1. Background
One of the most common infections of the eyelid and periorbital soft tissues is preseptal cellulitis that is characterized by acute eyelid erythema and edema (1). Primary sources of infection can be local skin trauma, sinus infections or penetrating trauma, specifically those involving the ethmoid sinus (2, 3). Most of the time, this kind of bacterial infection results from local spread of an adjacent sinusitis or dacryocystitis, from an external ocular infection, or following trauma to the eyelids (4). Fever is typically observed, however conjunctival hyperemia is typically absent (2). Preseptal cellulitis may progress to form subperiosteal and orbital abscesses and spread posterior to the septum. Cavernous sinus thrombosis or meningitis could be the result of infection in the orbit and spread posteriorly (5). The most common organisms are Staphylococcus aureus, Staphylococcus epidermidis, Streptococcus species, and anaerobes, which are reflecting the bacteria that usually cause upper respiratory tract infections and external eyelid infections (3).
Pseudomonas aeruginosa, Neisseria gonorrhoeae, Treponema pallidum, Mycobacterium tuberculosis, Bacteroides species, and fungal infections are rare causative organisms (6, 7).
During last decades, in 1985, Haemophilus influenzae was the most common organism isolated in blood cultures before the introduction of the Haemophilus influenzae type b (Hib) polysaccharide vaccine (8, 9).
Various antibiotic regimens have been used for the treatment of preseptal cellulitis infection such as ampicillin, cefuroxime, ampicillin with sulbactam, ampicillin and nafcillin and ampicillin and chloramphenicol (6).
Similar symptoms have been observed in patients with preseptal or orbital cellulitis, such as eye pain, periorbital swelling, and/or fever. Differentiation between the 2 infections is very important since the treatment for each is different. The aim of this study was to evaluate risk factors in patients with preseptal cellulitis admitted to two educational hospitals in Tehran, Iran.
2. Methods
This descriptive prospective study was conducted on patients with preseptal cellulitis hospitalized at the Imam Hossein and Labaffi-Nejad hospitals during 2014 - 2015.
The clinical features, diagnosis and risk factors were entered on a specially-designed proforma. The risk factors included trauma, symptoms, examination findings, treatment and CT scan reports. Odd ratio and P-values were calculated for potential risk factors. Statistical analysis was performed using the SPSS software version 20.
3. Results
During the study period, 40 patients who were diagnosed with preseptal cellulitis were identified. The mean age was 38.95 years. Nineteen patients (47%) were males, and 21 (53%) were females.
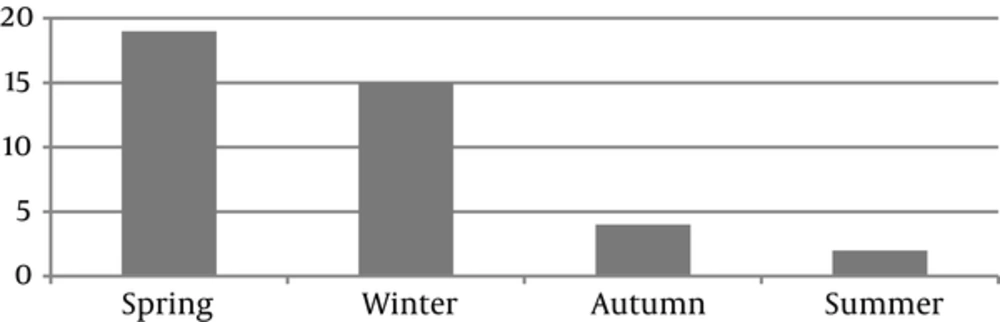
While in the orbital area, cellulitis with paranasal has a close relationship with sinus and upper respiratory disease, a seasonal distribution paralleling that of upper respiratory tract infections might be expected. Figure 1 shows the seasonal distribution of the participants. The higher frequency was observed in winter and spring.
3.1. Predisposing Factors
In our study, trauma (insect bite and blunt trauma) and sinusitis were the most common predisposing factors. Table 1 shows the associated diseases of our participants.
| Predisposing Factors | No. (%) | P Value |
|---|---|---|
| Trauma | 23 (57.5) | < 0.05 |
| Insect bite | 15 (65) | |
| Blunt trauma | 8 (35) | |
| Sinusitis | 10 (25) | < 0.05 |
| Ophtalmic zoster | 4 (10) | < 0.001 |
| Dacryocystitis | 2 (5) | < 0.001 |
| Hordeolum | 1 (2.5) | < 0.001 |
One of the most common underlying diseases was sinusitis, which was present in 25% of the preseptal cellulitis cases with the ethmoid sinus being the most common involved sinus (Table 2).
