1. Background
Brucellosis (Malta fever) is a zoonotic infectious disease caused by Brucella species, which are aerobic, Gram-negative, non-motile, and facultative intracellular coccobacilli responsible for the disease in a broad spectrum of mammalians. Brucella abortus and Brucella melitensis are the two common human pathogens in Iran (1, 2).
Brucellosis is a major concern in domestic and wild animals. It is transmitted to human through close contact with livestock, and ingestion of raw meat, milk, and other non-pasteurized dairy products. Therefore, brucellosis is considered an occupational disease, especially among laboratory workers, veterinarians, slaughterhouse workers, ranchers, and farmers. Other transmission routes include inhalation, conjunctiva, and skin cuts. Brucellosis is rarely spread from human to human (3).
Brucellosis is still one the most challenging health issues in the developing countries, including Iran. Brucellosis is difficult to control in animals because despite being the most common zoonotic disease, it is often neglected by scientists for practical reasons (4). Moreover, the wide range of clinical manifestations result in difficulty in definitive diagnosis because they overlap with symptoms of other diseases. Proper diagnosis is one of the main problems in the treatment of brucellosis (5).
Brucellosis has a high prevalence in developing countries, and due to the lack of proper surveillance and control programs, there has recently been an increase in brucellosis incidence rate (6). Considering its complicated nature, brucellosis is regarded as a grave threat to public health. The disease is known to cause abortion in cows during the three last months of pregnancy and subsequently decrease milk production (7). Fever, lethargy, and arthritis are important symptoms of brucellosis contamination in humans (8).
According to the World Health Organization (WHO) report, the estimation of total worldwide brucellosis cases is around 500,000 annually, while this value is one-fifth of all cases. Due to the consumption of raw milk and cattle-related occupations, brucellosis is prevalent in the east Mediterranean countries, South America, and possibly Sub-Saharan Africa (9, 10). Brucellosis is an endemic disease in Iran, and review of the literature indicates that numerous studies have been conducted on the epidemiology of brucellosis in Iran.
Salmas is the capital of Salmas County, West Azerbaijan Province, Iran. It is located near the eastern border of Turkey. It coordinates are 38°11’41”N 44°45’53”E at a 90-km distance from Urmia (capital of the province) in south, 45 km from Khoy in north, and 55 and 90 km from Tasouj and Shabestar, respectively, in east. According to the 2016 census conducted by the Statistics Center of Iran, the city’s population is 196,546, of which 101,440 people are settled in urban areas, and 95,406 people are settled in rural areas.
2. Objectives
Considering the high prevalence of brucellosis in northwest of Iran and the occupational nature of the disease, this study aims to investigate brucellosis epidemiology in Salmas where most people are stockbreeders.
3. Methods
This cross-sectional study was carried out using the personal health records of all patients visiting governmental and private clinics and laboratories in Salmas over a four-year period (2014 - 2017). A checklist was designed to collect data from the health surveillance system of Urmia University of Medical Sciences regarding age, sex, place of residence (urban/rural), occupation, date of diagnosis, history of animal contact, history of consuming unpasteurized dairy products, clinical signs and symptoms of disease, and results of diagnostic laboratory tests. According to national guidelines (Iranian Center for Disease Control [ICDC], 2012), the inclusion criteria in this study were both clinical signs and symptoms. Brucella cases were defined by demonstrating a Wright titer of 1/160, a Coombs titer of 1/320, and a 2-mercaptoethanol (2-ME) titer of 1/80 for patients with clinical signs and symptoms compatible with brucellosis. Data analysis was carried out by the SPSS version 19, using the chi-square test, t-test, and the Cochran-Armitage χ2 test for trend at a significance level of P < 0.05.
