1. Background
One of the most common operations in children is tonsillectomy. It is performed in about 500,000 pediatric patients yearly in the United States alone (1). The most common indication for this surgery is sleep disorder breathing (2). In addition, adenoidectomy is considered another one of the most common surgeries in pediatrics by otolaryngologists currently (3). It is conducted for various indications, although the most common one is recurrent upper airway infections (4). Additionally, there is a large variation in surgical rates all over the world (5). All of these diseases, in addition to healthcare, are affected in different aspects by the coronavirus disease 2019 (COVID-19) pandemic (6).
The coronavirus pandemic (COVID-19) has led to long-lasting and monumental changes in individuals’ lives due to the recommendations and restrictions to avoid the spread of this disease. One of the most common strategies was social distancing and lockdowns, which affected the number of various surgeries (7). For example, Haapanen et al.’s study (8) in 2021 in Finland reported that the restrictions during COVID-19 decreased the rates of tonsillectomies and tympanostomies in pediatrics. In addition, the lockdown and cancellation of elective surgeries during the pandemic increased (8).
However, there is no other study about the evaluation of incidence rates of tonsillectomy (TO), adenoidectomy (AD), and ear surgeries before and during the COVID-19 pandemic in the world, particularly in Iran. Additionally, there is no study about the impact of the COVID-19 pandemic peaks on the incidence rates of these operations.
2. Objectives
This study aimed as the first study to determine the impact of the COVID-19 pandemic and its peaks separately on the incidence rates of most common pediatric surgeries, such as tonsillectomy and adenoidectomy in the pediatric population, and ear surgeries in any age, in Iran.
3. Methods
This retrospective register study was performed in a referral university hospital (Amir A’lam hospital) in Tehran, Iran. This hospital is the most well-known referral and equipped center for all types of otolaryngological surgeries in Iran. The data collection of target patients within March 21, 2018, to November 22, 2021, was performed using the Health Information System (HIS). This 4-year period was classified based on the months of the year in Iran; therefore, a year was considered within April to April of the next year. It means that 1st year was considered within April 2018 to April 2019, 2nd year was considered within April 2019 to April 2020, 3rd year was considered within April 2020 to April 2021, and 4th year was considered within April 2021 to November 2021. The reason is that it was intended to adjust the time of each peak in Iran. It is noteworthy to mention that the COVID-19 pandemic started in February 2020 in Iran, although the first peak was in March 2020. Therefore, there were approximately 1st and 2nd years as before COVID-19 and 3rd and 4th years as after the COVID-19 pandemic started. No ethics committee approval was obtained due to the retrospective register-based study design, in which the patients are not contacted. However, institutional permissions from chief doctors of the hospital to access the register data were obtained.
A custom checklist was created by investigators that specifically focused on some operations, such as partial and complete tonsillectomies, adenoidectomy, and oto-surgeries, including tympanoplasty, tympanomastoidectomy, middle ear exploration, and ossiculoplasty. Patients of all ages who underwent any of the aforementioned operations were included. In addition, the age and gender information of each patient was collected. Then, the frequency of operations based on the type of operation, monthly and yearly, was calculated. Additionally, the exact time of any peak of the COVID-19 pandemic in Iran was extracted from the World Health Organization (WHO) website, and the number of surgeries during the period of any peak in addition to before and during the COVID-19 pandemic was determined. Finally, the number of operations was compared between different periods.
All the data were analyzed using IBM SPSS statistics for Windows (version 26.0). Descriptive variables were reported as mean, standard deviation (SD), and frequency. The chi-square, analysis of variance (ANOVA), post-hoc, and t-test were performed to compare the data between different variables. In addition, a P-value less than 0.05 was considered statistically significant.
4. Results
In total, 6290 patients were enrolled in this study. Out of these participants, 52.9% (n = 3328) and 46.5% (n = 2923) were male and female, respectively, and 0.6% (n = 39) were missing data. There were 3 types of surgeries, such as AD, TO, and ear surgeries, with mean ± SD age of 10.20 ± 9.4, 11.45 ± 10.8, and 44.19 ± 14.6 years, respectively. The baseline characteristics of these groups are summarized in Table 1.
