1. Background
In December 2019, an outbreak of pneumonia caused by coronavirus disease 2019 (COVID-19) emerged in Wuhan, the capital of Hubei province, China (1). Since then, the infection has spread globally, with significant numbers occurring in Asia, Europe, and other regions of the world (2, 3). Initially, those infected outside China were reported in individuals who had traveled to China or had been in contact with tourists from China. However, there are now increasing reports of community outbreaks, including within the United States of America (4). As of April 2020, a total of 2,878,196 confirmed cases of COVID-19 have been reported in over 100 countries worldwide, resulting in 198,668 deaths (4). The average age of affected individuals was 47 years (5), with a disproportionate incidence in older men with co-morbidities (6). Approximately 2% of reported cases were pediatric cases (7, 8), and 0.9% of all affected patients were under the age of 15 (5). Although early investigations described the medical and imaging features of COVID-19 in adults (9-12), computerized tomography (CT) findings in children have only been reported in small cohorts (13-15). Rapid diagnosis is challenging in children due to milder symptoms and lower hospitalization rates than adult patients (8, 13-17). Rapid and accurate diagnosis is particularly important, as severe symptoms and deaths have been reported in pediatric patients (8). Additionally, the social and psychological impact of isolating children, as well as the economic impact on caregivers, must be taken into consideration.
2. Objectives
This study aimed to identify CT features in children with COVID-19.
3. Methods
This descriptive cross-sectional study was conducted on inpatient children aged 1 month to 18 years hospitalized with a diagnosis of COVID-19 at Ali Ibn Abitalib Hospital, a comprehensive medical center that integrates medical care, education, and scientific research affiliated with Zahedan University of Medical Sciences (ZaUMS). The study was done from March 1, 2020, to August 30, 2020. During this period, 56 pediatric patients staying in the hospital needed a CT scan. This was because their RT-PCR test was negative or they showed no improvement. They also had low oxygen levels, severe respiratory symptoms, or trouble breathing.
For these children, COVID-19 was confirmed by a positive RT-PCR result. Confirmed or suspected children were referred to the radiology department for CT scans. Two experienced radiologists looked at the CT scans separately. They did not know anything about the patient's medical history. A special CT scanner was used to take images inside the body. The machine used was made by Siemens and is called the SOMATOM multi-slice spiral scanner. They did not inject any medicine into the body using a needle for this scan. For the imaging machine, the tube voltage was between 100 and 120 kV, there was automatic exposure control, the collimation was set to 2. 0 mm, and the pitch was set to 1. We looked at CT scans from different angles to see both the lungs and the area in the middle of the chest. We found out how often normal and abnormal CT scans occurred.
A form was used to collect information about where and how the lesions were distributed in the body (one side or both sides, on the edges or in the center) and what kind of blockage was seen (hardening, hazy appearance, etc.). We also noted whether bronchiectasis, exudate, cavity, or lymphadenopathy was present. Then, we worked out how often each type of problem occurred. This study was approved by the university's ethics committee with a code of IR.ZAUMS.REC.1399.532. Data were aggregated and reported using SPSS 20.0 (SPSS Inc., Chicago, IL, USA). Mean and SD were used for quantitative variables, and frequency and percentage were used for categorical variables.
4. Results
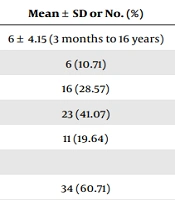
This study obtained CT scans from 56 pediatric patients infected or suspected of COVID-19 who met the inclusion criteria. The patients' ages ranged from 1 month to 16 years, with a median age of 6 years and a male-to-female ratio of 1.54:1. The demographic features of patients and age group statistics are presented in Table 1. Table 2 displays the chest CT features of COVID-19 pediatric patients, indicating that 17 patients (30.36%) had normal CT findings. Ground-glass opacity (42.86%) and consolidation (35.71%) were the most prevalent CT findings in these patients. The distribution of lesions was mostly bilateral (64.10%) and mainly peripheral (66.67%). Other findings included cavity or pneumatocele (5.36%), pleural effusion (3.57%), bronchiectasis (1.79%), and lymphadenopathy (1.79%).
