1. Background
Worldwide human papillomavirus (HPV) is known as the most frequent sexually transmitted viral infection. HPV is a highly contagious disease with a high level of relapse, increasing the chance of genital cancers, medical costs, loss of productivity, and increased psychosocial outcomes (1, 2). Early-onset sexual activity, multiple sexual partners, and unsafe sex are important risk factors for genital warts (3). Two studies showed tobacco use and a greater number of lifetime sexual partners were associated with higher HPV infection prevalence (4, 5).
High-risk behavior affecting anogenital warts (AGW) prevalence varies among different geographic, ethnic, racial, and cultural populations (6). A study reported that the HPV prevalence was relatively high (54.8%) in Tehran (7).
The HPV is identified as the principal reason for cervical cancer, penile cancer, anal and oropharyngeal cancer, which is seen in people practicing anal and oral sex (8). Knowledge about the risk factors and preventive strategy is low that results in serious health problems (3, 6, 9, 10).
2. Objectives
We investigated risk factors and knowledge about STIs among men with AGW.
3. Patients and Methods
The men who referred to a dermatology clinic affiliated to Shiraz University of Medical Sciences to treat AGW from June 2015 to Feb 2016 in Shiraz were enrolled. The data collection form was consists of age, marital and educational status, age of the first sexual intercourse, alcohol consumption, cigarette smoking, and pattern of sexual behavior and STIs knowledge.
Informed consent was taken from each patient after explaining the objectives of the study, and their information was recorded anonymously. Our study was approved by the local Ethics Committee of Shiraz University of Medical Sciences (Ethics code: ec-p-9378-7568).
4. Results and Discussion
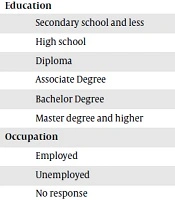
A total of 224 men diagnosed with genital warts by health care providers were enrolled. The mean age was 28.84 ± 8 years (range 16 - 57). Nearly half of the men were single 110 (49.1%), and 103 (48.4%) were highly educated, and the majority of the participants were employed 144 (64.3%). The onset of sexual relationships was 20.31 ± 3.71 years (rang 7 - 30). Among the married ones (95 men), 58 (61.05%) of them reported having extramarital sexual relationships. The median number of sex partners was 2.8.
A total of 125 (55.8%) had girlfriends, and 41 (31.5%) of them had 2 sex partners in the past six months. Moreover, 132 (58.9%) of them had the experience of anal sex in their lifetime, and only 15 (7.1%) of the participants used condoms regularly.
The history of smoking cigarettes, pipe or water pipe, and drinking alcohol was reported in 194 (87.1%), and 144 (64.3%) of our participants, respectively. Unprotected sex after opioid, use of stimulants, and consumption of alcohol occurred among 10 (4.5%), 11 (4.9%), and 57 (25.6%) participants, respectively (Table 1).
| Variables | No. | % |
|---|---|---|
| Mean age ± SD (years) | 28.84 ± 8 | |
| Age (years) | ||
| ≤ 20 | 33 | 14.7 |
| 21 to 30 | 122 | 54.5 |
| 31 to 40 | 54 | 24.1 |
| ≥ 40 | 15 | 6.7 |
| Marital status | ||
| Single | 110 | 49.1 |
| Married | 95 | 42.5 |
| Other | 19 | 8.4 |
| Educationa | ||
| Secondary school and less | 10 | 0.5 |
| High school | 43 | 20.2 |
| Diploma | 57 | 26.8 |
| Associate Degree | 29 | 13.6 |
| Bachelor Degree | 53 | 24.9 |
| Master degree and higher | 21 | 9.9 |
| Occupationb | ||
| Employed | 144 | 64.3 |
| Unemployed | 60 | 26.8 |
| No response | 19 | 8.5 |
| Type of sex partner (lifetime)c | ||
| Permanent wife | 90 | 40.2 |
| Temporary wife | 15 | 6.7 |
| Sex worker | 58 | 25.9 |
| Girlfriend | 125 | 55.8 |
| Homosexual | 2 | 0.9 |
| Number of sex partners in the past six monthsd | ||
| 1 | 32 | 24.6 |
| 2 | 41 | 31.5 |
| 3 | 33 | 25.4 |
| 4 | 14 | 10.8 |
| ≥ 5 | 10 | 7.6 |
| Type of sex (lifetime) | ||
| Vaginal | 174 | 77.7 |
| Oral | 52 | 23.2 |
| Anal (incentive) | 125 | 55.8 |
| Anal (receptive) | 7 | 3.1 |
| Condom used | ||
| Always | 15 | 7.1 |
| Often | 26 | 12.4 |
| Sometimes | 62 | 29.5 |
| Rarely | 60 | 28.6 |
| Never | 47 | 22.4 |
| Unprotected sex after opioid usage | 10 | 4.5 |
| Unprotected sex after stimulant usage | 11 | 4.9 |
| Unprotected sex after consumption of alcohol | 57 | 25.6 |
aNA (4.1%)
bNA (0.4 %)
cEverybody may have more than one type of sex partner
dNA (0.1 %)
4.1. STI Knowledge
More than half of the men (n = 146, 66.4%) were not aware of STI symptoms. The mean knowledge score regarding STI symptoms was 1.7 ± 1.31 (out of 8). The mean knowledge score of our participants regarding the transmission route of STI was 2.26 ± 1.37 (out of 9). The mean knowledge score regarding STI prevention was 1.04 ± 1.95 (out of 8). The total knowledge score regarding transmission routes, prevention, and STI symptoms was 6.25 ± 3.36 (out of 25).
There was no significant difference between knowledge of single (6.3 ± 3.01) and married participants (6.2 ± 3.69) (P value = 0.893) about STIs. There was no significant difference in knowledge scores regarding different levels of education (P value = 0.418).
Anogenital warts are one of the most common infections among adolescents and young adults (11). This study represents general information and risk factors in men with genital warts in Shiraz, Iran. Those infected were largely young; almost half of them were single and had a high level of education. Similarly, young adults have been reported as the highest vulnerable group (11, 12).
In our study, the onset of sexual activity was similar to Tehran (6). The onset of sexual activity differs in various cultures and religions; hence, health education, especially about STI prevention, should be initiated at high school when this vulnerable group is easily accessible.
There were no differences in awareness about STI between married and single participants. Also, no association was observed among condom use, sex type, and STI knowledge in our study. On the other hand, another study showed that HPV awareness was higher among highly educated and married participants (11).
Result of different studies showed that most of the participants had high education and unsafe sex, but did not use a condom (1, 6, 13, 14). These results are consistent with our findings.
Our study could provide baseline data for an interventional study. The presence of information bias is probable due to self-report. Lack of a control group was our limitation.
HPV is a public health challenge that involves young adults. To combat this problem, primary prevention by abstaining from multiple sex partners and condom usage are the best option. Managing the affected patients should be considered secondary prevention by finding and treating symptomatic and asymptomatic individuals in STI clinics. Most of the infected population are young people; hence, the psychological and economic burden of HPV infection should be considered.