacaine and less fentanyl, the block onset time was faster, anesthesia duration was longer, yet analgesia duration and the time of first postoperative analgesia in the HBLF group was shorter than the LBHF group.
Numerous studies have compared high-dose and low-dose bupivacaine, yet 50 µg fentanyl was not used in any of the studies, and no study was performed on spinal anesthesia of opioid-addicted mothers, and in order to improve the hyperalgesia and reduce the local anesthetics adverse effects, and earlier movement, 6 mg bupivacaine was used with 50 µg fentanyl.
In Khezri’s study, there was a comparison between clonidine and intrathecal fentanyl and in comparison with 10 mg bupivacaine + clonidine, and bupivacaine + fentanyl, and bupivacaine + distilled water, the only clinical difference was increase in duration of analgesia in the clonidine group (13). In a study with 2 groups of 7.5 mg bupivacaine + 25 µg fentanyl and 5 mg bupivacaine + 25 µg fentanyl, the anesthesia onset time, duration, Apgar score, adverse effects, degree of motor block, ephedrine, and patient’s satisfaction were compared and the results in mothers and infants for anesthesia efficacy and side effects were the same (13).
In another study performed on 50 cesarean sections, 7.5 mg bupivacaine + 15 µg fentanyl and 7.5 mg levobupivacaine + 15 µg fentanyl were compared. The bupivacaine start time was faster, yet duration of anesthesia in levobupivacaine was longer (14). In a systematic research on 35 studies, bupivacaine with doses above and below 8 mg was evaluated. In the low-dose group, the need for analgesic was higher during surgery, yet the adverse effects, such as hypotension, nausea and vomiting was reported to be lower. In the low-dose group, only 2 patients needed general anesthesia and despite the benefits of low-dose bupivacaine, the quality of anesthesia and motor block had decreased. Another review study showed that low-dose of bupivacaine (5 to 7 mg) is a valuable method in maternal and fetal prognosis improvement, despite the lower quality of motor block (10).
In conclusion, in this study, the greater dose of narcotic in opioid-addicted pregnant mothers reduced the need for bupivacaine, and also had faster sensory reversal block and longer duration of analgesia. There was no difference between the adverse effects of 50 µg fentanyl and lower dose. In the group with lower dose of fentanyl and higher dose of bupivacaine, the anesthesia onset time was faster and sensory block was longer.