1. Context
The hospital is a fundamental site for the creation of waste. Every hospital office creates squander, and the item overall is a misuse of various kinds, sterile, homegrown, and authoritative (1). The specific clinical waste like disposing of wound dressings, expired synthetic substances/drugs, radioactive materials, and rough materials (needles, surgical blades, scissors, and so on). Since these materials cause pathogenic and natural calamities, they should be treated efficiently (2).
Individuals who work in medical care and scroungers when presented with this waste because of microbial contamination. Ill-advised treatment of sharp articles can cause the needle to leave wounds and lead to contamination with blood-borne microbes (3).
Untreated waste causes cerebral pains, dazedness, sickness, tissue harm, fetal neoplasms and distortions, heart, and respiratory infections (4).
The administration of waste produced by hospitals is the obligation of hospital workers and everybody in every division. The development of dangerous clinical waste should be all around constrained by its creation, treatment, and removal (5).
The main foundations of healthcare waste are blood banks, clinics, pre-clinical and clinical labs, mortuary/autopsy centers, and nursing homes. We aimed to give information to follow and adapt to maintain cleanliness and hygiene in the hospital.
2. The Rules on Waste in India
India planned the rules on the organization and treatment of bio-medical waste (BMW) in 1998 and amended them in 2016. The rules enclosed by the Central Pollution Control Board (CPCB) to aid in the execution of the rubrics: (1) strategies for the supervision of BMW management in 1998; (2) recommendations for the Common Bio-medical Waste Treatment Facility (CBWTF); (3) plan and building of BMW incinerator.
3. Steps Involved in Hospital Waste Management
There are various measures in the hospital’s organization waste as follows (6): (1) training and awareness, (2) generation, (3) separation, (4) collection, (5) transportation, (6) storage, (7) treatment, (8) final disposal.
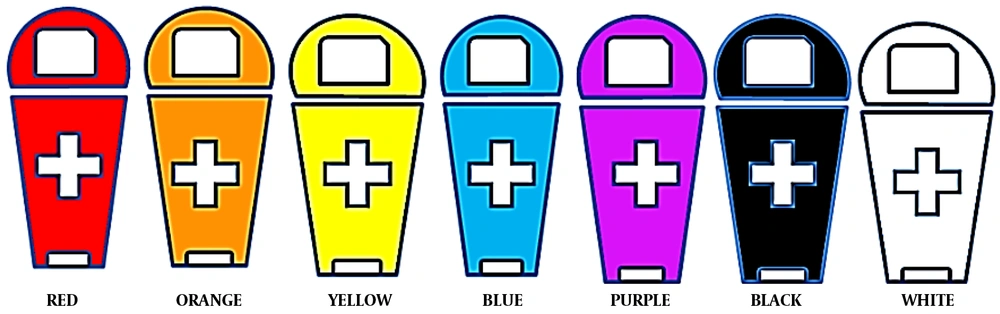
The WHO has recommended a color code for the respective waste bins (Table 1 and Figure 1) (7).
| Waste Material | Bin Colour |
|---|---|
| Chemical pharmaceuticals | Brown |
| Clinical/infectious | Orange |
| Cytotoxic and Cytostatic products | Purple |
| Dental wastes | White |
| General wastes | Black |
| Highly infectious | Red |
| Infectious/pathological/ anatomical | Yellow |
| Liquid wastes | Blue |
| Radioactive | Silver |
| Sharps | Yellow |
The waste collectors should wear protective gloves, collect and segregate the waste materials into colored bags/bins. These bags should be zipped tightly around the neck.
4. Final Discarding Methods
Finally, the collected waste has been discarded by the process of incineration (at > 1200°C), chemical disinfection, or by rendering it inert. The various strategies and categories of waste disposal in the hospital are as follows.
4.1. General and Harmful Waste
According to the set of laws for industrial waste, hospital waste should not be added to a sewage line. For example, sugar, lactic acid, bromides, or carbonates. Even though they do not adversely harm human health, they must be first collected, accumulated, treated, and dumped in secured landfills (8).
4.2. Liquid Waste
They should be treated with a chemical disinfectant, neutralized, and discarded into the sewage. The liquid waste oriented from hospitals is of the following types (9).
4.3. Contagious Waste
These include blood, body fluids, laboratory wastes (cultures of contagious microbes, eliminated vaccines, culture dishes, etc.) (10).
