1. Background
Influenza viruses, belonging to the Orthomyxoviridae family, are significant pathogens responsible for seasonal, chronic, and epidemic diseases through infection of the upper respiratory tract, including the trachea and bronchioles (1). In December 2019, Wuhan, the capital of China's Hubei province, became the center of an outbreak of pneumonia of unknown origin. On January 7, 2020, Chinese scientists isolated a novel coronavirus, later named severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2, formerly known as 2019-nCoV), from a patient with pneumonia (2). In February 2020, the virus was officially named coronavirus disease 2019 (COVID-19) by the WHO (3). The clinical spectrum of SARS-CoV-2 infection is broad, ranging from asymptomatic infection to upper respiratory tract infection, severe viral pneumonia with respiratory failure, and even death. Many patients with pneumonia were hospitalized in Wuhan during the early outbreak (4).
CT imaging of patients with pneumonia reveals reticular opacities, with or without areas of consolidation, predominantly in the lower lobes. Poorly defined areas, including regions of rapid resolution or nodules indicating extensive alveolar damage, may resolve within approximately three weeks (5). Ground-glass opacities (GGOs) are the most common finding in COVID-19 pneumonia. These opacities are often multiple, lateral, and peripheral, although in the early stages, they may present as unifocal lesions, particularly in the lower lobes (6).
In COVID-19, initial CT findings often include two-dimensional GGO, primarily affecting the lower lobes, with less involvement in the middle regions. These findings are typically distributed posteriorly (5). However, the CT imaging patterns of COVID-19 overlap significantly with those of other viral pneumonias (7).
A study by Amorim et al. (8) on H1N1 infections confirmed that the most common CT findings were GGO (85%), consolidation (64%), and the coexistence of both opacities (58%). Koo et al. (9) reported that the most common findings in CT scans of pneumonia included bilateral nodular reticular opacities, with or without areas of consolidation, primarily in the lower lungs. Similarly, Shim et al. (10) examined CT images of 21 patients with influenza A (H1N1) pneumonia and found that GGO were present in 95% of cases. Lomoro et al. (11) noted that the typical CT findings in COVID-19 pneumonia include bilateral and multilobular GGO, accompanied by consolidation in 60% of cases and without consolidation in 36% of cases.
A study by Bernheim et al. (12) on CT findings in COVID-19 patients revealed that 56% of patients showed no abnormalities on initial CT scans conducted within 0 - 2 days of symptom onset. Over time, CT findings evolved to include bilateral and unilateral involvement, linear opacities, crazy-paving patterns, and halo signs. The literature highlights substantial overlap in chest CT patterns between COVID-19 and other viral pneumonias. Consequently, comparing CT scans of these infections can help identify overlapping patterns as well as unique features.
2. Objectives
This study aimed to compare chest CT findings between two groups: Patients with influenza and those with COVID-19, to identify distinguishing and overlapping imaging features.
3. Methods
This analytical-descriptive cross-sectional study analyzed the medical records and CT scans of patients diagnosed with influenza or COVID-19 who were admitted to Bu-Ali Zahedan Hospital from autumn 2019 to June 2020. Patients with tuberculosis or bacterial pneumonia were excluded from the study. Based on the number of patients available during the study period, the sample size was determined to be 114, comprising 57 patients with influenza and 57 patients with COVID-19, selected using a simple random sampling method.
3.1. Procedure
This study was conducted with the approval of the Ethics Committee under the methodology IR.ZAUMS.REC.1400.330. After receiving approval, coordination was established with the radiology department and the medical records unit of Bu-Ali Hospital in Zahedan, Iran.
Two groups of patients were included: Those diagnosed with influenza and those with confirmed COVID-19 infection verified by a positive PCR test. Patients' CT scans were accessed through the PACS system by entering their file numbers.
