1. Introduction
Coronavirus 2019 (COVID-19) is an emerging disease in the world that has become one of the biggest challenges of the century. Individuals infected with the virus during this period have experienced many different symptoms, from asymptomatic to critical conditions. Respiratory symptoms of this disease include shortness of breath and cough, as well as other symptoms such as fever, myalgia, gastrointestinal manifestations, and rarely neurological complications (1, 2).
Iran was one of the first countries badly hit by the virus, and despite all efforts, unfortunately, it is still the top country in the Middle East with more than 293,000 confirmed cases and around 16,000 deaths by 28 January 2020 (3).
There have been recent reports of severe multisystem syndrome in individuals under the age of 21 years.
Recent reports from Europe and the United States support the emergence of a new phenomenon with a significant hyperinflammatory response in previously healthy asymptomatic children related to SARS-CoV-2 infection. Multisystem inflammatory syndrome in children causes inflammation in various organs such as the heart, kidneys, skin, lungs, brain, etc. The symptoms of this disease are similar to Kawasaki disease and toxic shock syndrome, but the extent of general inflammation in the body is much greater (4).
The most common causes of death in these patients included multiorgan failure (28%), respiratory failure (70%), cardiac failure (15%), renal failure (4%), and hemorrhage (6%) (5). A recent prospective study showed that pulmonary embolism was the direct cause of death in four (33%), and deep vein thrombosis was observed in seven (58%) patients (6). A study showed intra-alveolar hemorrhages and intra-alveolar fibrin cluster formation in the autopsy of four patients (25%) (7).
Hemoptysis refers to the presence of blood in the sputum, coming from the lower airway under the glottis. A mild type of hemoptysis means < 5 mL of blood loss, mild-to-moderate hemoptysis means 6 - 240 mL of blood loss, and massive hemoptysis means more than 240 mL of blood loss (8).
The case of a child with post-COVID hemoptysis and GI bleeding was reported in this study.
2. Case Presentation
A 10-year-old male patient was admitted to Ali-Ibn-Abitaleb Hospital in Zahedan on 14 September 2020 due to cough, fever, and dyspnea for three days. His temperature was as high as 39°C. There was a history of COVID-19 in the patient's mother. His health and development were good, and no food and drug allergies, hemorrhagic disease, heart disease, liver disease, tuberculosis, bronchiolitis, or asthma were observed in the patient and his family members. He was alert during the examination and had tachypnea. Abdominal examination was normal. At hospitalization, vital signs were as follows: T = 39°C, pulse = 100 times/min, respiratory rate = 35 times/min, blood pressure = 100/65 mmHg, SpO2 = 90% in room air, no congestion in the pharynx, no swelling of the tonsils, no petechiae and purpura lesions, and breath sounds in the lung, and wet rales were recorded.
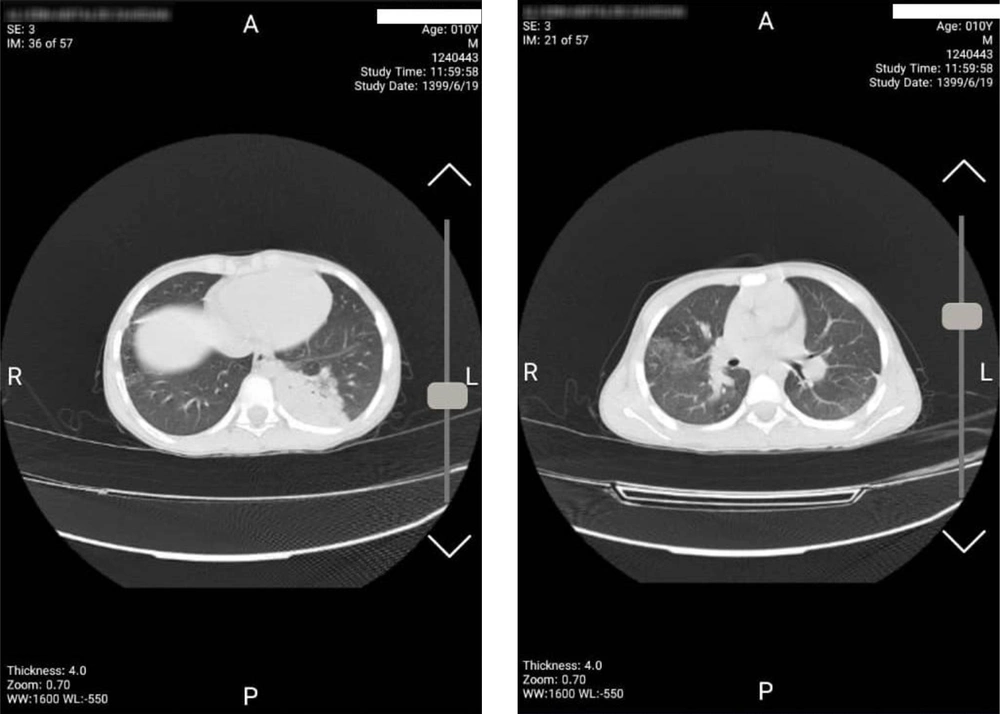
Laboratory data were checked in this center and the results were as follows: Leukocyte = 26 × 109/L, erythrocyte = 4.25 × 1012/L, neutrophil ratio = 92%, lymphocyte ratio = 6.12%, absolute value of lymphocyte = 1.5 × 109/L , hemoglobin = 13 g/L, platelet = 383 × 109/L, CRP = 96,ESR = 80, ALT = 15, AST = 23, PT = 11, PTT = 25, INR = 1 ,COVID-19 PCR = negative, fungal infections = negative, and influenza A and B = negative. The patient's echocardiography was normal. A chest CT scan showed consolidation at peripheral of the left lung with multilobar patchy and ground-glass opacity in the bilateral lung which was highly concerning for COVID-19 infection (Figure 1).
