1. Background
Methamphetamines are the most prevalent synthetic stimulants worldwide (1). Abuse of these neuro stimulants is associated with various physical and psychiatric problems such as mood disorders, psychosis (2, 3), cognitive impairment (4, 5), sexual dysfunction, and violent behavior (6).
Amongst adverse effects of methamphetamine abuse, methamphetamine associated psychotic symptoms due to the excessive release of dopamine (7) can have an impact on the quality of life and health conditions, which may lead to a heavy burden on individuals and society (8, 9).
The different studies have reported various rates of psychotic symptoms among methamphetamine abusers in a wide range between 13% to 60% (10, 11).
The high rate of psychosis in methamphetamine abusers motivates the researchers and practitioners to investigate the associated factors of methamphetamine-induced psychotic symptoms to reduce the risk of psychosis among these abusers. Based on the evidence, it seems that different factors such as chronic dependence on methamphetamine (12), the severity of dependence (13), lower onset age (14) and dose of the agent (15) are the risk factors that increase the probability of methamphetamine associated psychotic symptoms in abusers.
Despite the mentioned associated factors, there is some evidence that suggests contrasting findings. For example, some cases with long dependence and frequent abuse of methamphetamines do not show any psychotic symptoms, while some with limited abuse of methamphetamine experience long-lasting psychosis (16, 17). These controversies indicate the necessity to conduct more studies in different countries.
2. Objectives
Regarding the high prevalence rate of amphetamine abuse in Iran especially among youth population and distinguishing the risk factors of methamphetamine associated psychosis while reducing harmful consequences (18, 19), we aimed to investigate the relationship between the rate and severity of methamphetamine associated psychotic symptoms with duration and dose of methamphetamine in Iranian abusers.
3. Patients and Methods
The statistical population of this descriptive-correlational study consisted of all methamphetamine abusers who referred to Ibn-e-Sina Psychiatric Hospital in Mashhad city (the second most populous city of Iran). The cases were selected through convenience sampling method.
Inclusion criteria: (1) abusers aged 18 - 45 years who referred to Ibn-e-Sina Psychiatric Hospital in Mashhad city (hospitalized or out-patient) with positive amphetamine test; (2) presence of psychosis on admission; (3) receiving a diagnosis of amphetamine-induced psychosis based on DSM-IV criteria; (4) written consent form to participate in research (by patient or parents).
Exclusion criteria: presence of comorbidity, history of psychotic disorders before amphetamine abuse.
3.1. Research Instrument
3.1.1. Demographic Form
This form included demographic variables such as age, gender, marital status, occupational status, history of physical illness, history of psychiatric hospitalization.
3.1.2. Positive and Negative Symptoms Scale
This is a 30-question scale that responded in a 5-degree Likert system. It has 5 subscales included: negative symptoms (8 questions), disassociation (7 questions), positive symptoms (6 questions), arousal (4 questions), anxiety, and depression (5 questions). This scale has good validity (Cronbach alpha = 0.77), and it is normalized for the Iranian population (20, 21).
3.2. Ethical Approval
This research is approved by the vice-chancellor of Islamic Azad University, the branch of Shahrood concerning ethical considerations, the aim of the research was explained for parents of patients or patients who referred to Ibn-e-Sina Hospital, and the cases have participated voluntarily.
3.3. Statistical Analysis
Data were analyzed by descriptive statistics such as mean, standard deviation and mode, etc. and Pearson correlation coefficient through SPSS software.
4. Results
The participants included 100 amphetamine abusers (80 men and 20 women) with the mean age of 30.84 ± 6.62 years. Demographic characteristics of participants indicated that 43% of participants were married while 37% and 20% of them were single and divorced, respectively. In terms of educational level, 15% of them were educated at the elementary level, 37 of them had intermediate level while 40% and 8% of participants had a diploma and higher-level, respectively. Also, 70% of amphetamine abusers were jobless. Also, 13% of them had a history of admission in a psychiatric hospital, and 1% had a positive family history of psychiatric disorder.
Table 1 shows the descriptive variables related to psychopathology, psychotic symptoms, and amphetamine abuse.
| Variable | Mean | Standard Deviation | Maximum | Minimum |
|---|---|---|---|---|
| Severity of positive symptoms | 22.70 | 6.48 | 37 | 11 |
| Severity of negative symptoms | 18.47 | 5.73 | 37 | 8 |
| General psychopathology | 39.37 | 8.74 | 70 | 19 |
| Duration of amphetamine abuse (month) | 20.55 | 12.56 | 60 | 2 |
| Dose of amphetamine abuse (score 1 - 4)a | 1.86 | 0.93 | 4 | 1 |
a1, < 0.25 gram; 2, 0.25 - 0.50 gram; 3, 0.50 - 1.0 gram; 4, > 1.0 gram.