All CT scans of patients with pulmonary embolism referred to Bu-Ali Hospital in the fall of 2019 were reviewed by a radiologist and documented in a report form. The data collected included age, sex, lesion distribution, type of opacification, unilateral or bilateral involvement, site of involvement, presence of bronchiectasis, interlobular and intralobular septal thickening, pleural effusion, consolidation, cavities, lymphadenopathy, crazy-paving appearance, and vascular dilation. The same radiologist also reviewed and documented CT scan findings for patients with confirmed COVID-19 from March 2019 to June 2020. The information was entered into a standardized data form. The frequencies of various patterns and results in each group were recorded and analyzed using statistical software.
3.2. Statistical Analysis
After data collection, the raw data were imported into SPSS version 26 for analysis. Frequency and percentage were used to present qualitative data, while quantitative data were described using mean and standard deviation. For comparing the means of measured variables (continuous data) between the two groups, the independent t-test was used when the assumptions of parametric tests were met. If these assumptions were not satisfied, non-parametric tests such as the Mann-Whitney test were applied. To compare proportions (frequencies) between groups, either Fisher's exact test or the chi-square test was used. A P-value of < 0.05 was considered statistically significant for all analyses.
4. Results
A total of 114 patients participated in this study, comprising 56 men (49.12%) and 58 women (50.88%), with a mean age of 53.24 ± 11.99 years. The youngest participant was 24 years old, and the oldest was 74 years old. Among the COVID-19 patients, there were 27 men (47.37%) and 30 women (52.63%), while the influenza group included 29 men (50.88%) and 28 women (49.12%). Table 1 presents the frequency of unilateral and bilateral lung involvement observed in CT scans for patients with COVID-19 and influenza. In the COVID-19 group, 9 patients (15.79%) exhibited unilateral lung involvement, while 48 patients (84.21%) showed bilateral involvement. Similarly, in the influenza group, 10 patients (17.54%) displayed unilateral involvement, whereas 47 patients (82.46%) had bilateral involvement. Across both groups, a total of 19 patients (16.67%) demonstrated unilateral involvement, while 95 patients (83.33%) exhibited bilateral involvement. The comparison between the two groups reveals no statistically significant difference in the distribution of unilateral or bilateral lung involvement (P-value = 0.802). Bilateral involvement was the predominant pattern in both COVID-19 and influenza patients.
| Groups | Type of Affection | P-Value | |
|---|---|---|---|
| Unilateral | Bilateral | ||
| COVID-19 | 9 (1.79) | 48 (84.21) | 0.802 |
| Influenza | 10 (17.54) | 47 (82.46) | |
| Total | 19 (16.67) | 95 (83.33) | |
a Values are expressed as No. (%).
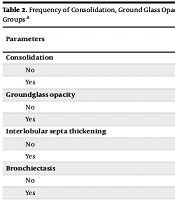
Table 2 presents the frequency of CT scan findings in COVID-19 and influenza patients. The analysis revealed significant differences in some imaging characteristics between the two groups. Consolidation was observed in 27 patients (47.37%) in the COVID-19 group and in 38 patients (66.67%) in the influenza group, totaling 65 patients across both groups. The P-value of 0.037 indicates that consolidation is significantly more common in influenza patients compared to those with COVID-19. Ground-glass opacity showed notable differences between the groups, with 40 patients (70.18%) in the COVID-19 group exhibiting GGO compared to 29 patients (50.88%) in the influenza group. This finding, with a total of 69 patients and a P-value of 0.035, demonstrates that GGO is significantly more prevalent in COVID-19 patients than in influenza patients.