Autoclaving and securing culture media in autoclavable bags can ensure that media in Petri dishes are free from microorganisms. Again, the bags are sterilized and passed on to micro waste containers that are disposed of in municipal trash or incinerated.
Currently, there are no new methods available, the same approaches are used, but they need to be strictly monitored and analyzed. Dispose of dirty and unpolluted glassware, and sterilize contaminated broken glassware. Incineration or industrial waste disposal is used to dispose of these materials. Uncontaminated glassware from urban waste can be disposed of.
4.4. Chemically Dangerous Materials
These forms are as follows (11, 12): (1) formaldehyde (got from pathology labs, autopsy, dialysis, and embalming); (2) mercury (damaged thermometers, sphygmomanometers, and dental amalgams); (3) solvents (organic solvents from pathology and embalming); (4) radioactive isotopes (F18, Ga67, Kr81, Ru82, N13, Te99, In111, I123, Xe133, and Th201).
4.5. Pharmaceutical Liquid Waste
These forms of disposal contain unused/expired medications like chemicals used in photography (fixer and developer) and water after cleaning/washing hospital materials/instruments left in the drain. The liquid waste comprises either emancipation from health care amenities (HCF) or from household, commercial layouts, industry, and agricultural lands, which cover an extensive variety of growing contaminants and microbes. Sewage is a section of waste that has been polluted with feces and urine (13).
4.6. Human Anatomical Waste
Pathological and bodily wastes comprise almost everything from laboratory cultures and pileups of donated blood to tissue biopsied for testing/diagnosis/removed owing to ailments (14). These are a sub-category of pathological waste, those materials that are noticeably human such as a removed limb. Even with an effective septic scheme and a sufficient sewage treatment system, some pathological waste can be disposed of in the drain.
Wastes, like placentas from mothers after delivery and expired blood, may not be infectious, but their status is recognized. Sometimes, the amputated limbs are buried or cremated in a similar pattern as a dead person (15). Blood and placentas are necessarily disposed of in the cesspits using a macerator. This material must be first autoclaved as a preventive measure before it is further re-processed for disposal.
Bio-digestion is a present technology that has been adopted for treating such pathological wastes. However, this technique needs a long time to destroy all pathogens and guarantees that the slurry has been dealt with well. This slurry should not be used as fertilizer later.
4.7. Abrasive Metallic Waste
These are biomedical waste, which comprises any device/object used to puncture/lacerate the skin. Sharp waste has been considered bio-hazardous and should be handled cautiously.
Extreme attention must be paid to the removal and control of sharp wastes, as they must be carefully handled until they can be suitably discarded. The last step in disposing of sharps is by burning or autoclaving (16, 17).
There is a risk of injuries and infections associated with improper disposal of needles and syringes, as well as potential for reuse. Recent efforts to reduce reuse of injection devices have helped significantly reduce injections with contaminated needles and syringes in low- and middle-income countries. In addition, a hazard may arise during scavenging and during the manual sorting of hazardous waste at health care facilities. The practice is widespread in many parts of the world, especially in parts of the world with low and middle incomes. Those who handle waste are at risk of needle stick injuries and being exposed to potentially harmful substances.
4.8. Microbiology Wastes
The microbial wastes in the culture media of glass Petri plates must be sterilized by autoclaving and then repacked in autoclaving bags. Later, these bags are re-sterilized by autoclaving and then moved to micro-waste, which is then discarded either by incineration or municipal trash (18).
4.9. Radioactive Waste
If the removal of radioactive waste has not been managed and planned properly, it could lead to a drastic environmental disaster. Solid waste is discarded by accumulating and storing it, which is a trending approach for nuclear waste disposal. The storage should be done in steel or lead cylinders as a radioactive shield (19).
Hospitals use sealed sources for a variety of applications, such as teletherapy, brachytherapy, blood irradiation, and calibration. With the exception of the teletherapy and blood irradiation sources, those having high activity levels are generally relatively small. A source must be replaced once it becomes incapable of supporting future applications. To make sure that the sealed radioactive sources are safely removed and replaced, hospitals must enter into a contract with the suppliers. To order such equipment and the source, a hospital's Radiation Safety Officer should be consulted.