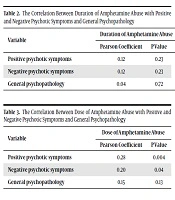
Tables 2 and 3 present the correlation between duration and dose of amphetamine abuse with positive and negative psychotic symptoms and general psychopathology.
| Variable | Duration of Amphetamine Abuse | |
|---|---|---|
| Pearson Coefficient | P Value | |
| Positive psychotic symptoms | 0.12 | 0.23 |
| Negative psychotic symptoms | 0.12 | 0.23 |
| General psychopathology | 0.04 | 0.72 |
| Variable | Dose of Amphetamine Abuse | |
|---|---|---|
| Pearson Coefficient | P Value | |
| Positive psychotic symptoms | 0.28 | 0.004 |
| Negative psychotic symptoms | 0.20 | 0.04 |
| General psychopathology | 0.15 | 0.13 |
As seen in the above tables, there were significant relationships between dose of amphetamine abuse and positive (P = 0.004) and negative psychotic symptoms (P = 0.04) while the duration of amphetamine abuse did not have any significant relationships with positive and negative psychotic symptoms and general psychopathology (P > 0.05).
5. Discussion
Based on the present study which was conducted on 100 amphetamine abusers, there were no significant relationships between duration of amphetamine abuse and positive and negative symptoms and general psychopathology despite the long duration of abuse among almost of patients (longer than 20 months). This is while the findings indicated that the dose of amphetamine had a stronger correlation with psychotic symptoms.
Similar to the present study, Ma et al. in China evaluated the risk of psychiatric symptoms in 1277 methamphetamine abusers (1069 men and 160 women) through positive and negative symptoms scale, Hamilton anxiety inventory, and Beck depression inventory. In terms of duration of amphetamine abuse, the cases were divided into three groups: < 1 year, 1 - 5 years, and five years. The findings showed that the prevalence of psychotic symptoms in 3 durations of MA abuse was 16.5%, 17.2%, and 23.5% respectively. Like our study though, the rate of any type of psychiatric symptoms increased significantly with longer duration of abuse (12).
In addition, Su et al. assessed the demographic variables and risk factors of methamphetamine-induced psychosis (MAP) in 1685 abusers. Most of them are men aged 30 years or above with limited education. Furthermore, 72.3% of them had an abuse duration of more than 3 months. In terms of dose, 47.8% of them used ≥ 0.2 gram MA per occasion, and 17% of abusers experienced psychotic symptoms even in abstinence period. The results showed that higher dose of MA (≥ 0.2 gram) and longer duration (> 3 months) were associated with MAP. These findings support the present study (22).
There was an inconsistency between the conducted studies about years of abuse and methamphetamine associated psychosis (MAP). Almost of studies reported that there was not a significant association between duration of abuse and MAP, although some of the studies found that duration of abuse longer than 4 years significantly increases the rate of MAP (23).
On the other hand, it seems that the amount of amphetamine abuse is associated with MAP and psychiatric symptoms greater than the duration of abuse, similar to our research (13, 24).
McKetin et al. in their research which was published in 2013 assessed 276 participants aged 16 years or older (mean age: 31.7 years) who received the diagnosis of methamphetamine dependency through Brief Psychiatric Rating Scale to evaluate hallucinations, suspiciousness and unusual thought content and Opiate Treatment Index to assess the amount methamphetamine abuse in the past month. The majority of these participants were male, jobless, and single, as in our research. The findings showed that experiencing psychotic episodes was associated with a higher dose of amphetamine abuse (> 16 days of abuse in the past month) strongly similar to our research; although the weight of the methamphetamine was not measured in the McKetin et al. study (15).
Another study conducted by Salo et al. on 190 methamphetamine abusers indicated that there was not any significant relationship between MA-induced paranoia and demographic variables of methamphetamine abuse including duration, age of first abuse, and mean daily dose of MA (17).
Regarding to the high prevalence rate of methamphetamine-induced psychosis, violent behaviors and suicidality in methamphetamine abusers, assessment to identify risk-factors among these patients is necessary (25-27).
5.1. Limitations
Our research has some limitations as any cross-sectional studies such as:
- Small sample size.
- Participants who referred to one center.
- Lack of long term follow-ups.
5.2. Conclusions
Based on the findings, there were significant relationships between dose of amphetamine abuse and positive and negative psychotic symptoms, while the duration of amphetamine abuse did not have any significant relationships with positive and negative psychotic symptoms and general psychopathology. This finding emphasizes the psychiatric evaluation of heavy abusers.