| Parameters | Studied Group | P-Value | |||
|---|---|---|---|---|---|
| COVID-19 | Influenza | Total | |||
| Consolidation | 0.037 | ||||
| No | 30 (52.63) | 19 (33.33) | 49 (42.98) | ||
| Yes | 27 (47.37) | 38 (66.67) | 65 (57.02) | ||
| Groundglass opacity | 0.035 | ||||
| No | 17 (29.82) | 28 (49.12) | 45 (39.47) | ||
| Yes | 40 (70.18) | 29 (50.88) | 69 (60.53) | ||
| Interlobular septa thickening | 0.032 | ||||
| No | 31 (54.39) | 42 (73.68) | 73 (64.04) | ||
| Yes | 26 (45.61) | 15 (26.42) | 41 (35.96) | ||
| Bronchiectasis | 0.242 | ||||
| No | 55 (96.49) | 52 (91.23) | 107 (93.86) | ||
| Yes | 2 (3.51) | 5 (8.77) | 7 (6.14) | ||
| Pleural efconfluent | 0.002 | ||||
| No | 55 (96.49) | 44 (77.19) | 99 (86.84) | ||
| Yes | 2 (3.51) | 13 (22.81) | 15 (13.16) | ||
| Cavity/pneumatocele | 0.026 | ||||
| No | 55 (96.49) | 48 (84.21) | 103 (90.35) | ||
| Yes | 2 (3.51) | 9 (15.79) | 11 (9.65) | ||
| Lymphadenopathy | 0.012 | ||||
| No | 57 (100) | 51 (89.47) | 108 (94.74) | ||
| Yes | 0 (0) | 6 (10.53) | 6 (5.26) | ||
| Crazy paving pattern | 0.026 | ||||
| No | 39 (68.42) | 49 (85.96) | 88 (77.19) | ||
| Yes | 18 (31.58) | 8 (14.04) | 26 (22.81) | ||
| Vascular dilatation | 0.011 | ||||
| No | 36 (63.16) | 48 (84.21) | 84 (73.68) | ||
| Yes | 21 (36.84) | 9 (15.79) | 30 (26.32) | ||
| Distribution of the lesion | 0.059 | ||||
| No | 37 (64.91) | 27 (47.37) | 64 (56.14) | ||
| Yes | 20 (35.09) | 30 (52.63) | 50 (43.86) | ||
a Values are expressed as No. (%).
Interlobular septal thickening was identified in 26 patients (45.61%) with COVID-19 and 15 patients (26.42%) with influenza, totaling 41 cases. The P-value of 0.032 suggests that interlobular septal thickening is more common in COVID-19 patients than in those with influenza.
Bronchiectasis was observed in 2 patients (3.51%) in the COVID-19 group and 5 patients (8.77%) in the influenza group, totaling 7 patients. The P-value of 0.242 indicates no significant difference, suggesting similar rates of bronchiectasis in both groups.
Pleural effusion was noted in 2 patients (3.51%) in the COVID-19 group and 13 patients (22.81%) in the influenza group, with a total of 15 cases. A highly significant P-value of 0.002 highlights that pleural effusion is much more prevalent in influenza patients than in COVID-19 patients.
Cavities or pneumatocele were found in 2 patients (3.51%) in the COVID-19 group and 9 patients (15.79%) in the influenza group, totaling 11 cases. The P-value of 0.026 indicates that cavities or pneumatocele are significantly more common in influenza patients than in COVID-19 patients.
Lymphadenopathy was observed in 6 patients (10.53%) in the influenza group, while no cases were noted in the COVID-19 group. The P-value of 0.012 underscores a statistically significant difference, with lymphadenopathy being more frequent in influenza patients.
Finally, the crazy paving pattern was reported in 18 patients (31.58%) in the COVID-19 group and 8 patients (14.04%) in the influenza group, suggesting this pattern is more prevalent in COVID-19 patients. This resulted in a total of 26 patients and a P-value of 0.026, indicating that the crazy paving pattern is significantly more prevalent in patients with COVID-19. Vascular dilatation was identified in 21 patients (36.84%) in the COVID-19 group compared to 9 patients (15.79%) in the influenza group. With a total of 30 affected patients and a P-value of 0.011, these findings demonstrate that vascular dilatation is notably more common in COVID-19 patients than in those with influenza.
The distribution of lesions was observed in 20 patients (35.09%) in the COVID-19 group and 30 patients (52.63%) in the influenza group, totaling 50 patients. Although the P-value was not provided, the findings suggest that lesion distribution is more frequently observed among patients with influenza compared to those with COVID-19.