| Involved Sinus | No. (%) |
|---|---|
| Ethmoid | 4 (40) |
| Maxillary | 2 (20) |
| Ethmoid + Maxillary | 4 (40) |
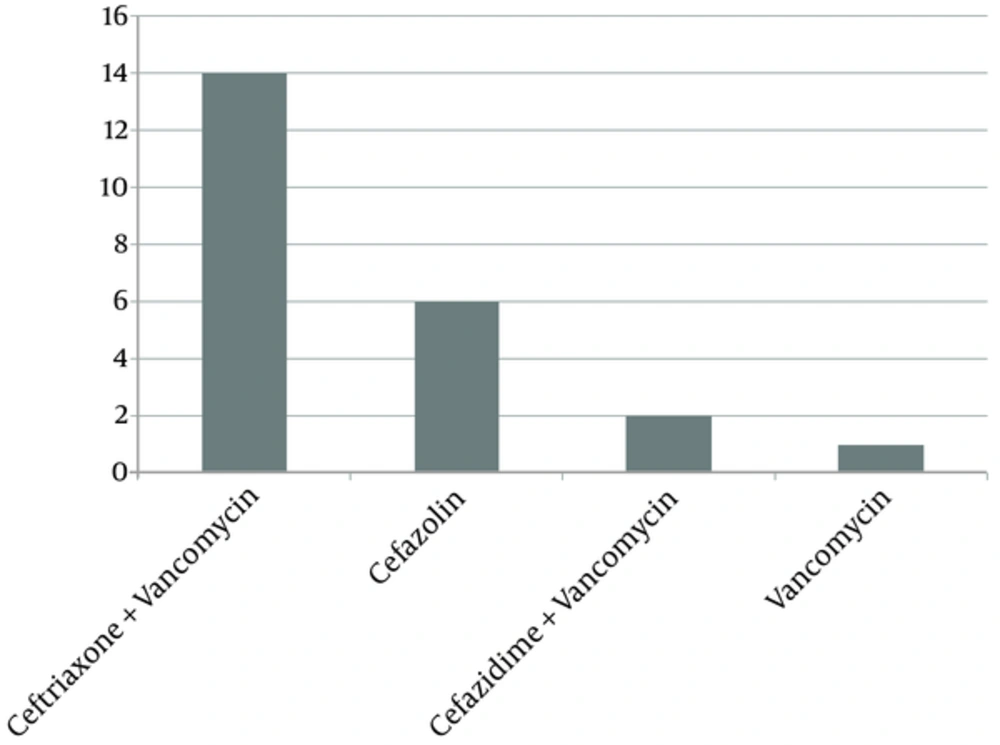
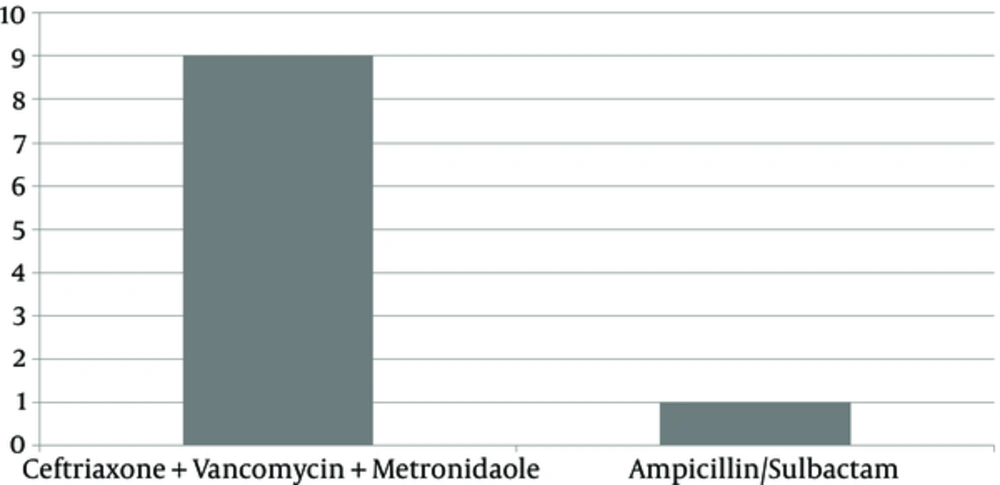
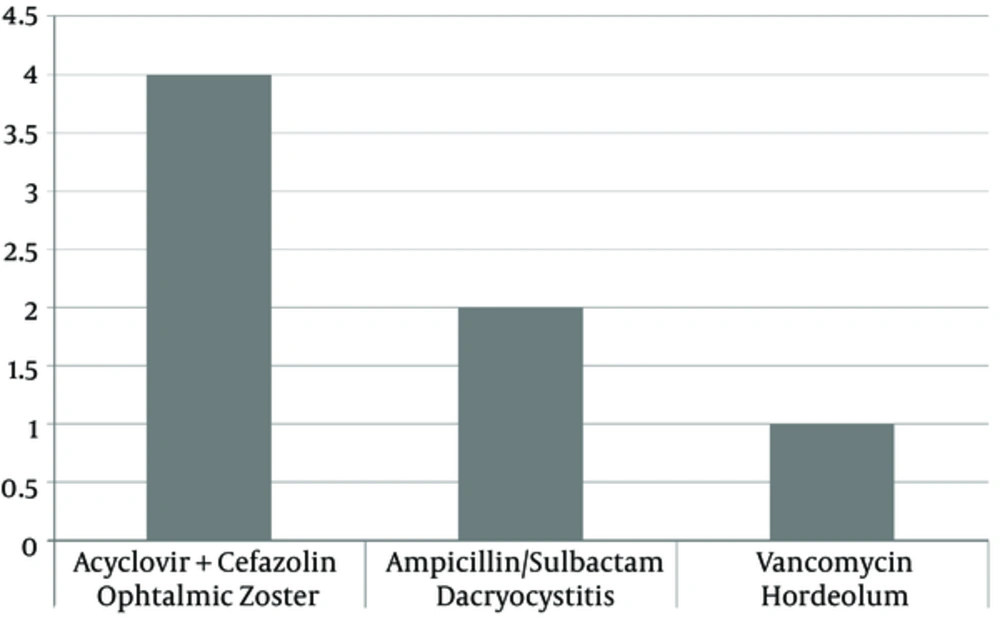
The most commonly used antibiotics included vancomycin, ceftriaxone, cefazolin, ceftazidime, metronidazole, ampicillin/sulbactam and acyclovire. The Figures 2 - 4 show the numbers treated with the various antibiotics used in case of trauma, sinusitis, ophtalmic zoster, dacryocystitis and hordeolum.
4. Discussion
Preseptal cellulitis is a distinct disorder that explains an infection of the eyelid and superficial periorbital soft tissues, which do not involve the globe and orbit (10). One of the most common ocular diseases is a cellulitis in the orbital area, relatively. It can usually be treated effectively with antibiotics. Rapid diagnosis is very necessary, since a delay in detection, diagnosis and management can cause serious complications such as vision loss, cavernous sinus thrombosis, meningitis, and sepsis.
Preseptal cellulitis and orbital cellulitis can both present with increasing swelling, tenderness and redness around the eye, but their management differs. Preseptal cellulitis is more common and much less aggressive than orbital cellulitis (11). Preseptal cellulitis characterizes a cellulitis of the tissues localized anterior to the orbital septum. This distinction is important, as orbital cellulitis, while less common, may be associated with significant visual and life-threatening sequelae, including optic neuropathy, encephalomeningitis, cavernous sinus thrombosis, sepsis, and intracranial abscess formation (12).
In this study, we provided a systematic approach to distinguish preseptal cellulitis associated risk factors, which can be potentially lifesaving.
