1. Background
The prevalence of HIV infection is reported to be around 66,000 in Iran. Since 2010, HIV incidence has increased by 21%, and AIDS mortality declined by 14% (1). Reduced mortality results in a possible increase in risky sexual behaviors and, therefore, higher transmission rates (2). Encouraging people to inform their sexual partners about HIV status is a way to reduce the spread of the diseases. According to the studies conducted in developing countries, the average disclosure rate of HIV infection to current or regular sexual partners is 49% (3). There are no official statistics about this issue in Iran, and previous studies reported that only 38% of people living with HIV (PLWH) are aware of their disease (4).
Disclosure of HIV status to sexual partner through increasing awareness and taking preventive measures, reduces the transmission probability of the diseases. It has two benefits; first, it reduces the number of sexual partners or sexual contacts with those at lower risk of infection. Second, it increases the prevalence of condom use (5). Factors such as condom use prevalence, Antiretroviral Treatment (ART) and Pre-exposure Prophylaxis (PreP) reduce the probability of HIV transmission and, therefore, with the aim of preventing HIV transmission are widely available to the public; Hence, awareness about HIV status of the partner is now of crucial importance (6).
Amoran et al. reported that 50.9% of PWLH informed their partner about their disease. The authors also reported that 44.6% of participants did not know their partner's HIV status (7). In another study, Przybyla et al. reported that 88% of PWLH informed their partner about their infection (8). Marks and Crepaz also reported that in 79.6% of cases using a condom was associated with disclosure of HIV status, while in 79.6%, it was not accompanied by disclosure of the HIV status (9). Kalateh Sadati et al. conducted a qualitative study, and the findings showed that PWLH were not inclined to disclose their status to the society (10).
Studies also show that nearly one-third of male PWLH that are sexually active do not disclose their HIV status to their sexual partners; unprotected sexual relationships include both vaginal and anal intercourses. Studies indicate that men who are engaged in unprotected sex acts are less committed to continue their treatment (i.e. ART or PreP) and are more likely to use drugs and/or alcohol (11). A study on PWLH in Haiti reported that 61% of patients did not disclose their disease, and people with multiple partners reported their HIV status to a lesser extent (12). Kalichman et al. found that 42% of participants did not disclose their HIV status to their partners during the past three months. In the current study, a close association between non-disclosure of HIV status to a sexual partner(s) and high-risk sexual behaviors was found (13). The results of a study conducted by Nachega et al. revealed that only 37% of participants disclosed their HIV status to their sexual partner(s) (14).
Latkin et al. highlighted the social network predictors of HIV status disclosure in Afro-American homosexual male PWLH and underscored the underlying role of factors other than communication skills, such as disclosure of HIV status, in reducing the risk of sexually transmitted diseases (STDs). The authors noted that HIV status disclosure is associated with characteristics of the social network that the person belongs to it, the recipients of disclosure, and individual's personal characteristics (15). Other studies mentioned to various associations between disclosure and mental health of the individuals depending on the purposes of disclosure and the quality of the relationship (16, 17). The study of Zea et al. on homosexual and bisexual Latin men showed that disclosure of HIV status was associated with increased social support, higher self-esteem, and lower levels of depression (18). While another study revealed that disclosure of HIV status was associated with increased depression among African-American and white women (19).
Disclosure of HIV status in addition to reducing the risk of disease transmission provides more opportunities to receive/provide social and spiritual support, improves access to treatment and medical care, increases opportunities for discussion and implementation of programs, reduces the probability of sexual transmission of HIV, and provides more opportunities for accurate and proper planning (3). Therefore, disclosing the status of HIV to sexual partners is a topic that should be considered to prevent and treat HIV. The current study aimed to determine predictors of disclosing HIV status to a sexual partner(s) in PWLH in Khuzestan province, Iran.
2. Objectives
This study was done to determine predictors of disclosure of HIV status to a sexual partner(s) in PWLH in Khuzestan province, Iran.
3. Patients and Methods
3.1. Study Type and Sampling Method
The current descriptive, analytical, cross-sectional study was performed on 89 men and 31 women with HIV/AIDS. Data were collected from October 2016 to February 2017. Participants were included in the study based on a positive serologic test, having a case file in the Behavioral Disease Counseling Center, and meeting the inclusion criteria.
Inclusion criteria were: being HIV-positive (based on the medical records available at the Behavioral Disease Counseling Center), being sexually active (based on patient reports, and the criterion was defined as having at least one vaginal, anal, or oral sex during the past six months), age over 18 years of old, ability to read and write, and willingness to participate in the study.
Questionnaires were completed by the participants in a completely private environment. To observe the confidentiality of information (mainly participants' names), a coding system was used in the questionnaires.
3.2. Data Collection Tools
A socio-demographic information form and an HIV status disclosure questionnaire, which was completed through self-report, were used to collect information.