Overall, these findings underscore distinct differences in the frequency of various CT scan parameters between COVID-19 and influenza patients. Certain features, such as the crazy paving pattern and vascular dilatation, appear more characteristic of COVID-19, while consolidation, pleural effusion, and lesion distribution are more common in influenza. These differences can aid in distinguishing between the two conditions when considered alongside clinical and laboratory data.
5. Discussion
The study included 114 patients with a nearly balanced gender distribution (49.12% men and 50.88% women) and a mean age of 53.24 years. This demographic aligns with previous studies where age and gender did not significantly differ between COVID-19 and influenza patients (13, 14). Specifically, our findings showed no significant difference in gender (P = 0.708) or age (P = 0.610) between the two groups, consistent with the results of Altmayer et al. (15) and Zarei et al. (16).
In terms of CT imaging characteristics, our findings revealed that among COVID-19 patients, bilateral involvement was observed in 84.21%, while unilateral involvement was present in only 15.79%. This supports the notion that bilateral lesions are indicative of COVID-19 pneumonia. Regarding the types of opacities observed, 32.46% of COVID-19 patients exhibited opacity and combined types, while 33.33% of influenza patients presented with GGO. These findings are consistent with Altmayer et al. (15), who reported mixed patterns of GGO and consolidation, with GGO being the predominant feature in COVID-19 cases, suggesting that GGO may serve as a key imaging feature for identifying COVID-19 pneumonia.
Furthermore, the comparison of peripheral versus central involvement revealed no significant difference (P = 0.059) between COVID-19 and influenza patients in our study, indicating that both conditions may present with similar central or peripheral distribution patterns. This finding contrasts with Altmayer et al.'s (15) report of a more pronounced peripheral distribution in COVID-19 patients (77%), suggesting that regional variations in CT findings among different populations or disease stages warrant further investigation.
Statistical comparisons of coexisting opacities, specifically the presence of GGO and consolidation, showed no significant differences (P = 0.841) between the two groups.
This suggests that while CT imaging can provide valuable insights into the presence and type of pneumonia, it may not always yield definitive differentiators between COVID-19 and influenza in certain populations. Influenza viruses are major pathogens causing upper respiratory tract infections, including seasonal and primary bronchitis, as well as chronic and epidemic diseases. While most infections are mild and confined to the upper respiratory tract, severe complications such as hemorrhagic bronchitis and fulminant pneumonia, whether primary viral or secondary bacterial, can arise in individuals with chronic conditions, the elderly, and infants (5, 8, 12-15, 17). The clinical symptoms and CT imaging features of influenza and COVID-19 often overlap, making differentiation challenging. There were no significant differences between the two groups regarding the distribution of lesions (peripheral vs. central), the number of lesions, or the presence of bronchiectasis or GGO, which may limit their diagnostic value.
Similar to prior studies (8-11), the most common CT findings in both groups were GGO and confluent lesions. Radiological analysis of 81 COVID-19 pneumonia patients conducted by Shi et al. (18) demonstrated that bilateral diffuse GGO were the most frequent abnormalities on chest CT scans, especially during the 1 - 3 weeks following onset. In contrast, studies examining H1N1 pneumonia found that consolidation was the dominant feature in hospitalized patients rather than GGO (19, 20). Although less common, certain CT features may still provide valuable clues for distinguishing between the two infections. Consistent with Yang et al.'s findings (14), our study also noted that interlobular septal thickening, crazy-paving patterns, lymphadenopathy, and pleural effusion occurred more frequently in influenza patients than in COVID-19 patients. While bronchiectasis showed no significant difference between the two groups, Zarei et al. (16) reported that bronchiectasis is often associated with respiratory diseases and vasodilation in COVID-19 patients. Furthermore, although reverse transcription polymerase chain reaction (RT-PCR) is a widely used and validated method for diagnosing COVID-19, it is not immune to false-negative results due to various factors (17). Therefore, CT findings in patients who are highly suspected of having COVID-19 but test negative with RT-PCR can serve as crucial diagnostic guidelines (13-15).