4. Results
Totally, 417 cases were identified with human brucellosis including 243 (58.27%) male and 174 (41.73%) female patients. The male to female ratio was 1.38, which is explained by the higher involvement of men in livestock handling. In this study, patients were aged from less than a year to over 60 and were classified into six age groups. The highest prevalence of brucellosis was detected among the age group of 31 - 45 years (33.74% male, 30.45% female), while patients aged 1 - 6 years (4.52% male, 2.29% female) showed the least prevalence. Among males, the oldest patient was 88 years old, and among females, the oldest patient was aged 87 years (Table 1). The mean age of cases was 34.8 ± 1.06 years in men and 39.29 ± 1.23 years in women (P < 0.001).
| Age Group, y | Male, No. (%) | Female, No. (%) | Overall | Male:Female Ratio |
|---|---|---|---|---|
| 1 - 6 | 11 (4.52) | 4 (2.29) | 15 | 2.75 |
| 7 - 15 | 21 (8.64) | 4 (2.29) | 25 | 5.25 |
| 16 - 30 | 65 (26.75) | 46 (26.45) | 111 | 1.41 |
| 31 - 45 | 82 (33.74) | 53 (30.45) | 135 | 1.54 |
| 46 - 60 | 47 (19.35) | 51 (29.33) | 98 | 0.92 |
| 60+ | 17 (7) | 16 (9.19) | 33 | 1.06 |
| Total | 243 (100) | 174 (100) | 417 | 12.93 |
The incidence rate of brucellosis was 52.73 cases/100,000 inhabitants over the four-year study in Salmas, with the highest incidence rate of 64/100,000 in 2017 (Table 2) (P < 0.01). In the same year, out of 123 patients, 66 (53.65) cases were male, and 57 (46.35) cases were female. Furthermore, 102 (82.93%) patients were from rural regions, and 21 (17.07%) patients were from urban areas. Out of the 70 cases of brucellosis in 2016, there were 41 (58.57%) male patients and 29 (41.43%) female patients. Moreover, 4 (5.71%) patients were from urban areas, and 66 (94.29%) patients were from rural regions (Table 2).
| Date of Admission | Total Cases | Total Population | Male | Female | Urban | Rural | Urban Population | Rural Population | Incidence Rate (Cases/100,000), % |
|---|---|---|---|---|---|---|---|---|---|
| 2014 | 110 | 203758 | 74 (67.27) | 36 (32.73) | 13 (11.82) | 97 (88.18) | 99929 | 103829 | 54 |
| 2015 | 114 | 198657 | 62 (54.38) | 52 (45.62) | 4 (3.5) | 110 (96.5) | 104911 | 93746 | 57.3 |
| 2016 | 70 | 196546 | 41 (58.57) | 29 (41.43) | 4 (5.71) | 66 (94.29) | 101440 | 95106 | 35.6 |
| 2017 | 123 | 191921 | 66 (53.65) | 57 (46.35) | 21 (17.07) | 102 (93) | 99544 | 92377 | 64 |
aValues are expressed as No. (%).
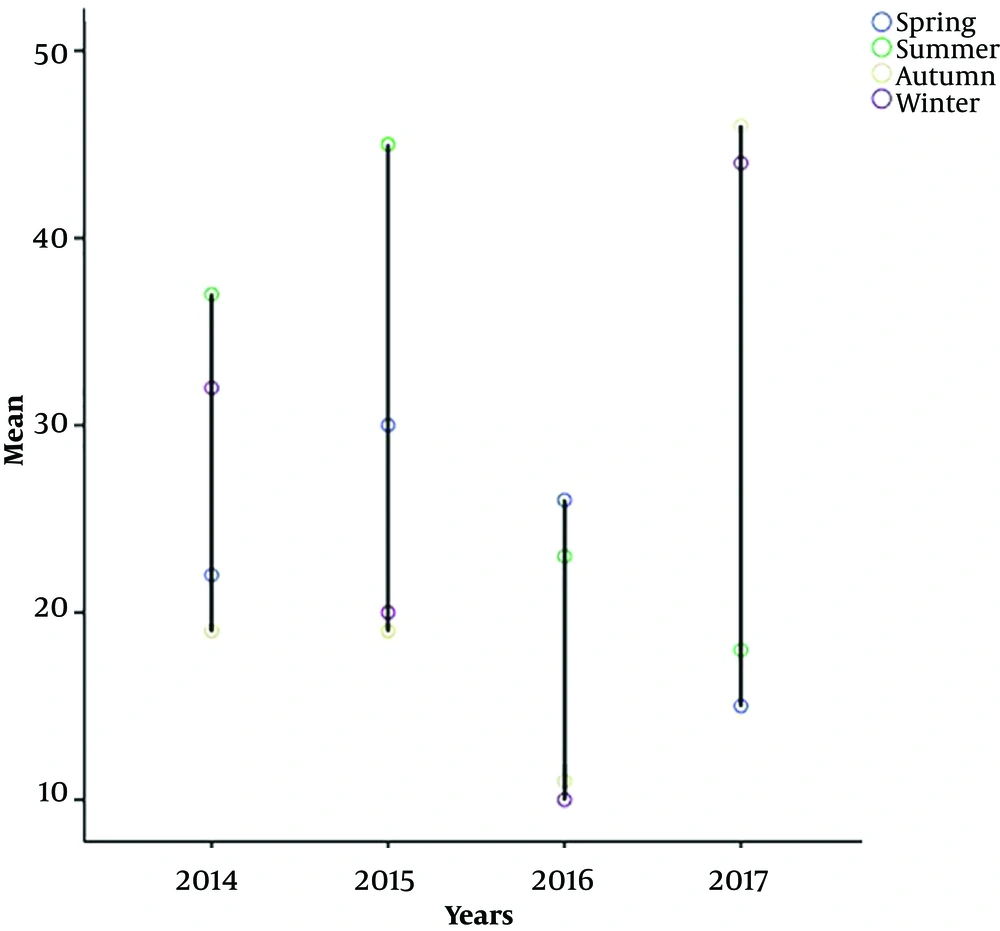
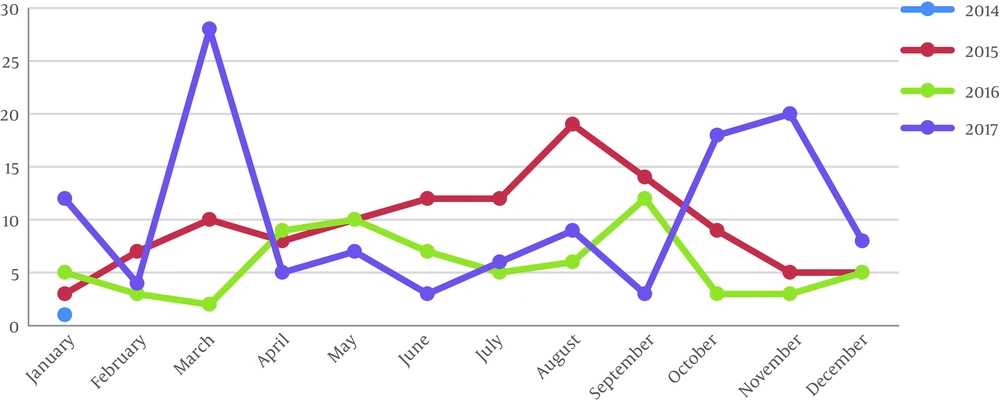
The highest prevalence was observed in summer with 123 (29.49%) cases, and the lowest prevalence was reported during spring with 93 (22.30%) cases (Figures 1 and 2). In March, brucellosis showed the highest incidence of 55 (13.18%) cases, while the lowest incidence was recorded in June with 22 (5.27%) cases. In the first half of the year, the prevalence of the disease was higher than the second half, such that 49.89% of cases were observed in the first six months (Tables 3 and 4).