The socio-demographic form included items on the age, gender, income level, level of education, race, marital status, occupation, factors related to disease (stage and time since onset of the disease) and behavioral factors (number of sexual partners, sexual behavior, number of unprotected vaginal, anal and oral sexual intercourses). In addition to demographic and clinical information, the participants were asked to report any high-risk sexual behaviors, history of other diseases or having sexually transmitted infections other than HIV, receiving or paying money for sex, history of intravenous drug use, history of drug, alcohol, methamphetamine, or cocaine abuse, number of sexual partners, HIV status of the partner (positive, negative, unknown or else), and specific to the men, history of homosexual activities.
The HIV status disclosure questionnaire developed by Kalichman was used to collect information regarding the HIV status and informing partners. To investigate its scientific validity (validity), first, the forward/backward translation method was used. Then, in order to obtain comments and information, changes were made. 10 items of the questionnaire were rated using a 4-points Likert scale (i.e., totally disagree, disagree, agree, and completely agree), that higher scores indicated more disclosure of HIV status (20).
All patients who had medical records in Ahvaz Behavioral Counseling Center were included in the study.
Data analysis was performed using SPSS version 24. Descriptive statistics, including frequency, percentage, mean, and standard deviation, were used to describe the socio-demographic, clinical, sexual behaviors, substance use, and overall HIV status disclosure scores. To determine the association between socio-demographic characteristics and the total score of HIV disclosure, bivariate tests (i.e. t-test and one-way analysis of variance (ANOVA)) were used. To control confounding factors, all variables with P < 0.05 were entered into the multivariate linear regression model with a backward strategy. All assumptions of multivariate linear regression, including normality, residuals, homogeneity of variance, collinearity of outliers, and independency of residuals, were examined.
4. Results
Out of 120 participants, 89 (74.2%) were male, and 31 (25.5%) were female. About half of the participants (50.8%) were aged 26 to 35 years old. More than one-third of the participants (35.8%) had elementary school education. 56 participants (46.7%) were married. Of 89 men who participated, nearly half (47.1%) of them were unemployed, and out of 31 women, nearly three-quarter (77.4%) were housewives.
About half of the participants (51.7%) reported zero income. Regarding the disease status, 50% of participants did not need drug treatment and were not in the active phase of the disease. Approximately one-third (35%) were receiving ART, and 11.7% did not take any medications, although they were in the active phase of the disease.
Regarding the history of HIV risks, less than half of the participants (45%) had a history of intravenous drug use (IDUs), 3.3% had a history of STDs, sex for money, and homosexual intercourse. About one-fourth of participants (26.7%) were women who were infected by their husbands (i.e. did not have risky behaviors); about one-fifth (19.4%) had more than one HIV risk factor.
About half of the participants (49.1%) had two sexual partners or more. Also, for 46.7 of the participants, the HIV status of sexual partners was unknown. The number of unprotected vaginal, anal, and oral sexual intercourses were 87.5%, 43.3%, and 58.5%, respectively. Also, 71.7% of the participants had a history of drug abuse, and 43.3% were current drug users. More than half of the participants (58.3%) had a history of imprisonment (Table 1).
| Variable | No. (%) | Variable | No. (%) |
|---|---|---|---|
| Age | History of high-risk HIV | ||
| < 25 | 10 (8.3) | Disease transmitted from other sex | 4 (3.3) |
| 26 - 35 | 61 (50.8) | Sex for money | 4 (3.3) |
| > 36 | 49 (40.8) | Male-male sex | 4 (3.3) |
| Sex | IDUs | 54 (45) | |
| Male | 89 (74.2) | None | 32 (26.7) |
| Female | 31 (25.8) | More than of the risks | 22 (19.4) |
| Marital Status | HIV status of sexual partner | ||
| Single | 54 (45) | HIV positive sexual partner | 32 (26.7) |
| Married | 56 (46.7) | HIV negative sexual partner | 25 (20.8) |
| Unmarried | 10 (8.3) | Sexual partner with unknown HIV status | 56 (46.7) |
| Job | Number of sexual partners | ||
| Unemployed | 42 (35) | 1 | 61 (50.8) |
| Other jobs | 13 (28.3) | 2 | 4 (3.3) |
| House keeper | 24 (20) | 3 or more | 55 (45.5) |
| Prostitute | 7 (5.8) | Unprotected vaginal intercourse | |
| Income | Yes | 105 (87.5) | |
| Income equal to expenditure | 19 (15.8) | Rectal unprotected sexual practice | |
| Income less than expenditure | 34 (28.3) | Yes | 52 (43.3) |
| Income more than expenditure | 5 (4.2) | Oral unprotected sexual practice | |
| No income | 62 (51.7) | Yes | 70 (58.3) |
| Education | Disease status | ||
| Primary School | 43 (35.8) | HIV positive | 64 (53.3) |
| Guidance School | 37 (30.8) | AIDS | 14 (11.7) |
| High School/Diploma | 30 (25) | Retroviral drugs intake | 42 (35) |
| Graduate | 10 (8.3) | History of drug use | |
| Diagnosis years | Yes | 86 (71.7) | |
| 1 year | 15 (12.5) | Current drug use | |
| 2 - 5 years | 66 (55) | Yes | 28 (43.3) |
| 6-10 years | 35 (29.2) | Prison Record | |
| more than 10 | 4 (3.3) | Yes | 28 (43.3) |
Socio-Demographic Characteristics in Men and Women with HIV/AIDS
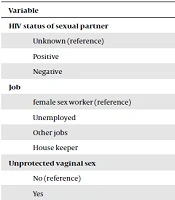
Based on Independent t-test and one-way ANOVA, there was a significant association between the total score of HIV disclosure and age, educational level, employment status, marital status, HIV status of sexual partners, number of sexual partners, unprotected vaginal sexual intercourse, unprotected anal sex, unprotected oral sex, HIV status, and current drug consumption. These variables were entered into the multivariate linear regression model with a backward strategy. The variables of age, educational level, marital status, unprotected oral sex, and HIV status were excluded. Employment status, HIV status of sexual partner, unprotected vaginal sex, unprotected anal sex, and recurrent consumption of narcotic drugs were predictors of HIV disclosure and explained 58.7% of the variance in the total score of HIV disclosure (Table 2).
