1. Introduction
Classical whooping cough infection primarily affects unvaccinated children aged 1 - 10 years. The illness can last 6 - 12 weeks or longer. The severity of pertussis infection is influenced by factors such as the patient's age, previous vaccination history, prior infection, the presence of passively acquired antibodies, and antibiotic treatment. The incubation period for whooping cough is between 5 - 21 days after exposure. Transmission is nearly 100% among individuals exposed to aerosol droplets at close range. Long-term carriage of the infection has not been demonstrated (1, 2).
Globally, there are approximately 50 million pertussis infections annually, leading to 300,000 deaths. The mortality rate in infants is 4% (2-4). Since 2009, the pertussis vaccine has been included in the routine vaccination schedule of the Ministry of Health (5).
In children, pertussis should be suspected if coughing persists and intensifies over 7 - 10 days, presenting stubbornly in the form of paroxysms. Pertussis infection should be considered in cases of apnea, cyanosis, or acute respiratory failure in infants under three months of age (6). A study conducted in France reported that 13% of deaths due to bacterial infections were related to pertussis (7). Additionally, there are publications indicating that whooping cough causes serious infections and necessitates intensive care hospitalization in our country (8).
Treatment for infants includes hydration, oxygen support, and mechanical ventilation as needed. Adequate nutrition and caloric intake should be provided. It is also important to address secondary bacterial infections and any complications that may arise (9). Pertussis treatment involves administering azithromycin (5 days) or clarithromycin (7 - 10 days) at an age-appropriate dose (10).
Leukocyte counts above 50,000 cells/μL due to causes other than bone marrow issues are referred to as leukemoid reactions (11). A leukemoid reaction is a clinical syndrome in which changes similar to those found in leukemia are observed in peripheral blood, although leukemic disease is not present (12). Leukemoid reactions can be caused by conditions such as pneumonic infections and inflammation, as well as chronic infections like infectious mononucleosis, malaria, and tuberculosis, some types of cancer such as Hodgkin's disease, and autoimmune anemia (13).
Studies suggest that leukemoid reactions are associated with increased cytokine production. Cytokines involved in leukemoid reactions include granulocyte-macrophage colony-stimulating factor (CSF), granulocyte-CSF (G-CSF), interleukin-3 (IL-3), and IL-6 (14).
Hyperleukocytosis can lead to congestion in the intracranial and pulmonary circulation. Due to hyperviscosity, white cells may occlude small vessels, resulting in slowed circulation, ischemia, acidosis, hypoglycemia, bleeding, and potentially death. Clinical findings depend on the system affected by hyperleukocytosis. Thrombi may impact the central nervous system, kidneys, adrenal glands, cardiopulmonary system, and gastrointestinal system (15, 16).
Rapid fluid replacement is crucial in treating a leukemoid reaction. Studies have demonstrated that fluid loading, urine alkalization, and allopurinol treatment can reduce white blood cell counts in patients with leukemia when the count exceeds 100,000 cells/μL. Early in treatment, blood transfusions and diuretics that increase blood viscosity should be avoided (16, 17). In severe symptomatic cases, leukapheresis and exchange transfusions may offer temporary reduction in white blood cell count (15-17).
This case report aims to present hyperleukocytosis in an infant with pertussis infection and the outcomes of partial exchange transfusion treatment.
2. Case Presentation
A 41-day-old female patient presented to the health center with a cough lasting five days, along with fever and wheezing for the past two days. On examination, the patient had a fever of 37.8°C, a heart rate of 144/min, tachypnea, and intercostal retractions (ICR), leading to her hospitalization in the pediatric intensive care unit (PICU). Her oxygen saturation was 82% without oxygen and 94% with a non-rebreathing mask. Given a prediagnosis of pneumonia, treatment with meropenem, vancomycin, and hydration was initiated. Laboratory results on admission showed a pH of 7.40, PCO2 of 40.31 mmHg, PO2 of 94.8 mmHg, hemoglobin of 12.9 g/dL, white blood cell (WBC) count of 22,550 cells/μL, platelet (PLT) count of 718,000 cells/μL, lactate dehydrogenase (LDH) of 493 U/L, and C-reactive protein (CRP) of 59.3 mg/L (Table 1). Bordetella pertussis PCR was positive for the patient, who had a nasopharyngeal aspirate sample taken. After 48 hours of hospitalization, the patient’s general condition deteriorated, and she developed respiratory failure, leading to intubation and connection to a mechanical ventilator (MV). At this time, a follow-up hemogram revealed a WBC count of 67,290 cells/μL, and the patient was transferred to our 3rd level PICU.
