1. Introduction
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) emerged in Wuhan city, China, in December 2019. The novel coronavirus disease (COVID-19) became a global pandemic over a few months (1, 2). At the beginning of the pandemic, in the Kurdistan region of Iraq, strict measures were implemented to combat the spread of the SARS-CoV-2 infection (1). However, political necessity and mounting socioeconomic pressure demanded a reopening process that was started at a progressively rapid pace (2). After reopening, the number of COVID-19 cases increased sharply with a concurrent increase in the number of symptomatic patients and a two-fold increase in the case-fatality rate (2).
We here report a 39-year-old male who underwent emergency surgery for COVID-19-associated intestinal ischemia.
2. Case Presentation
A 39-year-old married non-smoker male presented with intractable abdominal pain and fever for about a few hours. He had no past medical history of this condition. Localized central pain started gradually from the past four days, and it was dull in nature. The patient suffered from severe pain and showed generalized tenderness, mainly above the umbilicus. Other clinical findings included pallor, a heart rate of 110 B/min, respiratory rate of 22 breaths/min, and blood pressure of 115/65 mmHg. Serum amylase, lipase, and liver functional enzymes were normal. Other laboratory tests showed the following: hemoglobin level = 12.8 g/dL, white blood cell count = 12.8 × 109/L, platelet count = 188 × 109/L, C-reactive protein = 59 mg/L, blood urea nitrogen (BUN) = 62 mg/dL, and serum creatinine = 2.1 mg/dL. Abdominal X-ray at the erect position showed multiple air-fluid levels, and CT scan was not available for urgent scanning. Written informed consent was taken from the patient. Exploratory laparotomy was performed under general anesthesia and through a midline incision.
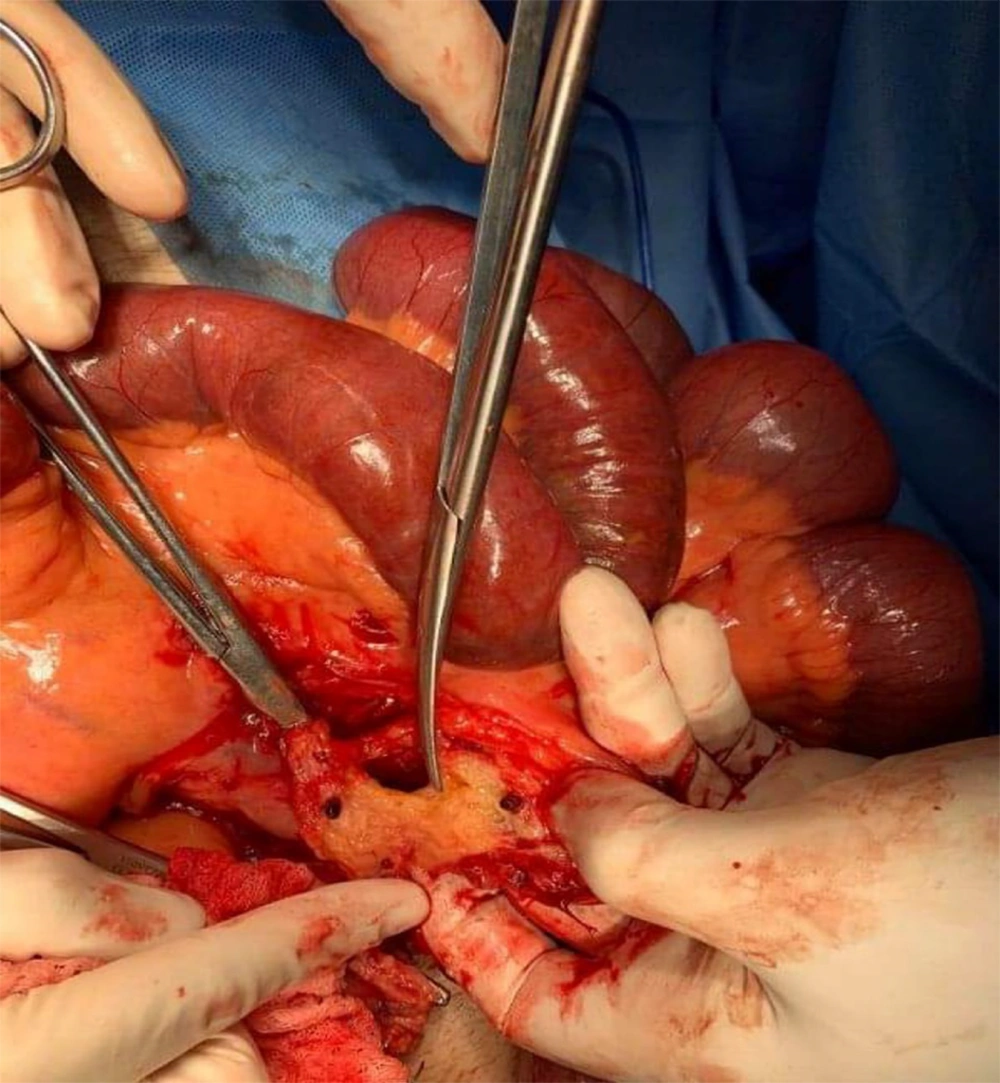
The patient underwent an emergency laparotomy showing segmental small bowel ischemia of about 2 meters (between the lower jejunum and upper ileum). The bowel was floppy and in an irreversible ischemic status (Figure 1). The resection of the ischemic segment was performed through the end-to-end anastomosis.
After the surgery, the patient was admitted to the HDU ward and greatly improved within two days. The pain subsided, urine output was adequate, and bowel movements became positive. Subsequently, oral liquid diets started for the patient. Both BUN and serum creatinine returned to normal. However, the patient still suffered from mild fever and cough. Because of persistent post-operative fever, a chest CT-scan was conducted, revealing focal-patchy peripheral and subpleural ground glass involvement of both lungs, mainly at the posterior segments of both lower lobes. Then a nasopharyngeal swab test was performed, which confirmed the COVID-19 diagnosis. The patient was admitted to a COVID-19 hospital where he was treated with favipiravir (800 mg P.O. bid on the first day and then 600 mg P.O. bid for five days) plus levofloxacin (500 mg po for seven days). Then the patient clinically improved, and the PCR test rendered a negative result two weeks later.