| Variable | B | (95% Confidence Interval) | P Value |
|---|---|---|---|
| HIV status of sexual partner | |||
| Unknown (reference) | 0 | ||
| Positive | -4.1 | -9.1 to 0.8 | 0.099 |
| Negative | 6.4 | 1.8 to 10.9 | 0.006 |
| Job | |||
| female sex worker (reference) | 0 | ||
| Unemployed | 4.9 | -2.9 to 12.7 | 0.213 |
| Other jobs | 7.2 | -0.8 to 15.3 | 0.079 |
| House keeper | 3.6 | -5.9 to 13.0 | 0.454 |
| Unprotected vaginal sex | |||
| No (reference) | 0 | ||
| Yes | -9.0 | -14.5 to -3.5 | 0.002 |
| Unprotected anal sex | |||
| No (reference) | 0 | ||
| Yes | -4.5 | -8.3 to -0.7 | 0.021 |
| Recurrent use of drug | |||
| No (reference) | 0 | ||
| Yes | -13.9 | -18.4 to -9.4 | < 0.001 |
Personal-Social Predictors of HIV Infection disclosure in Men and Women with HIV/AIDS Based on Multivariate Linear Regression Model
5. Discussion
The current study aimed to investigate the disclosure of HIV and its individual and social determinants in PWLH in Khuzestan province. The literature review showed that the current study is one of the few on individual and social predictive factors of HIV disclosure in Iran. Based on the results, the mean (SD) scores of HIV disclosure in men and women were 12.7 ± 3.8 and 11.2 ± 4.1 out of 20. There was a significant positive correlation between disclosure of HIV infection with employment status, HIV status of sexual partner, number of unprotected vaginal sex acts, unprotected anal sex acts and recurrent consumption of narcotic drugs.
In the current study, employment status was one of the variables that had effects on HIV disclosure. The rate of HIV disclosure in employed people was higher than unemployed and female sex workers. A study conducted by Bidaki et al. showed that employed PWLH feel more social acceptance than others (21), it can explain why they disclosed the disease.
In the present study, the HIV status of sexual partners was one of the variables that influenced the disclosure of HIV infection and, if their partner was HIV negative, the disclosure rate was higher. Tang et al. showed that disclosure of HIV status was higher in people who received such disclosure from their partner (22).
Unprotected vaginal and anal sexual intercourses also influence the disclosure of HIV. Based on the results, the score for safe sexual behaviors was lower in those who had unprotected sex. Many studies have highlighted the association between decreased unsafe and high-risk sexual behaviors and disclosure of HIV infection (23-26). The results of the mentioned studies are consistent with the findings of the current study.
In this study, recurrent consumption of narcotic drugs was one of the variables that influenced the disclosure of HIV. The rate of exposure to HIV in drug and alcohol users was lower than those who did not use drugs or alcohol. Wei et al. showed that there is a strong positive association between non-disclosure of HIV infection before sex and drug abuse (27). Although in many epidemic regions, HIV prevalence is high among IDUs, but few studies are conducted on the HIV disclosure rate among them (3).
Like other research, the current study also had limitations. First, the participants were clients of a behavioral disease counseling center, so generalization of the results to all PWLH should be with caution, particularly those who are not seeking care or medication. In addition, HIV-related data were obtained through self-report. Thus, some factors may not have been truly reported due to social orientations. Future studies are recommended on more diverse and larger populations of women. Also, interventional studies can be performed based on the findings of the current study.
5.1. Conclusions
More research is needed to identify the factors associated with disclosure of HIV status in Iran. The present study highlighted the need for behavioral interventions, such as providing support and counseling with sexual partners of HIV patients about HIV preventive behaviors, such as condom use, reducing the number of sexual partners, and creation of a positive attitude towards the lives of HIV-positive IDUs to overcome the barriers to reduce high-risk behaviors and drug abuse, through behavioral disease counseling centers.