Influenza viruses are significant pathogens that cause upper respiratory tract diseases, such as seasonal bronchiectasis and primary bronchitis, as well as seasonal, chronic, and epidemic illnesses. However, serious complications of influenza A, including hemorrhagic bronchitis or fulminant pneumonia (primary viral or secondary bacterial), occur in individuals with chronic illnesses, the elderly, and infants. The clinical course and CT manifestations of influenza and COVID-19 may be similar. Therefore, this study examined the CT scans of two groups of patients to differentiate between these diseases.
In many cases of viral pneumonia, a CT scan alone cannot distinguish between different disease types. Therefore, clinical and laboratory signs and methods should always be used in conjunction with CT findings to increase diagnostic accuracy. As a result, ground-glass opacity, interlobular septal thickening, occurrence of crazy paving patterns, and vasodilation were significantly more frequent in patients with COVID-19 compared to patients with influenza. Congestion, inflammation, cavitation or emphysema, and lymphadenopathy were more common in patients with influenza pneumonia.
By focusing on the type of admission and the specific CT characteristics, a more accurate diagnosis can be made when the initial diagnosis is unclear. The peripheral or central distribution of lesions, the number of lesions, and the presence of bronchiectasis, GGO, and consolidation were not significantly different between the two groups of patients, reducing their diagnostic value in some cases.
In our study, GGO and consolidation were the most common CT findings in patients, consistent with previous findings (8-11). However, this study found that patients with COVID-19 had a higher prevalence of GGO compared to patients with influenza, aligning with the findings of Zarei et al. (16). Ground-glass opacity was more prominent in patients with COVID-19 than in those with H1N1, whereas consolidation was more pronounced in patients with H1N1, consistent with previous studies.
Radiological findings of 81 patients with COVID-19 pneumonia reported by Shi et al. (18) showed that bilateral diffuse GGO were the most common pattern of abnormalities on chest CT scans during the 1 - 3 weeks following disease onset. Studies of H1N1-related pneumonia have shown consolidation on CT images without GGO in hospitalized patients (19, 20). Pathological findings, including alveolar rupture indicating ARDS, fibromucinous exudate in COVID-19, necrotizing bronchitis, and severe hemorrhage in H1N1 pneumonia, may account for the specific imaging features observed during the disease. These pathological differences help explain variations in radiological presentation. While rare, certain CT scan findings can provide additional insights to differentiate these diseases. Similar to the study by Yang et al. (14), interlobular septal thickening, crazy paving patterns, lymphadenopathy, and pleural effusion were more frequently observed in patients with influenza compared to those with COVID-19.
Zarei et al. (16) found no significant differences in the incidence of bronchiectasis between the two groups. However, bronchiectasis was often associated with respiratory illnesses and vasodilation in COVID-19 patients. These findings underscore the complexity of diagnosing COVID-19 and influenza based solely on imaging. Distinct patterns, such as bilateral distribution and the prevalence of GGO in COVID-19, highlight potential differentiating features. However, the overlap in imaging characteristics between the two diseases emphasizes the importance of integrating clinical history, imaging findings, and laboratory results to achieve an accurate diagnosis. Future research should focus on exploring these imaging patterns in larger and more diverse populations to further elucidate the diagnostic role of imaging in viral pneumonia. Such studies can contribute to refining diagnostic protocols and improving differentiation between COVID-19 and influenza in clinical practice.
5.1. Conclusions
This study highlighted the distinct and overlapping CT imaging features of COVID-19 and influenza pneumonia. While bilateral lung involvement was predominant in both groups, significant differences were identified in specific imaging characteristics. COVID-19 patients demonstrated higher frequencies of GGO, interlobular septal thickening, crazy-paving patterns, and vascular dilatation, whereas consolidation, pleural effusion, cavitation, and lymphadenopathy were more common among influenza patients. These findings emphasize the importance of integrating clinical evaluations and laboratory results with imaging studies to improve diagnostic accuracy, given the considerable overlap in clinical presentations of the two infections. Although certain CT features may assist in differentiation, imaging alone is insufficient for a definitive diagnosis. Future research involving larger and more diverse populations is essential to further explore these patterns, refine diagnostic protocols, and enhance outcomes in managing viral pneumonia.