5. Novel Approaches to Disposal
The latest approaches to cleaning and destroying pathogenic waste (20-22) are summarized in Table 2.
| Waste Material to Be Treated | Approach Adopted |
|---|---|
| Pathological waste, infectious, plastic, hazardous chemicals, or pharmaceutical waste | Plasma pyrolysis by plasma torches/electrodes (use of ionized gas to convert electrical energy to thermal energy) |
| Microbes | Ozonation |
| Dead bodies and parts before entombment | Freeze drying in liquid nitrogen and automated shaking |
| Body parts, specimens, and cadavers | Alkaline hydrolysis |
| Infectious bones and teeth | Alkali solution at > 127°C |
| Cleaning environmental air | Nano formulation of hydroxyl species and superoxide anion (O2-) |
| Sludge water separation | Membrane bioreactors |
| Wastewater treatment | Photocatalysis |
| Cultures, materials filthy with blood and fluids, laboratory waste, and medical instruments | Pre-vacuum autoclaves (121°C for 30 min, pressure of 205 kPa) |
| Reducing the volume | multiple-shaft shredders which cut volumes < 80% |
| Culture media, blades, things tainted with blood and body fluids, other diseased left-overs, laboratory leftovers, and soft waste (e.g., gauze, bandages, gowns, and bedding). | Microwave oven (30 cycles per min for 1 h) Confirmed by biological indicators Bacillus atrophaeus spores’ vials/strips with at least 104 spores. |
| Glassware and other reusable instruments | Hot air oven (up to 185°C for 90 - 150 min. cleaning confirmed by the spores of Geobacillus stearothermophilus or Bacillus atrophaeus with at least log106 spores per ml/indicator strip |
| Bacteria, viruses, and spores | 1 - 12% Sodium hypochlorite (NaOCl) |
| Disinfecting instruments | Calcium hydroxide, Glutaraldehyde, and peracetic acid are used |
| Inorganic, incombustible matter | Incineration (600°C to > 1,000°C) |
6. Better Practices for Hospital Waste Management
Remedial waste is hazardous, spreadable, toxic, and even lethal to humankind. If these materials are not correctly disposed of, treated, they lead to health disasters for humans and the environment (23). Problems like disease spread, ecological poisoning, and contamination result. To ensure safe and protective management of medical waste, the following practices should be adopted.
6.1. Keep a Check of State Rules and Regulations
The protocol for the disposal of hospital waste was set by country/state rules. These rules help maintain and manage hospital waste creating a healthy environment as well as keeping up and keeping the medical facility constructed (24). These rules will keep organizations accredited with training, courses, and other possessions to bring awareness among people about executing proper waste management.
6.2. Color Code Containers and Waste Bins
Hospital waste is broadly characterized into multiple types, and each type needs a specific disposal method. Filtering the various medical waste ensures each type was discarded, disposed of, elated, and devastated precisely, and so on (25). Color coding helps stop deadly health issues arising from mislabeled medical healthcare waste.
6.3. Monitor and Regulate Waste
Evaluate the success of the waste disposal and management system with a monitoring tool that easily guesses the workflow. Conducting regular inspections periodically throughout the waste management process, from filtration and gathering to storage, conveyance, and disposal (26-28).
The practices to safeguard proper waste supervision in hospitals are summarized as below: (1) it minimizes the spread of infections and reduces the risk of unintentional injury to staff, patients, and visitors, and the community; (2) it reduces the probability of infection of the soil or groundwater with chemicals or microbes; (3) it attracts fewer insects and rodents that are not attractive to animals; (4) it helps create a healthy environment.
7. Monitoring of Waste in Hospitals
Monitoring is a continuous and never-ending process. State pollution control boards (SPCBs), monitor and manage BMW. The Ministry of Environment, Forest, and Climate Change (MOEFCC) examines the rules through district, state, and central authorities. In hospitals, the waste management committee watches and controls the BMW.
8. Infringement
Any violation of the rules, healthcare facilities, and CBWTFs are answerable as per sections 5 and 15 of the environment protection act. Hospitals that cannot keep up with BMW will be punished and penalized (29).
9. Records
Healthcare facilities were required to keep up records of the generation, gathering, treatment, packing, conveyance, treatment, removal, or any other form of control of BMW for five years. The central or state pollution control boards and MOEFCC regularly verify these documents.
10. Conclusions
Proper training, regulation, and devoted infrastructure help in the effective management of hospital waste disposal. These safeguard precautions and effective disposal protect hospital staff, patients, the public, and the environment, which provides a clean and safe environment. The novel approach to the waste management system in treating hospital waste and disposal as per the color codes of the bins is simple and effective in identification and disposal of waste in hospitals. Still, a proper plan, protocol, and research are required for the effective disposal of waste for hospitals to give a hygienic and healthy life to the globe.