Another important sources of infection are contiguous spread of infection from the soft tissues of the face and ocular adnexa and could result from trauma, foreign bodies, insect bites, skin infections (impetigo), eyelid lesions (chalazia, hordeola), and iatrogenic causes such as eyelid and oral procedures (13).
Ferguson et al. (14) explained that a seasonal variation in orbital cellulitis was attributable to the increased incidence of upper respiratory tract infection and paranasal sinusitis in the same seasons of the year. In our pediatric patients who have orbital cellulitis, this inclination in winter was typically demonstrated. In addition, in other research, there were also smaller peaks in winter or spring, showed a seasonal preference of cellulitis in the orbital area.
Multiple factors can cause preseptal cellulitis, the following are common ones: having ocular trauma, paranasal sinusitis, upper respiratory tract infection, acute or chronic otitis, and dental origin (15, 16). Interestingly, in our series, the most common predisposing factors of preseptal cellulitis were trauma and sinusitis. Decaryocystitis and hordeolum were relatively minor factors. According to guidelines perceptual cellulitis due to sinusitis should be treated with antibitics active against S. pnemonia, H. influenza, and S. sureus. On the other hand, on case of perseptual cellulitis due to secondory infection of skin lesion antibiotics that are also active against group A streptococcus and S. aureus and sometimes MRSA. Especially in Staphylococcus and Streptococcus species, selection of antibiotic is completely directed towards causative agents of sinusitis and trauma, which can be considered as the predisposing factors of preseptal cellulitis (17).
In conclusion, preseptal cellulitis is more prevalent in age of 40; a seasonal preference of winter and spring has been explained in our patients. In our study, the most common predisposing factor was trauma, while other studies focus more on sinusitis factor.