| Varibales | 1 Day | 4 Days | After PE | 7 Days | 11 Days |
|---|---|---|---|---|---|
| WBC (1000 cells/μL) | 98.18 | 144.31 | 77.32 | 68.86 | 56.3 |
| Haemoglobin (g/dL) | 10.1 | 9.5 | 10.8 | 10.2 | 9.3 |
| Platelet (1000 cells/μL) | 949 | 509 | 318 | 486 | 419 |
| CRP (mg/L) | 61.4 | 44.6 | 63.8 | 21.6 | 38.4 |
| Procalcitonin (ng/mL) | 1.6 | - | - | - | - |
| LDH (U/L) | 524 | 456 | 1136 | 943 | 931 |
| pH | 7.07 | 7.47 | 7.49 | 7.52 | 7.33 |
| PCO2 (mmHg) | 94 | 62 | 65 | 59 | 77 |
| HCO3 (mmol/L) | 27.2 | 29.6 | 39.3 | 42.1 | 45.5 |
| Ddimer (ng/mL) | 1890 | 2471.05 | - | 1119.96 | - |
| Ferritin (ng/mL) | 916.7 | - | - | - | - |
| Fibrinogen (mg/dL) | 396 | - | - | - | - |
| Triglyceride (mg/dL) | 203 | - | - | - | - |
| Uric acid (mg/dL) | 3 | - | - | - | - |
| Troponin I (ng/L) | 227.99 | 51.6 | - | - | - |
Blood Parameters
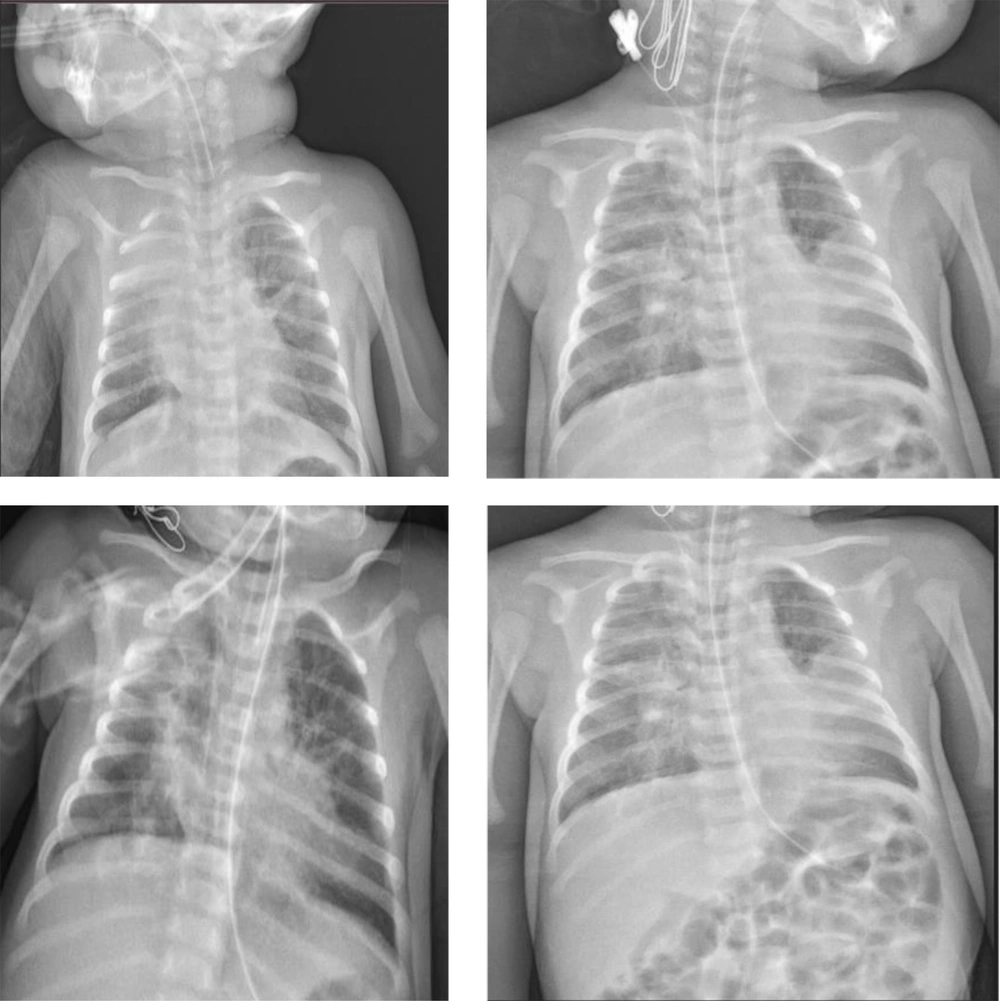
Upon admission to the PICU, the patient’s general condition was poor, she was intubated, and her consciousness was lethargic (she had been receiving sedation at the previous facility). The oropharynx appeared normal. Bilateral crepitant rales were present in the lungs. No organomegaly was observed, and other system examinations were unremarkable. The intubation tube was replaced and connected to the MV. Chest radiography revealed diffuse infiltrations (Figure 1). Treatment was adjusted with the addition of clarithromycin for pertussis and atypical bacterial infections, based on pediatric infectious disease consultation. Hydration was managed with 150 ml/kg/day of fluid.
