1. Background
The novel coronavirus disease (COVID-19) caused by the SARS-CoV-2 virus started to spread across the globe from China in December 2019, resulting in more than 21.1 million confirmed infections and more than 761 000 deaths worldwide as of August 17, 2021 (1). Despite strict measures to contain the spread of the virus, the disease continues to ravage the world, overwhelm hospital resources, and exhaust health personnel. The most common symptoms of COVID-19 include fever, cough, fatigue, dyspnea, and sputum production. The SARS-CoV-2 virus has variably affected different populations in the world (2). In this regard, older people and those suffering from comorbidities such as cardiovascular diseases (CVDs), diabetes, and pulmonary disease are more vulnerable and likely to develop severe disease (3).
Multiple research efforts have been made to determine the risk and vulnerability factors for severe COVID-19, which has important clinical implications in terms of triage and prognosis. So far, several population-based studies have identified patient-related risk factors that can predict poor outcomes in COVID-19, including gender, race, ethnicity, age, obesity, and preexisting medical conditions (4). Recent studies have investigated the association between ABO blood group type and the risk of contracting COVID-19 (5, 6). The blood group has been identified as a risk factor in many diseases, including CVDs, gastrointestinal diseases, dementia, cancer, and diabetes; however, most of these studies have been focused on infectious diseases (7). Blood group antigens play a direct role in infections through various mechanisms. At the molecular level, blood group antigens can act as main receptors for pathogens and facilitators for the cellular uptake of viral particles (8). Blood groups have been noted to be clinically associated with bacterial, parasitic, and viral infections (9, 10). There are also studies indicating that blood groups can affect susceptibility to certain viruses such as SARS-CoV-1 and norovirus. Accordingly, ABO antigens comprise the main blood group system and express not only on the surface of red blood cells but also on the surface of other cells in the body. These antigens are made of polysaccharides mimicking the structure of the polysaccharides present in some bacteria, so they may directly or indirectly enhance or weaken the function of the immune system. Zhao et al. described that blood group A could be associated with a higher risk of contraction and death due to COVID-19, while blood group O was associated with a lower risk of infection and mortality (11). Also, Zietz et al. found that blood group A was associated with a higher chance of testing positive for COVID-19 (12). A meta-analysis study in 2012 demonstrated that non-O blood groups were among the most important genetic risk factors for venous thromboembolism (13). Coagulopathy has been reported to be a common problem in patients with COVID-19 (14, 15), requiring strict risk management for venous thromboembolism in this condition. However, there are also negative relationships between blood group and infections with SARS-CoV-2 (16-19).
2. Objectives
Considering that the results of studies are contradictory, the present research was conducted to investigate the relationship between ABO blood groups and the mortality rate, disease severity, and length of hospitalization (LOH) in patients with COVID-19.
3. Methods
This study was a cross-sectional, multi-center analysis of adult patients with COVID-19 hospitalized in two hospitals (Shahid Beheshti Hospital of Shiraz and Shariati Hospital of Isfahan) from March 1 to June 1, 2020. Written informed consent was obtained from all participants or their caregivers before data collection. All patients who tested positive for COVID-19 (based on the nasopharyngeal reverse transcriptase polymerase chain reaction method) and whose blood groups were recorded in their profiles were included in the study. We excluded those without a documented ABO blood group and younger than 18 years old. Demographic data (age, sex), comorbidities, disease severity (hospitalization in general ward or intensive unit care (ICU), LOH (number of inpatient days spent in ICU and/or skilled care setting over the study period), and disease outcomes (i.e., neuronal, gastrointestinal, or cardiac involvement) were recorded. The LOH was defined as the total number of days of admission during the study period. Death was recorded when the patient passed away during the study period. Severe disease was regarded for ICU admission and/or death. The accuracy of data was carefully evaluated by healthcare staff working in the mentioned hospitals and the research team prior to analysis. Those who were involved in data gathering did not perform data analysis.
This study was approved by the Research Ethics Committee of Islamic Azad University, Najaf Abad Branch, and informed written consent was obtained from all participants. The study protocol was in accordance with the Declaration of Helsinki (1975) and its amendments in 2008. The history of diseases such as hypertension, hyperlipidemia, CVDs, diabetes mellitus, and cancer was questioned. The serum levels of creatinine, blood urea nitrogen (BUN), C-reactive protein (CRP), erythrocyte sedimentation rate (ESR), lactate dehydrogenase (LDH), alanine transaminase (ALT), and aspartate aminotransferase (AST), as well as white blood cell count (WBC), were recorded.