| Variables | Adenoidectomy | Tonsillectomy | Oto-surgery |
|---|---|---|---|
| Gender | |||
| M | 93 (60) | 2438 (57) | 797 (43.1) |
| F | 62 (40) | 1819 (42.4) | 1042 (56.2) |
| Missing | - | 25 (0.6) | 14 (0.7) |
| Age | |||
| Valid | 10.20 ± 9.41 | 11.45 ± 10.843 | 44.19 ± 14.656 |
| Missing | - | N = 456 | N = 124 |
| Year | |||
| 1st | 60 (2.4) | 1891 (75.9) | 542 (21.7) |
| 2nd | 74 (2.9) | 1845 (71.6) | 658 (25.5) |
| 3rd | 18 (2.3) | 315 (41.1) | 433 (56.5) |
| 4th | 3 (0.7) | 231 (50.9) | 220 (48.5) |
| COVID-19 | |||
| Before | 134 (86.4) | 3736 (87.2) | 1200 (64.8) |
| After | 21 (13.6) | 546 (12.8) | 653 (35.2) |
Abbreviations: M, male; F, female; COVID-19, coronavirus disease 2019.
a Values are presented as mean ± SD or No. (%).
Additionally, the number of cases before and after the COVID-19 pandemic and yearly are separately summarized in Table 1 based on the type of surgery. The adenoidectomy, tonsillectomy, and oto-surgery groups included 2.5% (n = 155), 68% (n = 4282), and 29.5% (n = 1853) of cases, respectively. The total number of surgeries in 1st, 2nd, 3rd, and 4th were 39.6% (n = 2493), 41.0% (n = 2577), 12.2% (n = 766), and 7.2% (n = 454), respectively. There was a significant difference in terms of the total number of operations and the number of each type of surgery between before and after the COVID-19 pandemic (P < 0.001). Additionally, the frequency of age, gender, and number of operations are shown in Figures 1 , 2, and 3 based on each type of surgery separately.
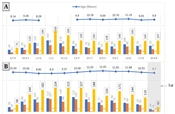
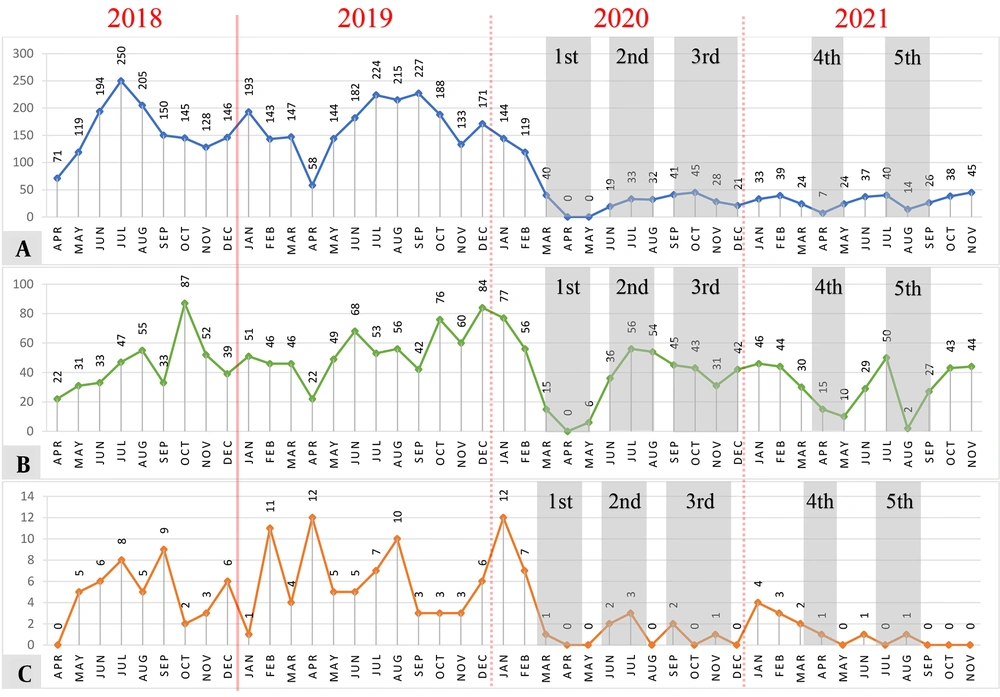
Monthly frequency of age, gender, and number of operations for adenoidectomy based on 1st, 2nd, 3rd, and 4th years. (A: 1st year; B: 2nd year; C: 3rd year; D: 4th year). A and B are related to ‘before COVID-19', and C and D are related to 'during COVID-19’. Each gray highlighted area presents one peak that is shown by the arrow and the number of peaks.