Daily hemogram controls and routine tests were performed. Laboratory results from the blood samples taken during the patient’s clinical follow-up are shown in Table 1.
A peripheral smear performed after a WBC count of 98,180 cells/μL revealed 44% neutrophils, 32% lymphocytes, and 24% rods, with no atypical cells observed in the lymphocytes. In the peripheral smear, where platelets were within normal range, erythrocytes appeared normochrome and normocytic. A pediatric hematology specialist was consulted, and a leukomoid reaction was primarily considered. Continuation of antibiotherapy was recommended, and enoxaparin was started prophylactically due to the high D-dimer value.
On the fourth day of hospitalization, the patient's WBC count was 144,000 cells/μL, and partial exchange (PE) was planned. The patient underwent bone marrow aspiration followed by low-dose PE. After the PE, the patient's WBC count decreased to 77,320 cells/μL. Bone marrow examination showed no findings compatible with leukemia. The patient was extubated approximately 36 hours after the PE. On the 8th day of follow-up, the patient experienced two tonic-clonic convulsions lasting 3 minutes each. Levetiracetam was administered as a loading dose, followed by maintenance therapy. No further convulsions were observed.
The control hemogram showed a WBC count of 56,000 cells/μL. On the 11th day of hospitalization, the patient desaturated, had thick secretions, and exhibited intercostal retractions, leading to the initiation of high-flow nasal oxygen therapy. As respiratory distress increased and carbon dioxide retention was observed on control blood gas, the patient was re-intubated and connected to mechanical ventilation (MV). During follow-up, the patient suffered a cardiac arrest, did not respond to cardiopulmonary resuscitation, and was declared deceased.
3. Discussion
Unvaccinated children under 2 months of age diagnosed with whooping cough usually require hospitalization. While apnea and pneumonia are common, seizures, encephalopathy, and death are rare. As seen in our case, a leukomoid reaction may occur in whooping cough, which is one of the diseases causing severe pneumonia (18). Leukemia must be ruled out when a leukomoid reaction is present. In neutrophilic leukomoid reactions, the differential diagnosis should consider drugs, hemorrhage, infections, hypersensitivity syndrome, myeloid growth factors, malignancy, and splenectomy (19).
The patient was initially treated with meropenem and vancomycin, and clarithromycin was subsequently added for pertussis infection. The patient received hydration and MV support for respiratory failure. As the leukocyte count increased to over 140,000 cells/μL, PE was performed on the 4th day of hospitalization, resulting in a 46.4% decrease in white blood cell count. This decrease is consistent with the findings of Christakopoulos et al. (20).
In severe symptomatic cases, leukapheresis and exchange transfusions are thought to provide a transient reduction in white blood cell count. However, there is no evidence that these procedures reduce intracerebral and pulmonary complications (15-17).
The worsening of the clinical condition despite the timely initiation of appropriate antibiotherapy is associated with the fact that our patient was younger than 2 months old. This age factor may contribute to the development of a leukomoid reaction and hyperviscosity, which may worsen the clinical picture. Indeed, a study involving young children hospitalized in intensive care units in China found that 90.3% of the patients were younger than 6 months and 56.9% were younger than 3 months. Among 38 patients admitted to the intensive care unit (ICU), 13 died, resulting in a mortality rate of 34.2% from severe whooping cough; 76.9% of these deaths occurred in patients younger than 6 weeks (21).
The patient was weaned from MV approximately 36 hours after PE. The decrease in the leukocyte count to 77,320 cells/μL, despite the initial extremely high count of 144,000 cells/μL, suggests a transient improvement. Although partial recovery was achieved after PE, no further increase in the leukocyte count was observed in the following days despite the worsening of the patient’s clinical condition. Therefore, PE was not repeated. There is a need for new case reports to determine when to start PE treatment and how many cycles should be performed.