3. Discussion
COVID-19 is an acute respiratory infection caused by SARS-CoV-2. Facing a pandemic emergency is challenging in low-resource countries such as Iraq. Around the world, gastrointestinal (GI) symptoms, mainly diarrhea, have been described in 10% of COVID-19 patients. Such symptoms are usually mild and without deleterious consequences (3). However, a few cases may present with severe GI symptoms associated with intestinal ischemia. In a report from Italy on seven patients with COVID-19-associated intestinal ischemia, an increased mortality rate was demonstrated in such patients (4). Our patient presented with severe and intractable abdominal pain and fever. The patient had no history of a similar clinical phenomenon and previous surgery, as well as no thromboembolism risk factors. During the operation, there was evidence of ischemia involving about two meters of the bowel length. Although the patient started to complain of mild pain from four days earlier, due to a low suspicion threshold, the diagnosis was missed, and therefore he was treated as a case of UTI. Due to the growing evidence linking COVID-19 to coagulopathy and previous reports of COVID-19-associated bowel ischemia, the role of COVID-19 infection in the occurrence of intestinal ischemia in our patient was highly probable. The exact mechanism of acute mesenteric ischemia is not fully understood yet. Four putative mechanisms have been proposed for such a fulminant complication, including the hypercoagulability provoked by systemic inflammation, endothelial activation, hypoxia, and immobilization, which may lead to mesenteric vascular thrombosis (4).
Based on the case presented here and previous reports on COVID-19-associated bowel ischemia, this condition should be considered in the COVID-19 patients presenting with gastrointestinal complications, including abdominal pain. Early interventions in such a condition may save the patient’s life, particularly in low-resource countries where CT scanning may not be available in emergency situations and in all hospitals. Simple X-ray at the erect position may help to early detect the condition and timely decisions on the operation.
3.1. Conclusions
Mesenteric ischemia should be highly suspected in the patients with COVID-19 presenting with severe progressive abdominal pain in order to perform timely diagnostic testing and appropriate decision making. Further studies are needed to understand the role of SARS-CoV-2 in the pathogenesis of this condition.