3.1. Statistical Analysis
All data were analyzed with SPSS version 24 software. The frequencies of various blood groups, as the main independent variable, were described in different study groups. The patients’ demographic and clinical characteristics were presented using descriptive statistics. The normality of data was assessed, and non-parametric tests were used for data analysis. The chi-square test was used to analyze qualitative variables, and ANOVA or the Kruskal-Wallis test was used to compare quantitative variables between study groups. Odds ratios (ORs) for ABO blood groups were determined by logistic regression and adjusted for age, gender, the presence of comorbidities (diabetes, CVDs, and history of cancer), and Rh status. All tests were performed at the error level of 5% as the statistical significance cut-off.
4. Results
During the study period, the data of 398 patients admitted to two hospitals due to COVID-19 infection were analyzed. Patients’ demographic characteristics, comorbidities, and the results of laboratory tests have been presented in Table 1. Of the patients, 238 (59.8%) were men; 17 (4.3%) were admitted to the ICU, and 89 (22.4%) died of the disease. Also, 124 (31.2%) patients had diabetes, 165 (41.5%) had CVDs, and 30 (7.5%) of them had cancer. Out of 398 patients who were positive for COVID-19, 65 (16.3%), 71 (17.8%), 9 (2.3%), and 252 (63.3%) had blood groups of A, B, AB, and O, respectively, and 385 (96.7%) were Rh-positive. The mean values of ALT, AST, LDH, BUN, creatinine, ESR, CRP, and WBC did not differ significantly between patients with different blood groups (Table 1).
| Variables | Blood Group A | Blood Group B | Blood Group AB | Blood Group O | P-Value |
|---|---|---|---|---|---|
| Age, mean ± SD | 59.43 ± 17.75 | 60.70 ± 17.90 | 58.77 ± 12.36 | 58.65 ± 17.86 | 0.921 |
| Rh-positive | 62 (95.4) | 69 (97.2) | 8 (88.9) | 245 (97.2) | 0.502 |
| Female sex | 20 (30.8) | 28 (39.4) | 5 (55.6) | 106 (42.1) | 0.291 |
| DM | 21 (32.3) | 20 (28.2) | 2 (22.2) | 81 (32.1) | 0.854 |
| CVD | 23 (35.4) | 34 (47.9) | 3 (33.3) | 105 (41.7) | 0.486 |
| CA | 7 (10.8) | 8 (11.3) | 1 (11.1) | 14 (5.6) | 0.270 |
| ALT | 43.77 ± 33.39 | 49.19 ± 36.03 | 36.77 ± 30.13 | 44.65 ± 19.47 | 0.559 |
| AST | 55.54 ± 36.93 | 48.91 ± 25.11 | 42.77 ± 25.08 | 47.64 ± 17.12 | 0.600 |
| LDH | 685.80 ± 327.43 | 696.43 ±351.85 | 623.11 ± 274.75 | 640.65 ± 389.12 | 0.565 |
| BUN | 20.35 ± 16.22 | 19.13 ± 11.66 | 19.77 ± 11.87 | 17.71 ± 13.54 | 0.668 |
| Cr | 1.60 ± 1.07 | 1.51 ± 0.61 | 1.45 ± 1.07 | 1.64 ± 0.27 | 0.963 |
| CRP | 48.88 ± 28.67 | 42.04 ± 23.38 | 51.33 ± 26.72 | 46.77 ± 31.07 | 0.674 |
| ESR | 7253.84 ± 4441.25 | 8321.12 ± 5414.81 | 10900.00 ± 5167.84 | 7570.59 ± 5950.84 | 0.108 |
| WBC | 78.18 ± 41.27 | 64.49 ± 42.77 | 79.77 ± 41.47 | 67.51 ± 38.94 | 0.187 |
Abbreviations: SD, standard deviation; DM, diabetes mellitus; CVD, cardiovascular diseases, CA, cancer; ALT, alanine transaminase; AST, aspartate aminotransferase; LDH, lactate dehydrogenase; BUN, blood urea nitrogen; Cr, creatinine; ESR, erythrocyte sedimentation rate; WBC, white blood cells.