| Year | Spring | Summer | Autumn | Winter | Total |
|---|---|---|---|---|---|
| Frequency | No. | % | No. | % | No. |
| 2014 | 22 | 20.00 | 37 | 33.64 | 19 |
| 2015 | 30 | 26.32 | 45 | 39.47 | 19 |
| 2016 | 26 | 37.15 | 23 | 32.85 | 11 |
| 2017 | 15 | 12.20 | 18 | 14.63 | 46 |
| Month | Year | |||
|---|---|---|---|---|
| 2014, No. (%) | 2015, No. (%) | 2016, No. (%) | 2017, No. (%) | |
| January | 7 (6.33) | 3 (2.63) | 5 (7.14) | 12 (9.75) |
| February | 10 (9.14) | 7 (6.14) | 3 (4.28) | 4 (3.25) |
| March | 15 (13.63) | 10 (8.77) | 2 (2.85) | 28 (22.76) |
| April | 4 (3.53) | 8 (7.01) | 9 (12.85) | 5 (4.06) |
| May | 10 (9.14) | 10 (8.77) | 10 (14.30) | 7 (5.69) |
| June | 8 (7.37) | 12 (10.52) | 7 (10.00) | 3 (2.44) |
| July | 10 (9.14) | 12 (10.52) | 5 (7.14) | 6 (4.88) |
| August | 14 (12.65) | 19 (16.70) | 6 (8.57) | 9 (7.32) |
| September | 13 (11.81) | 14 (12.28) | 12 (17.17) | 3 (2.44) |
| October | 9 (8.18) | 9 (7.90) | 3 (4.28) | 18 (14.65) |
| November | 3 (2.72) | 5 (4.38) | 3 (4.28) | 20 (16.26) |
| December | 7 (6.36) | 5 (4.38) | 5 (7.14) | 8 (6.50) |
| Total | 110 (100) | 114 (100) | 70 (100) | 123 (100) |
The most common occupations involved in brucellosis are rural occupations. Women working as housewives-stockbreeders with 116 (27.81%) cases, and men working as stockbreeder-farmers with 110 (26.37%) cases exhibited the highest prevalence, while the least prevalence was observed among stockbreeding workers with 4 (0.95%) cases (Table 5). A calculated P-value of 0.000 was less than 0.05, indicating the significance of the correlation between the numbers of patients and different occupations.
| No. (%) | |
|---|---|
| Occupation | |
| Stockbreeder | 108 (25.9) |
| Stockbreeder-farmer | 110 (26.37) |
| Butcher | 8 (1.92) |
| Housewife-stockbreeder | 116 (27.81) |
| Slaughterhouse worker | 17 (4.08) |
| Stockbreeding worker | 4 (0.95) |
| Housewife | 36 (8.64) |
| Self-employed | 18 (4.33) |
| Total | 417 (100) |
| Dairy product | |
| Milk | 119 (28.54) |
| Cheese | 138 (33.10) |
| Cream | 41 (9.83) |
| Butter | 60 (14.38) |
| Colostrum | 21 (5.04) |
| Clotted cream | 31 (7.44) |
| Ice cream | 7 (1.67) |
| Yoghourt | 0 (0) |
| Total | 417 (100) |
Fresh cheese and raw milk (non-pasteurized) were the dairy products consumed most commonly by 138 (33.10%) and 119 (28.54%) cases, respectively. Ice cream was the least commonly consumed dairy product, with 7 (1.67%) cases of brucellosis reported.
Table 6 presents the clinical manifestations of 417 brucellosis cases from 2014 to 2017. The most common symptoms were musculoskeletal pain with 347 (83.21%) cases and fever with 333 (79.85%) cases. Splenomegaly was the least frequently observed symptom with 11 cases (2.63%) (P < 0.001).
| Symptom | No. (%) |
|---|---|
| Musculoskeletal pain | 347 (83.21) |
| Fever | 333 (79.85) |
| Back pain | 227 (54.43) |
| Anorexia | 216 (79.51) |
| Weight loss | 207 (49.64) |
| Fatigue | 104 (24.94) |
| Splenomegaly | 11 (2.63) |
5. Discussion
Over the course of the study, the incidence rate of human brucellosis was calculated to be 52.73 cases/100,000 inhabitants. Various studies have reported different incidence rates in various regions of Iran. From 2013 to 2015, Chalabiani et al. (11) reported the high prevalence rate of 25% in Hamadan Province followed by Markazi and Mazandaran with 24.7% and 22.5%, respectively. In 2011, Pakzad et al. (12) calculated the highest prevalence rate of 317 cases/100,000 in Koohrang County of Chaharmahal-Bakhtiari province. Furthermore, from 2012 to 2014, they reported the incidence rates of 384, 534, and 583/100 000, respectively, in Charuymaq County of East Azerbaijan Province (12). In the survey carried out by Mollalo et al. (13), the prevalence rates of human brucellosis in west and northwest were reported to be significantly higher than in any other region of Iran. As Pakzad et al. (12) presented in 2018, most of the high-risk areas for brucellosis were located in west and northwest of Iran, which confirms the findings of the present study.