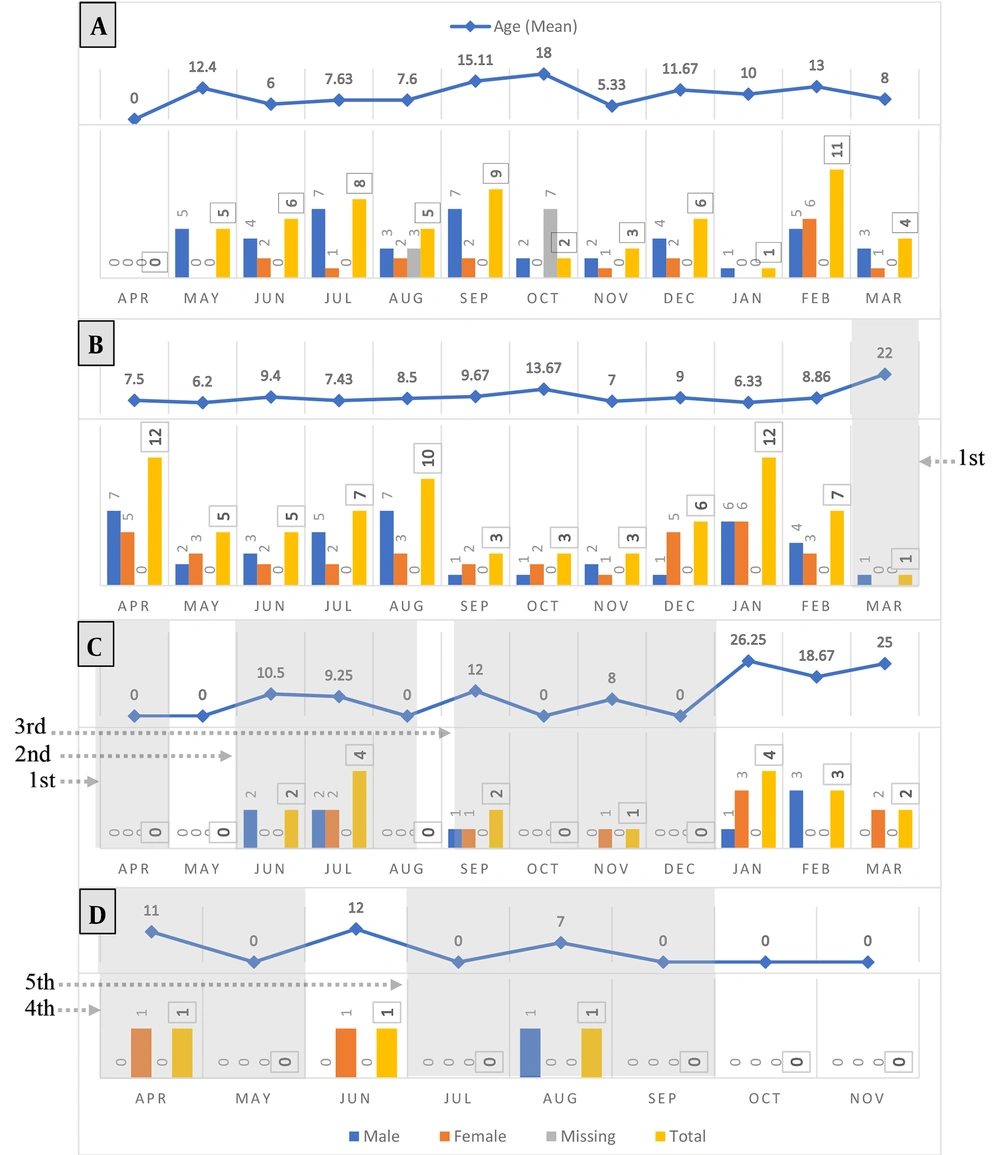
Monthly frequency of age, gender, and number of operations for tonsillectomy based on 1st, 2nd, 3rd, and 4th years. (A: 1st year; B: 2nd year; C: 3rd year; D: 4th year). A and B are related to ‘before COVID-19', and C and D are related to 'during COVID-19’. Each gray highlighted area presents one peak that is shown by the arrow and the number of peaks.