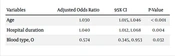
Multivariate analysis showed that for each day of hospitalization, the odds of death increased by 4% (OR = 1.04, P = 0.004). Also, the chance of death was 43% lower in patients with blood group O than those with other blood groups (OR = 0.574, P = 0.032) (Table 2). In patients with blood group A, the chance of hospitalization at the ICU was five times higher than in patients with other blood groups (OR = 5.038, P = 0.002) (Table 3). The LOH was 5.437 and 2.6 days shorter in Rh-positive patients and those with blood group B, while patients with blood group A were hospitalized 3.7 days longer than individuals with other blood groups (Table 4).
| Variables | Adjusted Odds Ratio | 95% CI | P-Value |
|---|---|---|---|
| Age | 1.030 | 1.015, 1.046 | < 0.001 |
| Hospital duration | 1.040 | 1.012, 1.068 | 0.004 |
| Blood type, O | 0.574 | 0.345, 0.953 | 0.032 |
| Variable | Adjusted Odds Ratio | 95% CI | P-Value |
|---|---|---|---|
| Blood type A | 5.038 | 1.849, 13.732 | 0.003 |
| Variables | B | 95% CI | P-Value |
|---|---|---|---|
| Rhesus factor | - 5.437 | - 10.089, - 0.784 | 0.022 |
| Blood type A | 3.692 | 1.370, 6.014 | 0.002 |
| Blood type, B | - 2.967 | - 4.923, - 0.471 | 0.018 |
5. Discussion
In the present study, we assessed the effects of ABO blood groups on the outcome, disease severity, and LOH in patients infected with the SARS-CoV-2. We observed the lowest chance of death in patients with blood group O compared to those with other blood groups. In addition, patients with blood group A had the highest probability of ICU admission and a longer hospital stay compared to people with other blood groups. Also, positivity for Rh was associated with a shorter hospitalization period.
Genetic factors play an important role in the development of various diseases. Accordingly, ABO blood groups, as a genetic factor, have been widely studied for their roles in the pathogenesis of infectious diseases (20-22). After the onset of the recent coronavirus pandemic, several studies were conducted on the relationship between ABO blood groups and COVID-19 (11, 23, 24). Most of these studies showed that among infected people, the proportion of patients with blood group A was relatively high, while the ratio of patients with blood group O was low. In comparison with studies on the link between blood groups and susceptibility to COVID-19, fewer studies have been conducted on the relationship between blood groups and mortality, disease severity, and LOH in these patients. In a meta-analysis of 10 studies by Liu et al., only five studies investigated the association between ABO blood groups and COVID-19-related mortality (25). This meta-analysis stated that blood group A was associated with a significant increase in the risk of mortality compared to other blood groups, which is in agreement with the results of the present study. Another study also showed that the risk of mortality due to COVID-19 was significantly higher in patients with blood group A and lower in those with blood group O compared to individuals with other blood groups (26). Nevertheless, there are also studies stating no relationship between ABO blood groups and mortality in COVID-19 patients (27, 28).
Our study revealed a significant relationship between blood group A and the severity of COVID-19 (as defined by admission to the ICU). In line, Halim et al. reported that disease severity, as well as COVID-19 complications and mortality, were significantly higher in patients with blood group A than those with non-A blood groups (29). In a study by Almadhi et al. on 2 334 COVID-19 patients, no association was found between blood groups and disease severity (30). Likewise, Rana et al. discovered no relationship between blood groups and susceptibility to severe COVID-19 (28).
In the present study, the LOH was significantly longer in COVID-19 patients with blood group A than in patients with non-A blood groups. Also, Rh positivity was associated with a significant decrease in the number of hospitalization days, which was similar to the results of Rana et al. (28). In contrast, Gursoy and Avci identified no relationship between blood groups and hospitalization length (31). Regarding the fact that negative Rh represented nearly 3% of individuals in our data, our results should be interpreted with caution. Our literature search revealed that studies on the relationship between the length of the recovery period and blood groups are rare. In one study by Esref et al., Rh positivity was significantly more prevalent among COVID-19 patients (32), while no significant difference was observed in another study by Solmaz (27).
Various mechanisms have been proposed to explain the poorer prognosis of COVID-19 patients with blood group A. The activity of angiotensin-converting enzyme-1 (ACE-1) is higher in people with blood group A, rendering them more prone to cardiovascular complications and severe COVID-19. Also, people with blood type A have elevated levels of Von Willebrand factor (VWF) and factor VIII, boosting the risk of thromboembolic events in those contracting COVID-19 (33). On the other hand, the higher prevalence of some viral infections in Rh-negative people is probably due to the variable expression of glycosylated structures on the surface of red blood cells, acting as common receptors/co-receptors and facilitating the binding of viruses (34).
One of the strengths of this study was the inclusion of laboratory findings in data analysis and adjusting the effects of possible confounding factors in multivariate analysis. However, our results may be restricted by the fact that this study had a retrospective observational design and a relatively small sample size.
5.1. Conclusions
Our study showed that the severity of COVID-19 and the duration of hospitalization were higher in patients with blood group A compared to individuals with other blood groups. Also, blood group O was associated with a lower mortality rate, and Rh positivity predicted a shorter hospitalization period. However, larger multicenter studies are required to verify the association between blood groups and SARS-CoV-2 infection.