The patient was treated with antivirals, dexamethasone, and antibiotics for bacterial superinfections. Due to the severity of the disease, in addition to corticosteroids, intravenous immunoglobulin (IVIG) was also prescribed for the patient. He was discharged in good general condition without fever and other symptoms. On 5 October 2020, 2 weeks after discharge from the hospital, the patient went to the emergency room with cough and hemoptysis following exercise. On examination, he was alert but restless and had respiratory distress. Patient admission examination showed these results: T = 36.8°C, P = 130 times/min, RR = 42 times/min, BP = 75/55 mmHg, SpO2 = 88% in room air, and breath sounds in the lung and wet rales were recorded. Laboratory data in the hospital showed the following results: White blood cell (WBC) = 11 × 109/L, neutrophil ratio = 74%, lymphocyte ratio = 19.5%, hemoglobin = 10.2 g/L, platelet = 309 × 109/L, CRP = 15, ESR = 56, ALT = 26, AST = 16, PT = 13, PTT = 20, INR = 1, and D-dimer = 42 ng/ml. A chest CT scan showed consolidation and ground glass in the left upper lobe (LUL) and the right upper lobe (RUL), consolidation collapse at the base of the left lung, and a pattern of alveolar filling in favor of blood aspiration (Figure 2).
The patient was immediately transferred to the pediatric intensive care unit (PICU). Intubation, oxygen therapy, and anti-cough and supportive measures were performed for the patient. The patient was evaluated and managed by a medical team consisting of a pediatric infectious disease specialist, a pulmonologist, a thoracic surgeon, and an anesthesiologist.
Due to decreased hemoglobin, the patient underwent pack cell transfusion. The patient suffered from gastrointestinal bleeding and massive hemoptysis during hospitalization. Gastric lavage and octreotide were administered. Despite all the supportive measures, including medication and transfusion of products, unfortunately, the patient expired within 3 hours after admission to the PICU.
3. Discussion
The case of a child with post-COVID-19 hemoptysis and GI bleeding shows the life-threatening effects of the COVID-19 virus.
The first cases of coronavirus 2019 (COVID-19), the leading cause of acute respiratory syndrome in China, were identified in December 2019, with a large number of infections and subsequent deaths worldwide increasing daily (9, 10). Respiratory failure was the most common cause of death in these patients (11).
In addition to respiratory failure, gastrointestinal and respiratory bleeding due to microvascular damage and thrombosis can also cause mortality. In a study by Magro et al. on 5 patients with COVID-19 and respiratory failure, lung and skin tissues were examined, and no viral cytopathic change or diffuse alveolar damage was observed in COVID-19 pneumonitis, but a capillary lesion by neutrophils. These pulmonary findings were found in small vessels with significant deposits of the complement components of C5b-9 (membrane attack complex), C4d, and lectin-dependent serine proteinase (MBL). Similarly, a thrombogenic vasculopathy with inflammation of the pauci, with C5b-9 and C4d depositions, severely involved skin and showed a normal appearance (12).
A study by Kumar et al. showed that COVID-19 disease can cause hypercoagulopathy. Patients recovered from COVID-19 require a follow-up post-discharge for a period of at least 1 month, and patients at higher risk for thrombosis require prolonged anticoagulation (13).
As a result, at least one subset of persistent and severe COVID-19 may modify a catastrophic microvascular injury syndrome that is modified by activation of complement pathways and an associated coagulation state. This provides a basis for further exploration of the pathophysiological significance of complement in COVID-19 and suggests specific targets for future interventions.
3.1. Conclusions
As this virus spreads, patients are more likely to present with COVID-19. COVID-19 can have a variety of presentations and complications that are beyond the classic respiratory symptoms and fever. The case is remarkable in terms of showing how insidious and life-threatening COVID-19 infection can be. Due to the unknown nature of many of the complications of this virus, including GI bleeding and hemoptysis raised in this case, paying special attention to patient care during recovery, as well as the follow-up required for these patients is necessary.