In general, the prevalence of human brucellosis is higher in younger age groups than older ones (14). In the present study, the most frequently infected group was aged 31 - 45 years, while the 2006 - 2011 survey carried out by Zeinalian Dastjerdi et al. (15) in central provinces of Iran revealed that the most frequently infected group were aged 15 - 20 years. In 2014, Chegeni et al. (16) reported that the highest prevalence rate appeared in the age group of 10 - 19 years in rural regions of Iran. In the 2012 study of Ebrahimpour et al. (17) in Mazandaran Province, human brucellosis presented the highest prevalence in the age group of 10 - 50 years and the lowest prevalence among children and the elderly. In 2013, Kassiri et al. (18) conducted a survey in western Iran and reported the highest prevalence in the age group of 15 - 24 years. Various studies from Iran and other countries presented that human brucellosis is most prevalent among young and middle-aged people (11, 19, 20). Since close contact with livestock is one of the most common ways of transmission, it is understandable that young and middle-aged people present the highest prevalence. Of course, the age distribution of patients may show trends towards other age groups depending on cultural and regional conditions; for instance, in endemic areas of human brucellosis the age of infected patients is declining (21).
In the present study, a higher prevalence rate of brucellosis was observed in men compared to women. In 2018 with a population of 191921 people, the highest prevalence rate was reported to be 64 cases/100,000. In the same year, 53.65% of patients were male, and 46.35% of patients were female. It is also confirmed by other studies that men seemed to be affected more than women. Chalabiani et al. (11) reported that 57.6% of patients were male, and 42.3% were female. Furthermore, in the studies conducted by Kassiri et al. (18) and Ebrahimpour et al. (17), a higher prevalence rate of human brucellosis was observed among men compared to women. In 2010, Donev et al. (22) indicated that men were infected with human brucellosis more often than women. There are, of course, reports whose results contrasted with the present findings. In Uganda, Makita et al. (23) observed a significantly higher prevalence rate among women than men. Furthermore, Nematollahi et al. (24) also displayed that female sex was a significant risk factor for human brucellosis in Hamadan province during 2009 - 2015. Since human brucellosis is mainly transmitted through contact with livestock and consumption of unpasteurized dairy products, the disagreement between various studies in the male-female frequency of the disease can probably be attributed to the fact that regional and cultural differences play a major role in the higher involvement of men or women in livestock-related activities.
In terms of occupation, women working as housewives-stockbreeders with 116 (27.81%) cases and men working as stockbreeder-farmers with 110 (26.37%) cases showed the highest prevalence, while the least prevalence was observed among stockbreeding workers with 4 (0.95%) cases. Although occupation is an important risk factor in contracting brucellosis, in the developing countries it is not merely an occupational disease, but other risk factors such as ingestion of unpasteurized dairy products, educational status, and environmental sanitation are also involved (25).
According to the results, the incidence rate of human brucellosis was high in Salmas, and most of the patients were men from rural areas. In 2018, about 83% of patients were from rural regions. In the studies conducted in Azerbaijan Area, the majority of patients were based in rural regions (26, 27). Furthermore, Eini et al. (5) reported that 72% of patients came from rural regions in Hamadan, northwest of Iran.
5.1. Conclusions
It is concluded that human brucellosis has to be considered a public health priority in rural regions to be prevented or controlled by educating farmers and people living in endemic areas. Lack of hygiene education programs, especially among the ignorant and the illiterate, is one of the imperative factors for declining human brucellosis prevalence. Unfortunately, the authors’ access to personal health records was restricted because, in most of the cases, the data were not well-documented.