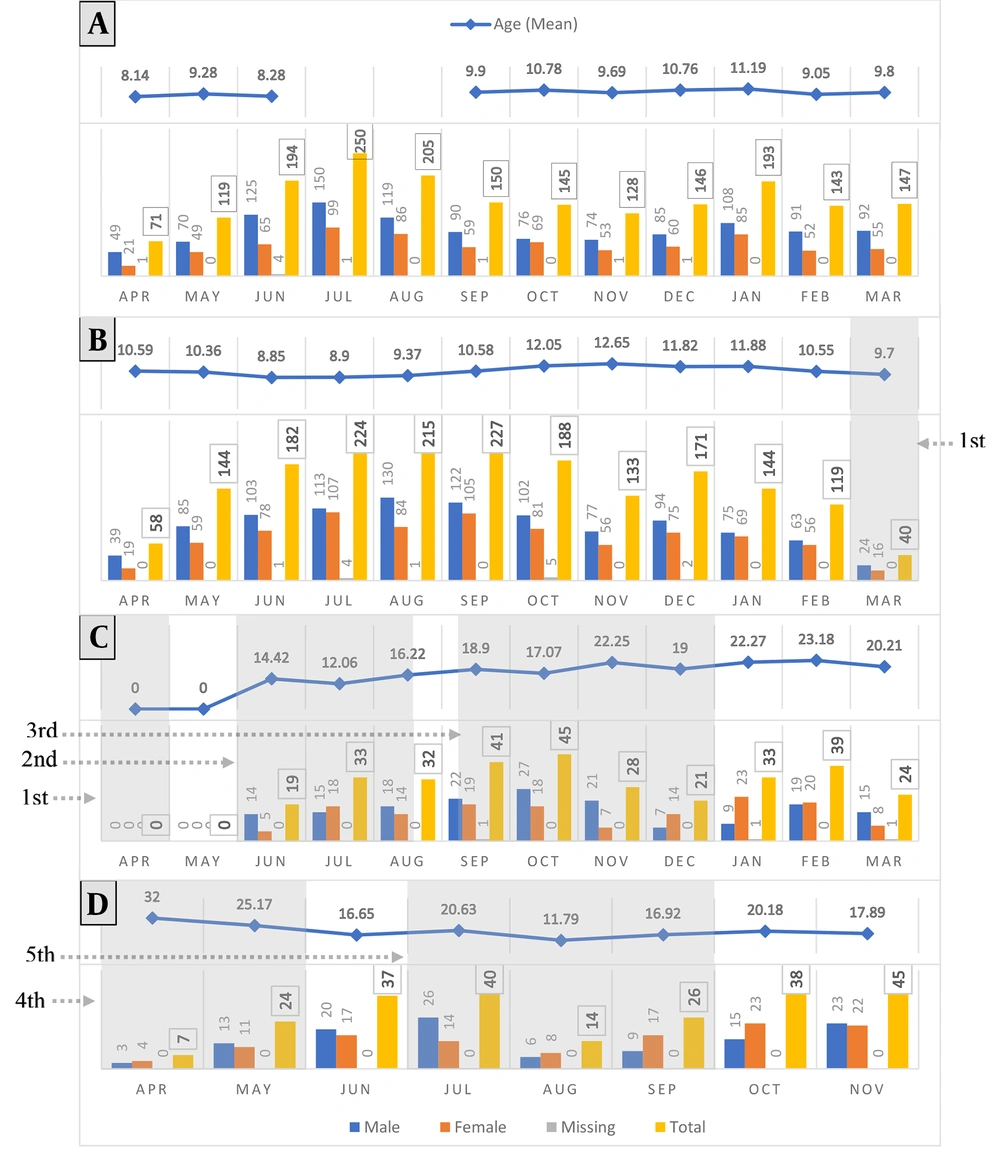
Monthly frequency of age, gender, and number of operations for oto-surgery based on 1st, 2nd, 3rd, and 4th years. (A: 1st year; B: 2nd year; C: 3rd year; D: 4th year). A and B are related to ‘before COVID-19', and C and D are related to 'during COVID-19’. Each gray highlighted area presents one peak that is shown by the arrow and the number of peaks.
The total number of each operation in each month, within March 21, 2018, to November 22, 2021, is shown in Figure 4, and the effect of each peak on the number of operations in comparison to before the COVID-19 pandemic can be observed. Additionally, the comparison of each peak to the past same months of a year was performed, and it showed a significant difference in terms of the total number of operations (P < 0.001).