| Variables | Mean ± SD or No. (%) |
|---|---|
| Age (y) | 6 ± 4.15 (3 months to 16 years) |
| < 1 | 6 (10.71) |
| 1 - 5 | 16 (28.57) |
| 5 - 10 | 23 (41.07) |
| > 10 | 11 (19.64) |
| Gender | |
| Boy | 34 (60.71) |
| Girl | 22 (39.29) |
| Variables | No. (%) |
|---|---|
| Normal | 17 (30.36) |
| Abnormal | 39 (69.64) |
| Opacities | |
| Ground-glass opacity | 24 (42.86) |
| Consolidation | 20 (35.71) |
| Nodular | 12 (21.43) |
| Reticular | 6 (10.71) |
| Crazy paving | 2 (3.57) |
| Laterality | |
| Normal | 17 (30.36) |
| Unilateral | 14 (25) |
| Bilateral | 25 (44.64) |
| Distribution | |
| Normal | 17 (30.36) |
| Peripheral | 26 (46.43) |
| Central | 11 (19.64) |
| Diffuse | 2 (3.57) |
| Other CT findings | |
| Cavity/pneumatocele | 3 (5.36) |
| Pleural effusion | 2 (3.57) |
| Bronchiectasis | 1 (1.79) |
| Lymphadenopathy | 1 (1.79) |
Abbreviation: CT, computerized tomography.
5. Discussion
This study found that 30.36% of the 56 patients had normal CT findings, while those with positive CT findings exhibited typical features such as ground-glass opacities and airspace disease, which presented as a thrombus with one or more lobes.
Notably, ground-glass opacities were more prevalent in this study, and a few patients developed pleural effusion, lymphadenopathy, and bronchiectasis. Approximately 44.64% of patients had bilateral pulmonary involvement, and 46.43% had peripheral pulmonary findings. These imaging findings suggest that COVID-19 may primarily manifest as ground-glass opacities in bilateral and peripheral lobe distributions in the pediatric population. This study is one of the largest and most comprehensive in this geographical area to demonstrate imaging findings in pediatric patients with COVID-19. The imaging results and their distribution are consistent with those published in the literature on COVID-19 in both children and adults (9-14, 18).
In this study, the detection rate of abnormal CT findings in children was only 69.64% compared to adults, which is similar to the findings of Shelmerdine et al. (64%) and Wang et al.'s study (63.2%) (19, 20). Ground-glass opacities (42.86%) were the most common CT findings in children with COVID-19 in this study, followed by consolidation (35.71%). The prevalence of these two features was slightly lower in children than in adult patients. Ojha et al. (21) reported 50.2% and 39% for ground-glass opacity and consolidation, respectively, while Wan et al. (22) reported 86% and 47% for ground-glass opacity and consolidation, respectively. Ebrahimpour and colloquies (23) examined the frequency of CT findings in pediatrics and found that the incidence of ground-glass opacity was 57.4% and consolidation was 10.2%, comparable to the present study's results. Additionally, the incidence of ground-glass opacity in Kumar et al. (24) and Wang et al. (20) studies was 40% and 39.5%, respectively, similar to our study. The rate in this study was 64.10%, compared to 61.5% in the study by Wang et al. (20) and 53.62% in the Ebrahimpour et al. study (23).
Ghodsi et al. (25) conducted the same study on children under the age of one and found a specific rate of 57.63%, and pulmonary involvement was predominantly peripheral (66.67%). In the Kumar et al. (24) study, 80% of the opacities were peripheral, and in the Ebrahimpour and colloquies (23) study, 81.2%, 15.6%, and 3.1% of children had a peripheral, diffuse, and central pattern, respectively. Other common findings in this study were pulmonary nodules and reticular opacities (21.43% and 10.71%, respectively). In Ebrahimpour et al.'s study, pulmonary nodules were observed in 2.6% of patients, and reticulation was observed in 1.7%, less than in the present study. The nodular and reticular opacity frequencies in Wang et al.'s study were 25.7% and 9.7%, respectively (20, 23). Pleural effusion (3.57%) and lymphadenopathy (1.79%) were rare findings in the current study. Other studies reported pleural effusion rates ranging from 2.7% to 9.1% and mediastinal lymphadenopathy at 0.5% (20-23). The ‘crazy paving’ pattern, one of the hallmarks of severe lung disease, was found less frequently than in adult patients. In our study, it occurred in only 3.57% of the children, whereas in adults, it has been reported as 12%, 15%, and 19.5% (21, 22, 26). In Ebrahimpour et al.'s study, the frequency of crazy patch patterns in children was only 0.6% (23). Because the CT manifestations of pneumonia caused by different pathogens can overlap, and COVID-19 pneumonia can also overlap with pneumonia caused by other pathogens, it may present with more severe and complex imaging manifestations. Therefore, combining epidemiological, etiological, and radiological investigations is important. The small sample size was the limitation of the study.
5.1. Conclusions
In conclusion, the study determined that approximately one-third of the children with COVID-19 exhibited normal CT features. Ground-glass opacity and consolidation were more prevalent than cavity or pneumatocele, pleural effusion, bronchiectasis, and lymphadenopathy. Most COVID-19-positive children exhibit only mild CT findings, and given the potential risk of radiation exposure, CT imaging results may not significantly impact treatment decisions. Therefore, CT scans may not be necessary for most patients and may be replaced by CXR, except for individual cases.