5. Discussion
In March 2020, the Iran government ordered a strict lockdown in reaction to the COVID-19 pandemic. A major disruption was made by the COVID-19 pandemic in different aspects, especially in routine hospital services all over the world (9). In the interests of patient support and safety, elective surgery decreased during this pandemic (10, 11). In otolaryngology, similar to other specialties, government protocol restricted surgery to emergencies (12). It is noteworthy to mention that TO and AD are considered elective surgeries (13).
The current study is the first one to evaluate the incidence rates of tonsillectomy, adenoidectomy, and ear surgeries before and during the COVID-19 pandemic in Iran. The results showed a significant reduction in surgery rates of TO, AD, and oto-surgery. However, there is no related study in Iran. Nevertheless, several studies all over the world have reported this significant issue (8, 13, 14).
Those types of oto-surgeries that were not directly affected by COVID-19 were enrolled. It means it can be considered a control group. It is noteworthy to mention that the amount of this reduction was much more in TO and AD than in oto-surgery (control group). Additionally, this difference is observed in various months during the pandemic in the current study figures. It is known that the rate of all types of surgeries had a fall (15) due to different factors, such as patients’ anxiety, lockdown, and government protocol about the cancellation of elective surgery (16, 17). However, all of these factors affected all types of operation approximately the same. Therefore, "Why did the amount of reduction differ between AD and TO ones and oto-surgery?" is the main question.
Additionally, previous studies did not report any theory that can exactly explain why TO and AD differed (13). It could be due to the one main reason for the tonsil and adenoid glands’ infection. Most surgical indications of tonsillectomy and adenoidectomy are directly due to the infection, such as recurrent tonsillitis, adenoiditis, otitis media, and abscess. Furthermore, most of the rest of the indications are indirectly related to the infection, such as obstructive sleep apnea (OSA) due to adenotonsillar hypertrophy and sinusitis (18). This finding means that infection plays a key role in rates of TO and AD.
The infection rates that cause tonsilitis and adenoiditis have decreased during the COVID-19 pandemic. This could be the result of wearing masks, the closure of schools, and social distancing during the pandemic. It means that these factors filtered different viruses entering, such as viruses that are related to tonsilitis and adenoiditis plus the COVID-19 virus. Following this, the rates of TO and AD probably decreased during the pandemic. On the other hand, tonsils and adenoids are lymphoid structures, and there is an equilibrium between the local immunologic response of adenotonsillar tissue and their normal flora. Acute viral infection or its colonization can disrupt this equilibrium and finally lead to hypertrophied lymphoid tissue (adenotonsillar hypertrophy) (19).
As mentioned previously, adenotonsillar hypertrophy can result in OSA as one of the surgical indications of tonsillectomy and adenoidectomy. Therefore, exposure to viruses can be reduced by wearing masks among many infected individuals during the pandemic. Following this, the risk of adenotonsillar hypertrophy decreased during the pandemic, and the rates of TO and AD were reduced. Some studies reported a reduction in the transmission of pediatric viral infections, such as otitis media (20) and tonsilitis (21). Moreover, their findings support the current study but are not certain.
The findings of the present study revealed that all operations were reduced to near zero in the first peak. It was due to the public stress and heavy restrictions at the beginning of the pandemic. However, in the second and fifth peaks, the number of TO and AD was less than in the current control group. It could be the result of the season. In Iran, that season is summer, and schools are closed, and physical interaction is very low for children. This issue highlights the present study hypothesis. In addition, the findings of Alde M. et al.’s study support it (20). However, its sample size is too smaller than the present study.
Generally, the rates of TO and AD dramatically declined during the peaks. In the third peak, the number of TO increased due to the nature of the season, and there was a cold atmosphere in Iran in autumn. Following this, the rates of upper airway infections were upwards. Again, in the 4th peak, a decrease occurred for all operations. However, it was more for TO and AD than the control group. It could be due to the virtual teaching of schools for children. Additionally, the months of the 4th peak are the best time for traveling in Iran. Therefore, many families traveled to different provinces, and the physical interaction was reduced.
The current study did not have any limitations except for some missing information about patients. It is suggested that future studies should be conducted on the pathophysiology of the present study hypothesis. Additionally, further studies could be better performed as clinical trials.
5.1. Conclusions
To sum up, the findings of the current study presented that the rates of TO, AD, and oto-surgery decreased significantly during the COVID-19 pandemic. However, this reduction was much more for TO and AD in comparison to oto-surgery. This difference proposes a hypothesis of the “impact of restrictions during the pandemic on the transmission of tonsillar and adenoidal glands infection among pediatric patients”.